Modified volumetric modulated arc therapy technique with reduced planning and treatment time for craniospinal irradiation utilising two isocentres
Abstract
Introduction
Paediatric patients (individuals below 18 years of age) requiring cranial-spinal irradiation (CSI) at our institution are commonly planned and treated using a three isocentre (3-ISO) volumetric modulated arc therapy (VMAT) technique. A modified two isocentre (2-ISO) VMAT technique was investigated with the aim to improve workflow and reduce planning and treatment time.
Methods
Five CSI paediatric patients previously treated with a 3-ISO VMAT technique were retrospectively replanned using a 2-ISO VMAT technique. The 2-ISO VMAT plans were reviewed and approved by a radiation oncologist (RO) before undergoing patient-specific quality assurance (QA) procedures, performed by a radiation oncology medical physicist (ROMP). Planning target volume (PTV) coverage, organ-at-risk (OAR) dose as well as planning and treatment durations of the first five patients utilising 2-ISO technique were compared with 3-ISO technique.
Results
The average percentage difference in PTV coverage by 95% reference dose between the 2-ISO and 3-ISO is 0.14%, and the average difference in OAR median dose is 0.68 Gy. Conformity and homogeneity indices have the same averages at 1.18 and 0.4 respectively. Patient-specific physics QA results were all comparable with the 3-ISO averages at 98.84% and the 2-ISO at 98.71%. Planning duration for the 2-ISO was reduced by up to 75%, and daily treatment duration was reduced by up to 50%. Of all the previously treated CSI patients using a 3-ISO technique, 45% were suitable for the 2-ISO technique.
Conclusion
The 2-ISO VMAT technique provided comparable dose distribution based on PTV coverage, OAR dose and plan metric indices. Reduced planning and treatment duration with the 2-ISO technique facilitated improved workflow with decreased sedation time for paediatric patients requiring a general anaesthesia.
Introduction
Cranial-spinal irradiation (CSI) is a complex radiotherapy technique due to the need to irradiate the entire craniospinal axis for patients with high-risk cerebrospinal fluid involvement.1-11 The planning target volume (PTV) extends from the vertex of the skull to the sacral region, and fields are matched at the junction region, from the posterior skin surface to adequately cover and treat the entire PTV.1-3 Various publications have explored ways to use intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) to improve plan conformity and reduce dose to organ at risk (OAR) such as optic structures, brainstem, heart and kidneys.1-11
A three-dimensional conformal radiotherapy (3DCRT) technique was previously used at our institution for CSI treatments with the patient lying in the prone position. Due to its dependence on maintaining an exact dose match at the spinal cord level, there is a high risk of dose variation in the junction region with 3DCRT.1, 8 IMRT and VMAT provide the opportunity to optimise dose in the junction region using the same field overlap throughout the course of treatment.5, 6, 8 Given this and the desire to improve overall plan conformality, we developed and implemented a supine 3-ISO VMAT technique.
The supine three isocentre (3-ISO) VMAT technique was specifically developed for the paediatric cohort in our institution. This position allows easy access to oral cavity and airway when a general anaesthesia (GA) is required. Additionally, based on our clinical experience the supine position is more comfortable for most patients making the position easier to hold throughout treatment, and this reduces the risk of intra-fraction motion. In developing the supine VMAT technique, new stabilisation equipment was designed to accommodate the new beam geometry. Patient comfort, stability, reproducibility and setup accuracy were a focus in design process.
With the planning technique changing from 3DCRT to VMAT, we encountered many challenges including the time it took to generate a clinically acceptable plan and the time it took to accurately deliver a complex treatment involving multiple arcs. To improve the efficiencies for CSI planning and treatment utilising the VMAT technique, a two isocentre (2-ISO) VMAT technique was proposed.5, 9, 10 In this study, we compared the 2-ISO VMAT technique to the 3-ISO technique with respect to plan dosimetry, patient-specific quality assurance (QA), quality metric indices and the planning and treatment time.
