Access to clinical genetic services: An evaluation of patient referral characteristics and identifying barriers in Michigan
Abstract
The utilization of genetics in medical care has enhanced the utility of precision medicine and hence increased the need for clinical genetic services. These services have reduced the costs and expanded the availability of genetic testing, but their use is limited in certain populations. This study explores the access to clinical genetic services for Michigan patients referred to a genetics clinic on the western side of the state. Factors included the travel distance (miles), wait time for appointment (days from the referral date to the date of first appointment), population demographics, and cultural characteristics. A retrospective record review of all aged patients (n = 568) referred to a genetics clinic in 2018 demonstrated that all patients were insured (100%), of which majority were white-non-Hispanic (90.7%), more than half were < 10 years of age at referral (53.3%), and most of them kept their first appointment (93.5%). Our analysis showed that the wait time was associated with referral non-compliance, p < 0.01. Adjusting for all variables, for each additional day in wait time, patients had 1% increased risk of not seeking clinical genetic services (OR = 1.01, 90% CI [1.01, 1.02]). Policies to encourage genetic service utilization and improve equitable access to precision health are needed. An opportunity exists for strategies that broaden and add diverse populations to those receiving genetic services.
What is known about this topic?
Access to clinical genetic services remains limited as utilization of genetics and genomics in healthcare continues to expand. This impacts patient care, outcomes, and is an ongoing present, and future concern.
What this paper adds to the topic?
Key factors for improving access include the travel distance, wait time for appointment, population demographics, and cultural characteristics. Focusing strategies in those areas may help address genetic service utilization, equitable access, and improved outcomes.
1 INTRODUCTION
Genetics in medicine is ever expanding, enhancing the utility of precision medicine, and changing medicine as it continues to grow. Since the human genome project, technology advancements have been rapidly improving human genetic diagnosis and treatment and this progression is enhancing the understanding of the molecular basis of genetic diseases, the role of the environment, and gene–disease associations. The medical specialty of clinical genetics includes service elements such as genetic evaluation and testing, diagnosis of genetic conditions, genetic counseling, and the treatment for individuals with, or at risk of, genetic disorders (Clinical Genetics Society, 2019; Doyle, 2009; Spectrum Health, 2019). As scientists, researchers and clinical genetics providers continue to understand the connection between human genes and disease, the realm of genetic services continues to develop.
The United States is at the forefront of genetic testing availability, which is already a major element of health care (World Health Organization, 2019). In 2003, the National Institutes of Health (NIH) funded a directory for laboratories performing genetic tests, which listed nearly 650 types of genetic tests, which did not include 340 tests that were being used for research only.
Since the launch of the United States National Precision Medicine Initiative by the then President Barack Obama in 2015 (The White House, n.d.), technology advancements in genetic medicine and scientific understanding of genetic disorders have contributed to the growth in demand for genetic professionals and their services (Mamun et al., 2019). Recent research demonstrates the need for referrals to genetic specialists by showing that many physicians lack the skills required to provide appropriate genetic services (Diamonstein et al., 2018). In a recent needs assessment of the current practice within the field of medical genetics, findings on key genetic service practice components revealed increased patient wait times and average new patient caseloads, but no increases in the number of geneticists (Jenkins et al., 2021; Maiese et al., 2019). In 2020, the U.S. Bureau of Labor Statistics (2022) reported that 3220 genetic counselors were employed in the United States and according to the American Board of Medical Genetics and Genomics (2023), there were 76 board certified medical geneticists in the state of Michigan. According to the United States Government Accountability Office (2020), on average, there were two medical geneticists per 500,000 in 2020. The U.S. Department of Labor estimates that there are 60 direct patient care genetic counselors employed in Michigan (United States Bureau of Labor Statistics, 2022) while the National Society of Genetic Counselors [2024] estimates 50–99 in Michigan. Among the 83 Michigan counties the United States Census Bureau estimates the population of Michigan to be 10,034,113 (United States Census Bureau, 2022; State of Michigan, 2019). Based on these numbers the ratio of genetic professionals to the population in Michigan is 1 geneticist per 167,235 individuals. In Michigan, five specialty pediatric genetics clinics can be found. All five medical genetics clinics have their main location in the lower peninsula, though some outreach clinics do exist. One is on the west side of the state and all others (Detroit Medical Center, University of Michigan, Henry Ford Health System in Detroit), and Corewell Health East are located in Southeast Michigan. This ratio as well as the lack of balance in geographic locations of genetic clinics in Michigan reveals potential disparities in access to clinical genetic services.
