New fractionations in breast cancer: a dosimetric study of 3D-CRT versus VMAT
Abstract
Introduction
Adjuvant radiation therapy (RT) following primary surgery in women affected by early breast cancer (EBC) plays a central role in reducing local recurrences and overall mortality. The FAST-FORWARD trial recently demonstrated that 1-week hypofractionated adjuvant RT is not inferior to the standard schedule in terms of local relapse, cosmetic outcomes and toxicity. The aim of this in silico study was to evaluate the dosimetric aspects of a 1-week RT course, administered through volumetric modulated arc therapy (VMAT), compared with traditional three-dimensional conformal radiation therapy (3D-CRT) with tangential fields.
Methods
Patients affected by left-side EBC undergoing adjuvant RT were selected. ESTRO guidelines for the clinical target volume (CTV) delineation and FAST-FORWARD protocol for CTV to planning target volume (PTV) margin definition were followed. Total prescribed dose was 26 Gy in five fractions. The homogeneity index (HI) and the global conformity index (GCI) were taken into account for planning and dose distribution optimisation purposes. Both 3D-CRT tangential fields and VMAT plans were generated for each patient.
Results
The analysis included 21 patients. PTV coverage comparison between 3D-CRT and VMAT plans showed significant increases for GCI (P < 0.05) in VMAT technique; no statistically significant differences were observed regarding HI. For organs at risks (OAR), statistically significant increases were observed in terms of skin V103% (P < 0.002) and ipsilateral lung V30% (P < 0.05) with 3D-CRT and of heart V5% (P < 0.05) with VMAT technique.
Conclusions
This in silico study showed that both 3D-CRT and VMAT are dosimetrically feasible techniques in the framework of 1-week hypofractionated treatments for left EBC.
Introduction
Breast cancer is the most common malignancy in women, with about 276,480 new cases and 42,170 estimated deaths in 2020 worldwide.1 Main risk factors include the following: age, family history, genetic predisposition, history of precancerous lesions, reproductive factors, hormonal treatment, alcohol consumption, obesity (in postmenopausal phase) and previous irradiation.2
Early breast cancer (EBC) is defined as a disease not spread beyond the breast or the axillary lymph nodes. It represents approximately 70% of breast cancer presentations.3, 4
Radiation therapy (RT) plays a crucial role in EBC conservative therapeutic strategy, mainly in association with hormonal therapy.5, 6
The adjuvant treatment of EBC has been historically characterised by the administration of 50 Gy in 25 fractions of 2 Gy/day to the entire residual breast, followed by an additional boost of 10–16 Gy to the surgical bed on the basis of predictive prognostic factors and pathologic status of the margins.7
Several studies have investigated hypofractionated treatment schemes to reduce overall RT time, aiming to reduce treatment waiting lists and taking advantage of radiobiological dose equivalence.
These studies have shown that moderately hypofractionated treatment is effective and safe for the management of EBC.8-11
A recent systematic review and meta-analysis of randomised trials and a mono-institutional experience further demonstrated that hypofractionated RT in the early stages of the disease does not reduce local control, nor negatively impacts long-term cosmetic results. The risk of acute toxicity (i.e. radiodermatitis, oedema and pain) appears to be overall decreased, when compared to conventional RT.12, 13
Hypofractionated RT could therefore be considered a valid therapeutic alternative in the case of early-stage disease, with preferred dose prescriptions of 40 Gy in 15 or 42.5 Gy in 16 fractions.14-18
The recent FAST-FORWARD trial paves the way to new standards of care for EBC,19 taking full advantage of hypofractionation in this context. This phase III trial has indeed finally demonstrated that adjuvant breast RT delivered with 26 Gy in five fractions is non-inferior to the standard 3-week schedule in terms of 5-year ipsilateral breast tumour relapse incidence, patient-assessed normal tissue effects, clinician-assessed normal tissue effects and photographic change in breast appearance.19
Thanks to its logistic advantages, this hypofractionated treatment schedule has already been included in the International guidelines on RT for breast cancer during the COVID-19 pandemic.20 This is meant to reduce as much as possible patients’ exposure to healthcare environments and may represent a practice changing innovation for low-risk EBC patients candidate to adjuvant RT.20
Interestingly, traditional irradiation techniques were applied in the FAST-FORWARD trial, using whole-breast (WB) 3D conformal radiation therapy (3D-CRT) with tangential field arrangements.