Methods and Materials
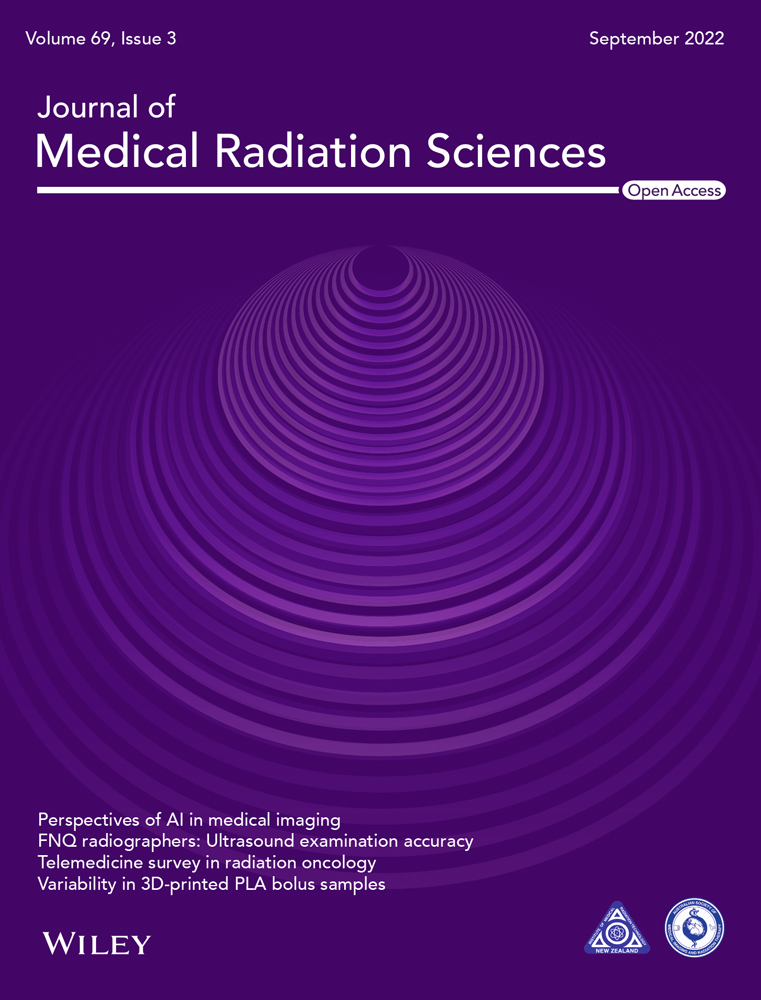
Ethics approval was obtained from Metro South Human Research Ethics Committee (HREC) prior to conducting the study. Five CSI paediatric patients previously treated using the 3-ISO VMAT technique were retrospectively planned using a 2-ISO VMAT technique. Four patients had a prescribed dose of 23.4 Gy in 13 fractions, and one had a prescribed dose of 36 Gy in 20 fractions. During their simulation session, patients were positioned supine on a Portrait carbon fibre board (Qfix, Avondale, AZ, USA) and supported by a whole-body CSI Vac-Lok bag (CIVCO Radiotherapy, Orange City, IA, USA). The patient's head and shoulders were immobilised using an S-Frame thermoplastic shell (CIVCO Radiotherapy) with arms resting on the Vac-Lok bag and raised slightly anterior to the spine. The knees were supported by a knee bolster (CIVCO Radiotherapy) (Fig. 1).
All patients planning computed tomography (CT) scans were acquired on a 20-slice SOMATOM Definition AS scanner (Siemens Healthcare GmbH, Erlangen, Germany). Patients were scanned from the skull vertex to the ischial tuberosities with 2-mm slice thickness. High definition scans from the skull vertex to base were also acquired at 0.6-mm slice thickness to assist with OAR contouring purposes. The two CT data sets were exported and registered in the Pinnacle3 treatment planning system, v16 (Philips Healthcare, Eindhoven, Netherlands), with the high definition scans the secondary data set. A dose grid size of 0.25 cm × 0.25 cm × 0.25 cm and collapsed cone convolution algorithm were used for all plans. All patients were treated with 6- mega voltage (MV) photon beams, on a Clinac iX (Varian Medical Systems, Palo Alto, CA, USA), with 120 multileaf collimators (MLC) and an image-guided radiation therapy (IGRT) couch.