2 BARRIERS IN GENETIC SERVICES USE
Adherence to genetic referrals hinges on many factors including race/ethnicity, education level, insurance coverage, fears of discrimination, and costs (Frey et al., 2022). A meta-analysis of factors that act as barriers to patient referral concluded the need for stronger evidence on factors that are barriers to developing “targeted interventions” for equitable access to genetic services in a range of populations (Delikurt et al., 2015). Factors related to individuals included lack of awareness of risk, lack of knowledge of family medical history, and genetic services. Factors related to healthcare professionals included lack of awareness of genetics in general, in genetic services, in patient risk factors, and lack of genetics workforce (Delikurt et al., 2015).
The significance of understanding current local access, barriers, and demographic characteristics to genetic services has grown in recent years (Maiese et al., 2019; Senier et al., 2019). Much of the literature explains the increased demands for genetic services coupled with a lack of genetic professionals. Maiese et al. (2019) painted a dire picture where a majority of geneticists (n = 249) in their study had practices that were full, while noting approximately 100 geneticist and 200 genetic counselor job vacancies.
With averages of 10.2 new patients per week, some have suggested telehealth to help with time constraints in seeing patients, but the use of telehealth by genetic professionals is reported at less than 18% (Maiese et al., 2019; Senier et al., 2019). Studies relevant to the comprehensive utilization of genetic services and disparities in genetics care are unfolding in literature, thereby suggesting the need for further investigation and resource support for the expansion of genetic services (Dragojlovic et al., 2020; Maiese et al., 2019; Senier et al., 2019). This is based on understanding the current state of the genetics workforce and the expected increased demand for their services (Dragojlovic et al., 2020). There is no disagreement on the problem, and suggestions for improvement have not been proven successful as of yet. Recommendations include collaboration between medical sectors, attracting students to the genetics field, and increasing efficiency through automation and streamlining processes (Dragojlovic et al., 2020; Maiese et al., 2019; Senier et al., 2019).
According to a study of genetic service providers' perception of patient barriers to seeking genetic counseling after referral, geographical distance to appointments made up 48% of patients' perceived barriers (Rolnick et al., 2011). Due to the shortage of genetic professionals, it is assumed that the patient barrier of distance to service is halting access (Case et al., 2008; Penon-Portmann et al., 2020; Seibel et al., 2022). In rural or medically underserved communities, telehealth genetic services have been recommended, and in some areas implemented, to provide genetic counseling services via video conference to those who would otherwise not have access to genetic specialists (Penon-Portmann et al., 2020; Villegas & Haga, 2019). Telehealth genetic services have been shown to improve access to genetic services by reducing such barriers (Boothe & Kaplan, 2018; Frey et al., 2022; Iredale et al., 2005). Telephone genetic counseling was shown to be associated with several advantages including decreased costs and perceived stress, and better satisfaction (Frey et al., 2022). A successful example of a telegenetic service is in the state of Mississippi. The location of genetic services is concentrated in Jackson, creating economic challenges for patients to travel there (Boothe & Kaplan, 2018). The only other option is to travel out of state, which is also not ideal. Implementation of a telegenetics clinic was begun to address access by providing convenience, lower costs, and decreased travel time (Boothe & Kaplan, 2018). After 1 year, the clinic was performing well and growth was planned. Literature suggests that rural individuals and families may not be benefitting from modern genetic advances such as tumor heterogeneity, greater knowledge in epigenetics, and precision medicine (Smith et al., 2016), and distance is a meaningful measure of access (Case et al., 2008; Iredale et al., 2005; Penon-Portmann et al., 2020; Smith et al., 2016; Stitzenberg et al., 2007; Villegas & Haga, 2019).