In the case of inverse planned intensity modulated radiation therapy (IMRT), the authors only suggest the planner to seek advice of the quality assurance (QA) team, in order to ensure the best possible planning solution, but no specific dose constraints are suggested.19
In recent years, radiation oncologists have begun to use IMRT techniques for the adjuvant treatment of EBC, aiming to improve target coverage and cosmetic results, and reduce treatment-related toxicity.21-24
The aim of this in silico study was to evaluate the dosimetric aspects of the FAST-FORWARD 1-week WB RT course, administered with a standard volumetric modulated arc therapy (VMAT) technique, and to compare it with traditional irradiation techniques based on 3D-CRT tangential fields.
Materials and Methods
Patient selection
All the consecutive patients affected by left EBC undergoing adjuvant RT at the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, from March 2020 to April 2020, were retrospectively selected for this study. Patient selection was limited to left-side breast diseases in order to focus on heart dose.
Patients treated both in free breathing (FB) or deep inspiration breath hold (DIBH) were selected, according to clinical judgement based on age, compliance and the possible dosimetric advantage.
Patients affected by right or bilateral breast tumours or requiring nodal station irradiation were excluded from this analysis.
Patients enrolled signed a consent for data collection according to the study design requirements and Fondazione Policlinico Universitario Agostino Gemelli IRCCS ethical committee.
Treatment planning
Simulation was performed on a dedicated 16 slices CT scanner with 2.5-mm slice acquisitions (Optima CT580 W, HiSpeed DX/I Spiral; GE Healthcare, Chicago, Illinois). Gated CT images were acquired using a Cine CT respiratory protocol, and the respiratory waveform file was simultaneously recorded with an external real-time position management respiratory gating system (RPM) (Varian Medical Systems, Palo Alto, California). Patients set up included wing-board and feet-block repositioning systems.
- a 3D-CRT plan using tangential mediolateral and lateromedial fields and a maximum of three 15MV field in fields;
- a VMAT plan, using Photon Optimizer algorithm (v. 15.6) and only two partial 6MV photon arcs for DIBH treatments and three partial 6MV photon arcs for FB treatments, ranging from 310° to 165°. The collimator angles were set at 10° and 330° for the two arcs, and at 30° for the third arc, in order to reduce tongue and groove effect.
A 2.5-mm calculation grid was used in all the plans.
All the plans were optimised for a Varian TrueBeamTM linac equipped with Millennium 120 multileaf collimator (5 mm leaf width for the 20 cm central beam) (Varian Medical Systems, Palo Alto, CA).
The clinical target volume (CTV) was outlined according to the ESTRO guidelines.25
The CTV to planning target volume (PTV) margin was set at 10 mm, as proposed in the FAST-FORWARD protocol, cropping it at 5 mm from body surface.
Total prescribed dose was 26 Gy in five fractions of 5.2 Gy each, as in Brunt et al.19
Dose constraints for organs at risk (OAR) and upper and lower limits for PTV were applied as for suggested in the FAST-FORWARD protocol (Table 1).
| Mandatory | Optimal | |
|---|---|---|
| OAR | ||
| Ipsilateral lung | V30% ≤ 17% | V30% ≤ 15% |
| Heart | V25% ≤ 5% | |
| V5% ≤ 25% | ||
| PTV | ||
| Lower limit | V95% ≥ 90% | V95% ≥ 95% |
| Upper limit | V105% ≤ 7% | V105% ≤ 5% |
| V107% ≤ 2% | ||
| Dmax ≤ 110% | ||
Homogeneity index and global conformity index

The global conformity index (GCI) was also used in this study as an additional tool for the comparison of the different used planning techniques and to support the selection of the most appropriate treatment plan, taking into account both the irradiation of the target volume and the irradiation of the healthy tissues.27
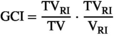
 represents the target volume covered by the reference isodose (95% of the prescription dose);
represents the target volume covered by the reference isodose (95% of the prescription dose);  is the target volume, and VRI is the volume of the reference isodose.
is the target volume, and VRI is the volume of the reference isodose.The ideal GCI value is 1 (GCI ≤ 1). If a GCI value >1 is observed, the treated volume is larger than PTV. On the other hand, when the GCI value is <1, the target volume is not completely covered.28, 29
Statistical analysis
Statistical Package for the Social Sciences (SPSS, IBM, US, Armonk) was used for statistical analysis. Statistical significance was considered if P < 0.05 after two-tailed Student’s t-test.