3-ISO technique planning and treatment
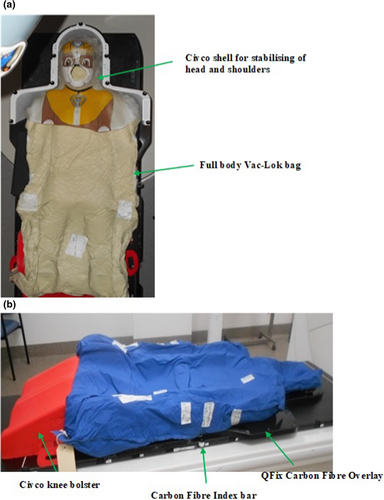
The clinically treated 3-ISO VMAT plans had one isocentre placed in the skull region, the second and third isocentres were placed in the thoracic and lumbar spine region respectively. The 3-ISO plan consisted of three full arcs to the skull, two partial arcs to the upper spine and two partial arcs to the lower spine. Two junction regions with a minimum field overlap length of 3 cm were used to smooth the dose between adjacent fields.11 The 3 arcs to the skull had collimator angles of 275° (one arc) and 5° (two arcs). Field widths were set to cover the PTV at every angle, and field lengths were set to cover from the vertex to just above the shoulders. The four partial arcs used in the spinal region had collimator angles of 355° (upper spine arcs) and 5° (lower spine arcs). The widths of the spine arcs were set to cover the PTV and their lengths were set to overlap adjacent fields by 3 cm. Inferiorly, the spine arcs cover the PTV (Fig. 2a). Arc angles were 181° to 253° and 107° to179° for the upper spine and 179° to 107° and 253° to 181° for the lower spine (Fig. 2c). These angles were chosen to avoid dose to anterior structures, such as the heart, lungs, sternum, breast tissues and arms, and are similar to those reported as optimal by Pollul et al.11 Arc directions were selected to reduce beam off time between arcs and to improve efficiency of treatment delivery.
2-ISO technique development and evaluation
For the retrospectively generated 2-ISO VMAT plans for each of the five patients, the upper isocentre (ISO UPR) was placed in the upper thoracic region and the lower isocentre (ISO LWR) was placed in the abdominal region (Fig. 2b). Four partial arcs were used to treat the skull and upper thoracic region and were attached to the ISO UPR point (Fig. 2c). The arc angles were 179° to 107°, 107° to 253°, 253° to 181° and 253° to 107°. Collimator angles were 5° for the first three arcs and 275° for the fourth arc. Multiple partial arcs were utilised in the skull and upper thorax region to control dose to OAR such as optic structures and hippocampus. The lower thoracic and spinal region were treated using two partial arcs with the same gantry angles as the 3-ISO (Fig. 2c) to avoid anterior structures such as heart, lungs, breast tissues and arms. Spinal arcs were attached to the ISO LWR point with superior field borders set to overlap the upper arcs with 3 cm and the inferior borders set to cover the PTV. Our decision to set a minimum overlap region of 3 cm is consistent with other studies where the overlap region varies between 2 and 4 cm to reduce sensitivity for uncertainties.11
Each of the retrospectively generated 2-ISO plans were performed by one radiation therapist (RT) using the same prescribed dose, number of fractions, OAR dose tolerances and objectives as the 3-ISO VMAT technique. The optimisation method and objective values used were consistent between the two techniques to minimise process variations. Scripts were used to generate all standard items such as regions of interest (ROI), points, arcs, prescriptions, plan objectives and Pinnacle3 scorecards. Minor adjustments were made to dose controlling ROIs used in plan objectives to customise individual patient plans. All plans were normalised to achieve PTV coverage of 95% prescribed dose.