Financial constraints and insurance coverage among low socioeconomic status (SES) populations may act as a barrier to obtaining genetic services. The cost of genetic testing varies widely, from approximately $100 to more than $2000, depending on the nature and complexity of the suspected condition as well as how much is covered by insurance (National Library of Medicine, 2021). In a survey of genetic counselors from eight integrated health systems, the second-highest ranked perceived barrier to genetics referrals was concerns related to the impact of insurability (52%), followed closely by lack of insurance (44%; Rolnick et al., 2011). Individuals with little income are more likely to be Medicaid recipients or uninsured. After recent Medicaid expansion in some U.S. states, patients in one study were shown to have an increase in cholesterol check and blood pressure medication. However, flu shots and routine doctor visits showed no change (Kim & Zhao, 2021). Furthermore, low education levels among this population may also play a role in the perception of access and understanding of benefit to genetic services.
Other demographic variables may also affect barriers. Age of genetic disease onset ranges from infancy to the elderly. Considering the wide scope of the genetic impact across the lifespan, age is an important factor when determining the ability and desire to seek care. Age differences present varying levels of genetic knowledge, health literacy, and beliefs about the causation of health conditions (Krakow et al., 2017). One study out of New York, U.S.A. found that when compared to younger age groups (18–25 years), older age groups have lower levels of genetic knowledge and health literacy (26–35 years, p = 0.011; 36–49 years, p = 0.002; 50 years and older, p < 0.001; Ashida et al., 2011).
Sex is an important determinant of health, especially when considering genetic components such as sex chromosome aneuploidies, behavioral factors, differences in carrier status, and assistance in reproductive technologies. Trends in healthcare utilization in the United States suggest that women use significantly more services over their lifespan when compared to men (Swoboda et al., 2023).
Literature related to racial and ethnic health disparities in health care services and among diseases is rich. From a genetic perspective, ethnic disparities have been associated with preterm birth, infant mortality, morphological characteristics, disease susceptibility, and environmental response, as well as knowledge and utilization (Bamshad et al., 2004; Carroll et al., 2019; Mamun et al., 2019; Suther & Kiros, 2009). Differences were demonstrated in a study using the National Cancer Institute's Health Information National Trends Survey. The results showed out of 3.285 participants, 57% were aware of genetic testing, but differed by age, income, and race (Krakow et al., 2017). Specifically, lower genetic knowledge was seen in older adults, those with lower incomes, and minorities (Krakow et al., 2017). Hispanic populations in the United States are comprised of individuals from several Spanish-speaking countries, with varying cultures, religions, and fluency in the English language (Hallford et al., 2020). These are further challenges that may add to health disparities. Fraiman and Wojcik (2021) stated that Hispanic children with genetic issues are likely to be diagnosed less due to being missed in all five steps required in the overall process of diagnosing genetic disorders. The authors pointed to geographic reasons and lack of awareness of genetic testing. Non-Hispanic White people were more likely to have clinical genetic testing compared to other ethnic groups, but were similar to Hispanics and non-Hispanic Black people in rates of direct-to-consumer genetic testing. Of these, non-Hispanic White people were more likely than other ethnic groups to speak to a medical professional about abnormal results (Carroll et al., 2019).
The aim of this retrospective study was to explore access to clinical genetic services offered in a genetics clinic on the west side of the state of Michigan and identify barriers to access. We looked for an association between distance in miles from clinical genetic services and receipt of clinical genetic services. Medical genetic services refer to medical genetics services for adult and pediatric patients but exclude cancer, prenatal, and metabolic genetics. Additional variables included age at referral, sex, ethnicity, language, insurance coverage, income, education, and wait time.
3 METHODS
This study utilized a retrospective record review study design with primary data acquired from two sources: hospital-based electronic medical records, and The American Community Survey from the United States Census Bureau (2022a). The hospital is one of three hospitals in Grand Rapids, MI, and one of 10 regional hospitals in the state (Corewell Health, 2024a). Medical genetic services are offered through the children's hospital. The professional team includes geneticists and genetic counselors who provide testing, diagnosis, and risk counseling to pediatric and adult patients (Corewell Health, 2024b). A referral report from the hospital-based electronic medical record captured all patients with Michigan zip codes who had been referred for medical genetic services during 2018. Included in the referral report were all covariate demographic characteristics including age at referral, sex, ethnicity, language, insurance coverage, wait time, zip code and county of patient's primary residence, and two variables to compute receipt of clinical genetics services: referral reason and scheduled/completed visits (i.e., 1/1, 1/0, 0/0, 0/1). Four variables were created to complete the dataset: distance in miles, income, education, and the binomial outcome, receipt of genetic services. Since SES is not assessed at the time of referral, income, and education variables were created using represented counties from the referral report with the American Community Survey from the United States Census Bureau to understand the general SES of counties where patients reside.