Results
Patient characteristics
This analysis included 21 patients affected by left EBC.
All patients were treated with conservative surgery and addressed to adjuvant RT.
A total of 10 patients (47.6%) were treated using DIBH technique; the remaining 11 (52.4%) underwent RT in FB conditions.
Patients’ characteristics are summarised in Table 2.
| ID | Age (years) | Gender | Stage | DIBH | Volume PTV (cc) |
|---|---|---|---|---|---|
| 1 | 44 | F | I | YES | 274.4 |
| 2 | 52 | F | I | YES | 457.3 |
| 3 | 54 | F | I | YES | 280.3 |
| 4 | 39 | F | I | YES | 326.6 |
| 5 | 50 | F | I | YES | 833.7 |
| 6 | 62 | F | I | YES | 615.8 |
| 7 | 46 | F | I | YES | 679.3 |
| 8 | 69 | F | II | YES | 777.2 |
| 9 | 61 | F | I | YES | 926.2 |
| 10 | 76 | F | I | YES | 942.7 |
| 11 | 68 | F | I | NO | 913.5 |
| 12 | 65 | F | I | NO | 682.4 |
| 13 | 54 | F | I | NO | 526.6 |
| 14 | 41 | F | I | NO | 371.4 |
| 15 | 77 | F | II | NO | 1618.9 |
| 16 | 63 | F | I | NO | 359.3 |
| 17 | 60 | F | I | NO | 278.9 |
| 18 | 79 | F | II | NO | 997.8 |
| 19 | 71 | F | I | NO | 1682.8 |
| 20 | 69 | F | I | NO | 776.2 |
| 21 | 50 | F | I | NO | 555.8 |
- All female patients with left-sided breast cancer; CTV = whole breast.
- PTV, planning target volume.
Dosimetric parameters: target coverage
The PTV coverage was compared for 3D-CRT and VMAT plans considering V95%, V105%, V107% and Dmax as dosimetric reference parameters (Figs 1 and 2).
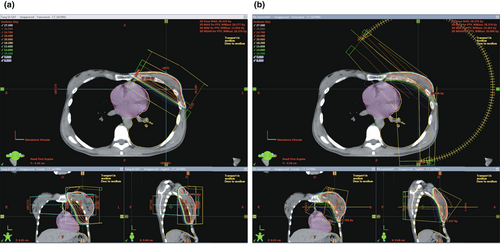
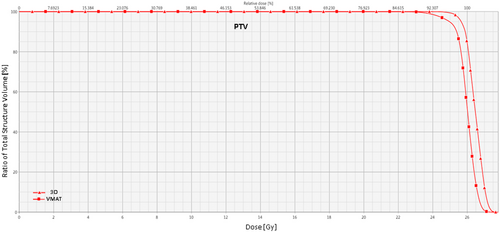
Significant differences between DVH mean values for 3D-CRT and VMAT plans have been observed.
The two-tailed t-test analysis showed significant increases for V95% (97.2% vs. 95.41%, P = 0.03), V105% (5% vs. 0.65% P < 0.05) and V107% (0.1% vs. 0.01%, P = 0.02) mean values in 3D-CRT plans with DIBH patients’ series.
No significant difference was found comparing Dmax mean values.
As for the FB patients series, significant increases in 3D-CRT plan were found for V95% (96.32% vs. 93.4%, P = 0.002) and V105% (5% vs. 0.86%, P < 0.05) mean values, while V107% and Dmax mean values did not show significant differences.
VMAT plans always showed a significant increase of GCI (0.9 vs. 0.6 for DIBH series and 0.89 vs. 0.63 for FB series, P < 0.05).
Diversely, no statistically significant differences regarding HI were observed.