All retrospectively generated 2-ISO VMAT plans were reviewed and approved by one radiation oncologist (RO) as per departmental protocol, adapted from St Jude Children's Research Hospital guideline ‘A Clinical and Molecular Risk-Directed Therapy for Newly Diagnosed Medulloblastoma’ SJMB12 activated on 10 October 2013. PTV coverage and OAR doses were analysed and compared using dose volume histogram (DVH) analysis and Pinnacle3 scorecard data. Prescribing and reporting of doses for PTV and OAR are summarised in Table 1. Total MU in the cranial and spinal regions were also compared.
| Target volume | Craniospinal prescription | Primary site prescription | Required coverage |
|---|---|---|---|
| Low risk | 15 Gy | 51 Gy | 95% RD–100% PTV |
| ¶Standard risk | 23.4 Gy | 54 Gy | 95% RD–100% PTV |
| *High risk | 36–39.6 Gy | 54 Gy | 95% RD–100% PTV |
| Structures/OAR dose constraints | |||
| Brainstem |
¶<24.6 Gy (105%) *<37.8 Gy (105%) |
Max <54 Gy or D50 < 61 Gy D10 < 63 Gy |
|
| Spinal cord |
¶<24.6 Gy (105%) Ideal (22.2–23.4 Gy) *≤37.8 Gy (105%) |
Max <45 Gy or D50 < 26 Gy D10 < 57 Gy |
|
| Optic globes |
¶≤24.6 Gy (105%) Ideal <18 Gy *≤37.8 Gy (105%) |
Max <50 Gy or D50 < 10 Gy D10 < 35 Gy |
|
| Optic nerves & chiasm |
¶<24.6 Gy (105%) *<37.8 Gy (105%) |
Max <54 Gy or D50 < 54 Gy D10 < 56 Gy |
|
| Cochleae RT & LT |
¶≤23 Gy (98%) *<35.3 Gy |
<54 Gy D50 < 35 Gy |
|
| Lens RT & LT |
¶≤5 Gy (PRV < 12 Gy) *≤8 Gy (PRV < 18.5 Gy) |
≤8 Gy | |
| Heart |
¶D90 < 5 Gy D50 < 6 Gy D10 < 9 Gy Max 12 Gy *D90 < 5 Gy D50 < 10 Gy D10 < 15 Gy Max 18.5 Gy |
||
| Lung RT & LT |
¶Mean Dose ≤8 Gy *Mean ≤ 12.3 Gy |
||
| Kidney RT & LT |
¶Mean Dose ≤6 Gy *Mean ≤ 10 Gy |
||
| Liver |
¶D90 < 3 Gy D50 < 6 Gy D10 < 9 Gy *D90 < 4 Gy D50 < 10 Gy D10 < 15 Gy |
||
- Dx, dose at x percentage; OAR, organ at risk; PTV, planning target volume; RD, reference dose.
Plan quality metrics including conformity index (CI) and homogeneity index (HI) were used to quantify plan quality. Conformity index is generally defined as the ratio of the total volume enclosed by x% of the prescribed dose to the volume of the PTV enclosed by x% of the prescribed dose. Dzierma et al. describes CI = (VptvPD/VPTV × VPD)2 where VptvPD = volume of PTV enclosed by x% of prescribed dose, VPTV = total volume of PTV, VPD = total volume of prescribed dose.12 The HI plan metric assesses the variation of radiation received by the PTV and commonly serves as a measure of dose homogeneity within the PTV volume. There are many variations for HI, however, according to Dzierma et al. HI = PTVmax – PTVmin/ PTVmean where PTVmax = max dose in PTV, PTVmin = min dose in PTV and PTV mean = PTV mean dose.12
The clinically acceptable 2-ISO VMAT plan for each patient underwent patient-specific QA procedures to ensure beams were deliverable and met the department's pass criteria. This was performed by one radiation oncology medical physicist (ROMP) using an aS 1000 Portal Vision Electronic Portal Imaging Device (EPID) panel (Varian Medical Systems) and EPIDQA software v4.3.4 (Epidos, Bratislavia, Slovakia) with gamma analysis 3%/3 mm and accuracy above 90% as the pass criteria. Note a maximum jaw size of 17.5 cm (which equate to 35 cm at the EPID distance) when using the EPID and EPIQA software.