4 REFERRAL PROCESS FOR GENETIC SERVICES
Referrals to genetic services are received in three different ways: third party, electronic medical record, and facsimile. The referral process is completed through a third party, Great Lakes Health Connect, and facsimile referrals are entered into the electronic medical record, EPIC. Anyone with access to EPIC can generate referrals. At that time, a determination process is initiated to determine referral appropriateness and what type of appointment is needed prior to scheduling. Once this determination has been made, personnel contact the patient to schedule an appointment. While conducting this study the process for scheduling patient appointments changed. In the beginning of the study, referred patients would be automatically scheduled by the genetics clinic staff then patients would be contacted to notify them of their appointment. This process was reversed after a change was introduced. Referred patients were called first to notify them of their referral then personnel would request to schedule their appointment with the patient. Appointments are scheduled using a team-based care model where all patients see either a medical geneticist, a genetic counselor, or both. The focus of services provided at this genetics clinic are hospitalized pediatrics and the general population. Cancer and reproductive genetic services follow a separate referral process and therefore were excluded from this study.
A total of 2336 patients were referred to a West Michigan medical genetics clinic for services in the year 2018. The inclusion criteria for this study were a referral to the medical genetics department between January 1, 2018, and December 31, 2018, and Michigan residency. Ten patients resided out of state and were therefore excluded from the study. Additionally, 1219 observations were omitted due to conditions not accepted for referral (referrals made in error, genetic evaluation was not appropriate; n = 157, 12.9%), duplicate referrals (referrals with matching age at referral, sex, zip code, insurance type and reason for referral; n = 234, 19.2%) and missing data points (patients with missing variables; n = 828, 67.9%). Corewell Health's IRB only approved a sample size limited to the greatest sample size needed for adequate power in the study. The final analytic sample of 568 patients was randomly selected from the remaining 1117 referred patients who met criteria. Due to a small study sample, a more narrow CI (90%) was used.
5 DATA MEASUREMENTS AND STATISTICAL ANALYSES
The outcome variable, receipt of clinical genetic services, was measured as “no” or “yes” based on a patient's referral compliance of either missing (0) or keeping (1) their first scheduled appointment. The reason for a missed appointment included no-shows, cancellations, and first appointments scheduled outside of the study timeframe. These patients were considered not compliant with their referral. Patients who attended their first scheduled appointment during this study timeframe were considered compliant with their referral. The independent variable of interest was distance in miles from the referred patient's primary residence to the genetics clinic. Distance was computed using zip codes in a web-based application. The covariates considered in this study were the following demographic and cultural characteristics: age at referral, sex, ethnicity, language, insurance coverage, income, education, and wait time defined as days from referral date to the date of first appointment. Insurance coverage was the patient's primary insurance reported at the time of referral. Income was determined by the median household income of the county where the patient resides. Education was defined as the percentage of the county population where the patient resides that attains a high school diploma. Income, age and education were all categorized into groups for analysis.
Univariate analyses were used to examine distributions in patient characteristics. Quartiles from univariate analyses were necessary for the variables wait time and distance due to skewness, heavy kurtosis and outliers in the distribution. Chi-square tests were conducted to determine associations between the receipt of clinical genetic services and independent variables. Fisher's exact tests were used for determining the associations of language and county. Multivariate logistic regression models were used to analyze the odds of not keeping the first appointment to genetic services for significant associations. Three logistic regression models were performed to assess the covariate contribution with non-compliance of genetic referral using backward elimination. The first model was unadjusted including only insurance coverage and wait time. The second model was also unadjusted including only insurance coverage and wait time, and the primary outcome, distance. The third and final model was adjusted including all variables, including the primary outcome. Statistical significance was set at <0.05.
Insignificant variables were excluded from models one and two, and were only included in the third model. Firth's estimation was applied to all logistic regression models to reduce bias in the assessment of the rare event of referral non-compliance, validating the maximum likelihood estimates. Interaction effects were not evaluated. All analyses were conducted using Statistical Analysis Software (SAS) version 9.4.