All plans achieved optimal PTV coverage aims, except for the V95% of three cases of the 3D-CRT arm and eight cases of the VMAT arm.
The mandatory PTV coverage goal was not met only in a patient of the VMAT arm.
Table 3 summarises the dosimetric parameters of target coverage.
| PTV | GCI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| V95% | V105% | V107% | Dmax% | |||||||
| 3D | VMAT | 3D | VMAT | 3D | VMAT | 3D | VMAT | 3D | VMAT | |
Mean ± SD DIBH |
97.22 ± 2.22 | 95.41 ± 0.68 | 5 ± 0.0 | 0.65 ± 0.28 | 0.12 ± 0.14 | 0.01 ± 0.01 | 108.4 ± 0.82 | 108.8 ± 0.45 | 0.607 ± 0.06 | 0.909 ± 0.01 |
Mean ± SD FB |
96.32 ± 3.24 | 93.39 ± 3.18 | 5 ± 0.0 | 0.86 ± 0.77 | 0.11 ± 0.14 | 0.08 ± 0.16 | 108.7 ± 0.76 | 109.1 ± 0.73 | 0.627 ± 0.07 | 0.889 ± 0.03 |
| Two-tailed paired t-test | ||||||||||
| P DIBH | 0.03 | 0.000 | 0.03 | 0.3 | 0.000 | |||||
| P FB | 0.002 | 0.000 | 0.6 | 0.6 | 0.000 | |||||
- DIBH, deep inspiration breath hold; FB, free breathing; GCI, global conformity index; PTV, planning target volume.
Dosimetric parameters: OAR
The VMAT and 3D-CRT plans were also compared in terms of dose to OAR. All plans met the mandatory dose OAR aims, except for two cases of the 3D-CRT arm, due to ipsilateral lung (iL) V30%, one case of the 3D-CRT arm and seven cases of the VMAT arm due to heart V5%.
Skin, iL and heart were considered for OAR dosimetric evaluation (Figure 3).

A statistically significant increase was observed in the analysis of skin V103% for both DIBH (P = 0.0005) and FB (P = 0.001) series in 3D-CRT plans.
The V30% analysis for iL showed a significant increase in 3D-CRT plans for both the DIBH (0.3% vs. 0%, P < 0.05) and FB (0.29% vs. 0%, P = 0.005) series.
As for the heart, the analysis of DIBH series showed significant increases in terms of V5% (22.39% vs. 8.15%, P = 0.002) and Dmean (1.06% vs. 0.61% P = 0.0002) mean values for VMAT plans.
In the FB patients’ series, V5% (29.47% vs. 11.89%, P < 0.05) and Dmean (1,41% vs. 0,96%, P < 0.05) showed significant increase, while Dmax mean values (11.78 Gy vs. 19.78 Gy, P = 0.001) were reduced in VMAT plans.
Table 4 summarises the OAR dosimetric parameters.
| Ipsilateral lung | Heart | Skin | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| V30% | V5% | V25% | Dmax (Gy) | Dmean (Gy) | V103% | |||||||
| 3D-CRT (%) | VMAT (%) | 3D-CRT (%) | VMAT (%) | 3D-CRT (%) | VMAT (%) | 3D-CRT (Gy) | VMAT (Gy) | 3D-CRT (Gy) | VMAT (Gy) | 3D-CRT (%) | VMAT (%) | |
Mean ± SD DIBH |
12.13 ± 2.28 | 8.33 ± 2.15 | 8.16 ± 5.46 | 22.39 ± 14.26 | 0.55 ± 0.74 | 0.62 ± 0.92 | 14.04 ± 9.48 | 11.00 ± 4.73 | 0.61 ± 0.22 | 1.06 ± 0.33 | 0.30 ± 0.18 | 0.0 ± 0.0 |
Mean ± SD FB |
13.35 ± 4.69 | 8.18 ± 3.17 | 11.89 ± 6.75 | 29.47 ± 10.72 | 0.96 ± 0.95 | 1.41 ± 1.81 | 19.78 ± 6.43 | 11.78 ± 6.40 | 0.76 ± 0.26 | 1.29 ± 0.34 | 0.29 ± 0.20 | 0.0 ± 0.0 |
| Two-tailed paired t-test | ||||||||||||
| P DIBH | 0.00 | 0.00 | 0.8 | 0.1 | 0.00 | 0.00 | ||||||
| P FB | 0.01 | 0.00 | 0.5 | 0.00 | 0.00 | 0.00 | ||||||
- DIBH, deep inspiration breath hold; FB, free breathing; GCI, global conformity index; PTV, planning target volume.