2-ISO technique clinical implementation evaluation
After the successful investigation of the 2-ISO VMAT technique on five retrospective CSI plans, a protocol for the 2-ISO VMAT technique was developed and implemented for clinical use. Five paediatric patients, with suitable PTV lengths of equal or less than 65 cm, were subsequently prospectively planned and treated using the 2-ISO VMAT technique. To evaluate the efficacy of the 2-ISO technique as a replacement for the 3-ISO technique, the time it took to generate a clinically acceptable plan and the treatment duration of these five patients were recorded for comparison with the 3-ISO VMAT technique.
Time taken to deliver the treatment with the 3-ISO VMAT technique was retrospectively obtained using time stamps of the first verification image and the last treatment field as recorded by the record and verify (RV) system. To ensure consistent time comparison with the 3-ISO technique the same time stamp information was collected for the 2-ISO technique.
The first five patients treated with 2-ISO technique also had a time-in-motion survey completed by the RT on the treatment units. Time was recorded from when patient first entered the treatment room to when the patient left the room. Re-setups and/or required extra imaging were also recorded. The data collected were used to determine CSI treatment time allocation at our institution.
To compare planning duration between the two techniques, the time it took to complete each optimisation for each technique for each patient was used. Note the optimisation process was kept to 40 iterations. This method was chosen as it provided an accurate comparison that is independent of the number of optimisations performed by an RT. While the overall planning processes involve PTV and OAR contouring, this time was omitted when comparing between the two techniques due to variable patient-specific factors influencing the time taken to complete this step.
The IBM SPSS statistics software, version 23 (Armonk, NY, USA), was used to analyse the treatment time difference between the two techniques. The mean treatment time for each technique and their standard deviations were determined, and a non-paired t-test was performed to determine whether the differences were statistically significant.
Image-guided radiation therapy protocol
IGRT is consistent for both techniques where kilovoltage (kV) orthogonal images were taken at each isocentre and the entire PTV volume is assessed prior to treatment. Cone-beam computed tomography (CBCT) was performed once a week at each isocentre to check for weight loss/gain. Translational couch shifts were applied based on image match from the upper/skull isocentre with 3-mm best fit match tolerance and 0-mm action level. Match points for the upper/skull isocentre were the bony skull with emphasis placed around optic structures. No rotational couch shift was applied. The orthogonal spinal images were used to confirm positional variation was within 5-mm tolerance. No independent moves were made based on image match from the spinal regions. If variations between the upper and lower orthogonal images exceeded 5 mm tolerance, a re-setup was required with the entire imaging sequence repeated.
This imaging guideline was developed to ensure distances between field edges and field isocentres remain the same and overlap region of 3 cm is enforced for treatment. An imaging flowchart was created for the 2-ISO VMAT technique (Supporting Information Fig. S1).
Results
2-ISO technique development and evaluation
Dosimetric comparison
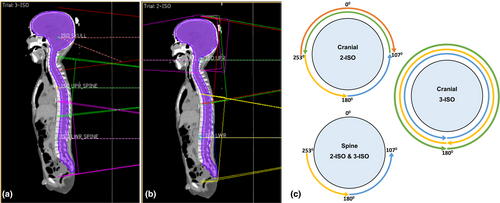
Dose distribution and percentage of PTV covered by 95% of reference dose (RD) were comparable for both techniques with the 2-ISO technique showing up to 0.4% higher PTV coverage (Fig. 3). Supporting Information, Table S1 compares coverage of PTV with 95% RD for the two techniques. Table 2 shows CI, HI and PTV mean all comparable between the two techniques with the average ± standard deviation almost identical for CI and HI. Most OAR doses (except optic structures) for the 2-ISO technique were slightly improved compared to the 3-ISO technique (Table 3). The median of the mean dose differences between the two techniques for the heart, right and left lungs and the liver were within 0.5 Gy, while the median of the mean dose differences for both kidneys and lenses range from 1.14 to 2.07 Gy. Using 3-ISO mean dose as reference, a value less than this for the 2-ISO will equate to a positive difference, while a value greater than this will equate to a negative difference. Table 3 shows the majority of OAR has a positive median value suggesting that the 2-ISO technique is comparable with the 3-ISO technique. Global maximum point doses for the entire plan were also similar between the 2 techniques with the magnitude of the difference within 0.5 Gy.
| Patients | Conformity Index (CI) | Homogeneity Index (HI) | PTV mean dose | Total MU (cranial region) | Total MU (spinal region) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | |
| 1 | 1.24 | 1.21 | 0.50 | 0.38 | 24.1 | 23.93 | 1011 | 600 | 427 | 232 |
| 2 | 1.14 | 1.16 | 0.49 | 0.47 | 35.61 | 36.37 | 731 | 607 | 421 | 233 |
| 3 | 1.18 | 1.17 | 0.29 | 0.28 | 23.6 | 23.55 | 385 | 519 | 412 | 246 |
| 4 | 1.16 | 1.18 | 0.65 | 0.64 | 24.03 | 24.08 | 444 | 496 | 562 | 272 |
| 5 | 1.17 | 1.19 | 0.24 | 0.22 | 23.52 | 23.56 | 388 | 588 | 427 | 276 |
| Average ± σ | 1.18 ± 0.04 | 1.18 ± 0.02 | 0.4 ± 0.2 | 0.4 ± 0.2 | n/a | n/a | Total average ± σ |
3 ISO: 1041 ± 265 2-ISO: 814 ± 45 |
||
- MU, monitor units; PTV, planning target volume; σ, standard deviation.
| OAR | Mean dose (Gy) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Difference | ||||||
| 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | 3-ISO | 2-ISO | Median (range) | |
| RT lens | 4.96 | 4.80 | 7.64 | 7.50 | 7.42 | 5.35 | 7.60 | 5.16 | 11.27 | 6.41 | 2.07 (0.14–4.86) |
| LT lens | 4.85 | 4.91 | 7.55 | 7.43 | 7.58 | 5.87 | 7.57 | 5.02 | 10.69 | 6.82 | 1.71 (−0.06–3.87) |
| Heart | 6.40 | 6.72 | 6.53 | 7.08 | 6.19 | 5.09 | 6.40 | 5.36 | 4.96 | 5.04 | −0.08 (−0.55–1.1) |
| RT lung | 7.17 | 6.99 | 9.44 | 11.46 | 6.93 | 7.28 | 7.97 | 7.33 | 7.34 | 7.08 | 0.18 (−2.02–0.64) |
| LT lung | 6.42 | 5.98 | 9.91 | 9.48 | 6.94 | 6.33 | 6.12 | 5.59 | 7.01 | 6.98 | 0.44 (0.03–0.61) |
| Liver | 5.49 | 4.83 | 7.25 | 6.8 | 5.59 | 5.49 | 4.97 | 5.39 | 5.82 | 5.38 | 0.44 (−0.42–0.66) |
| RT kidney | 6.66 | 4.97 | 15.41 | 9.26 | 6.51 | 5.37 | 5.03 | 5.19 | 5.65 | 5.01 | 1.14 (−0.16–6.15) |
| LT kidney | 6.59 | 4.97 | 14.56 | 9.12 | 6.55 | 5.18 | 5.02 | 5.20 | 5.64 | 5.02 | 1.37 (−0.18–5.44) |
| RT Hippocampus | 24.41 | 24.09 | 32.31 | 31.39 | 23.61 | 23.51 | 24.33 | 23.21 | 23.05 | 23.40 | 0.32 (−0.35–1.12) |
| LT Hippocampus | 24.73 | 23.55 | 32.27 | 31.92 | 23.66 | 23.47 | 23.63 | 23.25 | 23.23 | 23.51 | 0.35 (−0.28–1.18) |
| Optic Chiasm | 23.94 | 24.35 | 34.99 | 35.7 | 23.73 | 23.13 | 23.57 | 24.37 | 24.06 | 23.4 | −0.41 (−0.80–0.66) |
| RT Optic Nerve | 22.96 | 23.78 | 33.3 | 33.54 | 22.55 | 21.31 | 24.03 | 24.55 | 23.96 | 24.05 | −0.24 (−0.82–1.24) |
| LT Optic Nerve | 22.52 | 23.71 | 31.75 | 32.43 | 22.47 | 21.99 | 24.05 | 23.88 | 23.87 | 23.98 | −0.11 (−1.19–0.48) |
- LT, left; OAR, organ at risk; RT, right. Positive differences between the two techniques equate to a lower OAR dose for the 2-ISO technique compared with the 3-ISO technique.