Discussion
This study analyses the dosimetric data of 1-week hypofractionated adjuvant RT treatments in patients with left EBC delivered through both 3D-CRT and VMAT techniques. In our experience, both VMAT and 3D-CRT resulted to be dosimetrically feasible, with overall slight advantages for 3D-CRT.
The recent paper by Brunt et al demonstrated the safety and efficacy of hypofractionated treatment for EBC.19
This 1-week treatment may play a significant role in the management of EBC, potentially representing the new standard of care, thanks to the positive results observed in the FAST-FORWARD study and to the several logistic advantages offered by this approach, such as the favourable impact on the RT departments resources with waiting list reduction and restraint of healthcare costs and patients’ private expenses.30
Nevertheless, this study has several limitations. First of all, it is a retrospective study based on arbitrary selection criteria and enrolling a small number of patients. Despite these limitations, the observed dosimetric findings support the use of both VMAT and 3D-CRT techniques in this treatment setting.
In this frame, the reduction in unnecessary OAR irradiation could represent the most significant advantage, considering the possible proximity with systemic therapies, especially when using VMAT techniques in this setting, thanks to the improved dose conformation and the reduction in dose peaks to the skin, lung and heart.31
Unfortunately, VMAT dosimetric indications have not been reported in the FAST-FORWARD trial (that suggested only to notify the QA team in the case of this occurrence), and in this study, we therefore aimed to meet the dose limits and constraints used in the original protocol for the 3D-CRT technique also for our VMAT planning approach (Table 1).19
The data we collected showed how these two planning techniques can achieve excellent results, in terms of both target coverage and OAR constraints.
Notably, VMAT technique proved to be superior for GCI and V30% iL sparing, although mandatory constraints (iL V30 ≤ 17%) have always been respected, also with 3D-CRT except for two cases.
Conversely, no advantage has been observed with the use of VMAT technique with regard to dose peaks.
The 3D-CRT technique, on the other hand, proved to be superior for heart V5%, with the mandatory dose constraint V5%≤25% being not respected with VMAT technique in seven cases.
These results reinforce data from other studies and planning experiences that suggest that VMAT increases both heart Dmean and V5% values.32-36
The treated breast volume was larger when compared to the ones of the other patients in which dose constraints were respected, being generally larger than 750 cc.
Furthermore, DIBH was not used in six of these patients and this could have potentially penalised the heart sparing with the hypofractionated scheme.
VMAT technique may therefore be preferred to reduce V30% iL and improve GCI, while 3D-CRT planning is better to spare heart low doses.
According to these findings, it could be practically suggested to firstly use the VMAT technique to improve the GCI and preserve the V30% iL, eventually switching to a 3D-CRT technique when exceeding the heart V5%. Our results also confirm that the use of gating is strongly recommended for left EBC to reduce at best the dose to the heart, especially when VMAT planning is chosen.
On the other hand, in the case of particularly large left breasts, we suggest to immediately use the 3D-CRT planning technique.
Conclusions
This in silico study confirmed that both irradiation techniques are feasible at dosimetric level in the frame of 1-week hypofractionated treatment of left EBC, with overall slight advantages for 3D-CRT, mainly thanks to a more efficient low-dose heart sparing.
A subgroup analysis of the patients enrolled in the FAST-FORWARD trial treated with VMAT technique would of course be useful to strengthen the robustness of our observations and further explore this planning comparison.
Future prospective studies comparing the two irradiation techniques may definitively establish which technique is better for this specific treatment, especially with regard to toxicity reduction and cosmetic results, which represent particularly important outcomes in this cohort of patients characterised by overall good prognosis and favourable survival outcomes.
Funding
All authors received no specific funding for this work.
Conflicts of Interests
All authors declare no conflicts of interest.