Patient-specific QA
Given clinical pass criteria for patient-specific QA for the gamma analysis is 90% within 3%/3 mm, both techniques showed comparable pass percentages with the differences clinically insignificant (Supporting Information, Table S2).
2-ISO technique clinical implementation evaluation
Due to the size of the EPID QA device required for patient-specific QA,13 maximum field length permissible per jaw is 17.5 cm. This field length limitation consequently imposes a PTV length limitation to ensure the 2-ISO technique will adequately cover the entire length of the PTV with 3 cm overlap. Patients with total PTV length of more than 65 cm did not qualify for the 2-ISO technique. Our records indicated even with this limitation, 45% of previously treated CSI patients using the 3-ISO technique were suitable for the 2-ISO VMAT technique.
Comparison of planning and treatment duration
Dosimetry time recorded from the five retrospective plans and five clinically treated plans using the 2-ISO VMAT technique showed time taken to generate a clinically acceptable plan was reduced by up to 75% compared with the 3-ISO technique. This time reduction calculation was based primarily on the faster optimisation time of 30 min for each optimisation with the 2-ISO technique compared to approximately 2 h required for the 3-ISO technique. Total treatment duration for the 2-ISO VMAT technique was on average completed within 17 min and the 3-ISO technique took close to 30 min to deliver the treatment. Table 4 shows the clinical significance of treatment time reduction in the 2-ISO technique (P-value = 0.006).
| Group | N | Mean time (min) | Std. deviation | Mean difference (min) | 95% Confidence interval of the difference | P-value | |
|---|---|---|---|---|---|---|---|
| 3-ISO | 65 | 24.50 | 4.38 | 9.63 | Lower | Upper | 0.006 |
| 2-ISO | 65 | 14.87 | 1.23 | 4.42 | 15.16 | ||
Discussion
While most CSI literature concentrated on dosimetric considerations of CSI, we report a novel approach of technique modification with the aim to improve planning and treatment efficiency. A review of recent literature showed that CSI treatment in the supine position using VMAT technique is the method of choice due to accessibility, stability, improved dose conformity and reduced OAR dose.1, 2, 5-8, 11, 13, 14 There are studies which mention treatment time differences between 3DCRT, IMRT and VMAT2, 15, 16 where all agreed VMAT would require longer treatment time. However, the literature ultimately concluded VMAT is the preferred method for CSI due to accuracy of treatment delivery and improve plan dosimetry with respect to PTV coverage and OAR doses.2, 15, 16
Dose in overlap region
With the initial development and implementation of the 3-ISO VMAT technique, the robustness of the technique with regards to positional error and its effects on dose in the overlapping junction area was tested and analysed by offsetting the spine isocentres in the anterior/posterior, right/left and superior/inferior directions to simulate positional errors. Studies performed by Strojnik et al. and Meyer et al. also used this method of assessment7, 15 with Strojnik et al. creating a linear ramp-like dose profiles in the overlap region to avoid dose discrepancies with minor positional errors.15 We believe our approach is more practical and better reflects the reality of the clinical settings as treatment setup was only repeated if positional errors resulted in unacceptable plan dosimetry variations. Acceptable dosimetry variation was determined by RO comparing the isocentre offset plan with the original plan for offsets of 1, 3, 5 and 7 mm. The RO deemed dosimetry variation with positional errors up to 5 mm was still acceptable provided this was in the spinal region. This decision is supported by Sarkar et al. where they reported that VMAT technique is insensitive to longitudinal setup errors because of the existence of low dose gradients at the junction between fields.4 Zhou et al. also reports that positional errors within 3 mm have little impact on dosimetry for VMAT CSI17 and Meyer et al. also concluded that accuracy will not be deteriorated when larger errors of >5 mm were simulated.7 The findings of these publications4, 7, 17 along with acceptable dose variation of up to 5 -mm positional errors supports our clinical decisions.
Treatment duration
Though our sample size of five patients is small, we used data collected from every fraction of each patient's treatment (13 fractions each) to obtain a total of 65 samples over five patients. Reduction in treatment duration for the 2-ISO technique was close to 50%, and this is due to the combination of reduced number of isocentre from three to two, treatment arcs from seven to six and verification images from six to four. It is important to clarify that although the 2-ISO technique has less control points due to modification of arc geometry, this does not always translate to less monitor units (MU) for the cranial region (Table 2). MU in the cranial region is greater for the 2-ISO technique due to increased modulation to achieve PTV coverage. For patients 3–5, who were older compared with patients 1 and 2, this increased modulation, in combination with different arc geometry and larger distances between PTV and lenses, have resulted in improved lens doses for the 2-ISO technique.
Despite this, the average total MU per fraction for the 2-ISO is less compared with the 3-ISO thus contributing to overall reduced treatment duration.
We were able to reduce imaging time by reducing the number of kV images from six to four and reducing the number of CBCT from three to two per week. We chose kV as our daily imaging modality due to quicker acquisition time and smaller dose delivered of 0.114 mGy compared to 2.7 mGy for CBCT (measured by our medical physicists on Varian Clinac iX). Weekly image dose reduction for the 2-ISO is 3.27 mGy (2.7: CBCT plus 0.114 × 5: KV) which is small but worth mentioning.
Treatment time allocated for the 3-ISO technique at our institution is 45 min to 1 h and for the 2-ISO technique it is 30–45 min. Our experience to date confirms these treatment times as appropriate.
Planning duration
While plan complexities are the same for both techniques with similar objectives used, time taken to plan a 2-ISO technique was considerably reduced as the number of control points used were reduced from 681 to 358 due to 2-ISO skull arcs being partial arcs and the junctions were reduced from two to one. The overall decrease in number of control points and junction regions has contributed to considerably faster optimisation time as well as treatment duration. Modifications to existing scripts were made for the 2-ISO technique has improved overall efficiency for the planning process. We noted that as planning experience for the CSI technique developed among RTs, plans were generated faster and this is noticed for the five clinical plans using the 2-ISO technique.
Patient-specific QA
As mentioned previously, the limitations of the 2-ISO technique are the maximum field lengths of 17.5 cm permissible for planning and therefore patient size suitable for this technique. This is primarily because of known overresponse of the EPID diode detectors off-axis caused by beam softening which contributes to the uncertainty of dose measurement for any jaws set at 19 cm. It is possible however to increase the maximum field length from 17.5 cm to 19 cm per jaw if patient-specific QA can be conducted with a device that does not exhibit off-axis overresponse and still allow for a total measuring length of 38 cm with a high spatial resolution. This would mean 75% of previously treated CSI patients (adults and paediatrics) would qualify for the 2-ISO VMAT technique. It is important to mention that although the 2-ISO technique has a 50% time reduction for planning and treatment, this new technique does not supersede the 3-ISO technique when field lengths >17.5 cm are required.
Future Directions
We are looking to incorporate the use of six-degrees-of-freedom (6DoF) couch for CSI IGRT to improve treatment accuracy. As Li et al. outlined in their study, using daily CBCT at each isocentre with 6DoF couch applied immediately before treatment will reduce time and risk of intra-fraction motion.16 Their study showed dose gradient in the overlap region was still robust with 3° rotational tolerance and 3-mm translational tolerance.
Conclusion
The 2-ISO VMAT technique presented in this study is an alternative technique for 3-ISO when PTV length is less than 65 cm. Plan quality metrics for the 2-ISO technique is comparable with the 3-ISO with respect to PTV coverage by 95% of prescribed dose, OAR dose, CI, HI and patient-specific QA. With the reduction in planning and treatment duration by 75% and 50%, respectively, the 2-ISO technique can potentially enhance treatment accuracy with reduced GA sedation time. Overall productivity and efficiency within our department have improved significantly.
Acknowledgement
The authors acknowledge Kevin Nguyen and Alison Jenkins for their insight and technical support.
Conflicts of Interest
The authors declare no conflict of interest.
Ethical Statement
Ethics approval was obtained from Metro South Human Research Ethics Committee (LNR/2018/QMS/48148) prior to conducting the study.