6 RESULTS
In this study, all patients (n = 568) were referred to the hospital system's medical genetics clinic during 2018 and resided in the state of Michigan. The primary outcome was the receipt of clinical genetic services. The primary exposure was travel distance between the referred patient's primary residence and the genetics clinic. Covariates considered for the primary outcome included age at referral, sex, ethnicity, language, insurance coverage, income, education, and wait time.
Of the study sample, almost all patients kept their first appointment after being referred (93.5%) indicating referral compliance. Most of the sample was non-Hispanic, White (90.7%). All study patients were insured, with approximately two-thirds of patients commercially insured (64.6%) and approximately one-third of patients with government insurance (35.5%). Nearly half (44.6%) of all study patients resided in Michigan counties where median household income is ≥ $60,000. Furthermore, nearly all study patients (94.9%) resided in Michigan counties where at least 87% or more of the county population hold at minimum a high school diploma. The distribution of sex was approximately equal between males (51.1%) and females (48.9%), and more than half of study patients were < 10 years old at date of referral (53.3%). Chi-square analyses of all variables with receipt of clinical genetic services are shown. Variables found to be significantly associated with receipt of clinical genetic services included insurance coverage (p = 0.04) and wait time (p < 0.01; Table 1).
| Frequency (%) (n = 567) | No receipt (6.51) (n = 37) | Receipt (93.5) (n = 530) | Statistic | |
|---|---|---|---|---|
| Age at referral | ||||
| <10 | 302 (53.3) | 21.0 (3.70) | 281 (49.6) | χ2(3) = 0.6228, p = 0.89 |
| 10–19 | 126 (22.2) | 7.00 (1.23) | 119 (21.0) | |
| 20–49 | 104 (18.3) | 6.00 (1.06) | 98.0 (17.3) | |
| ≥50 | 35.0 (6.17) | 3.00 (0.53) | 32.0 (5.64) | |
| Sex | ||||
| Male | 290 (51.0) | 14.0 (2.47) | 275 (48.5) | χ2(1) = 423.8, p = 0.10 |
| Female | 278 (48.9) | 23.0 (4.06) | 255 (45.0) | |
| Ethnicity | ||||
| White, non-Hispanic | 515 (90.7) | 34.0 (6.00) | 482 (85.0) | p = 0.85 |
| Hispanic | 52.0 (9.16) | 3.00 (0.53) | 48.0 (8.47) | |
| Language | ||||
| English | 551 (97.0) | 35.0 (6.17) | 515 (90.8) | p = 0.38 |
| Other | 17.0 (2.99) | 2.00 (0.35) | 15.0 (2.65) | |
| Education | ||||
| <87.0% | 29.0 (5.11) | 2.00 (0.35) | 27.0 (4.76) | χ2(2) = 2.821, p = 0.26 |
| 87.0%–91.9% | 361 (63.7) | 28.0 (4.94) | 333 (58.7) | |
| ≥92.0% | 177 (31.2) | 7.00 (1.23) | 170 (30.0) | |
| Income | ||||
| <$50,000 | 173 (30.5) | 16.0 (2.82) | 157 (27.7) | χ2(2) = 3.0744, p = 0.22 |
| $50,000–60,000 | 141 (24.9) | 7.00 (1.23) | 134 (23.6) | |
| ≥$60,000 | 253 (44.6) | 14.0 (2.47) | 239 (42.2) | |
| Insurance coverage | ||||
| Commercial/private | 366 (64.6) | 18.0 (3.17) | 348 (61.4) | χ2(1) = 4.3740, p = 0.04* |
| Government | 201 (35.5) | 19.0 (3.35) | 182 (32.1) | |
| Wait timea, median (IQR) | 73.0 (44.0, 97.0) | 72.0 (43.0, 96.0) | 83.0 (59.0, 124) | p = <0.01* |
| Distanceb, median (IQR) | 32.0 (11.1, 58.2) | 32.0 (9.91, 58.2) | 31.8 (17.8, 55.7) | p = 0.53 |
| County | ||||
| Kent | 162 (28.6) | 9.00 (1.59) | 153 (27.0) | p = 0.83 |
| Ottawa | 59.0 (10.4) | 3.00 (0.53) | 56.0 (9.88) | |
| Muskegon | 46.0 (8.11) | 4.00 (0.71) | 42.0 (7.41) | |
| Kalamazoo | 39.0 (6.88) | 0.00 (0.00) | 39.0 (6.88) | |
| Other | 261 (46.0) | 21.0 (3.70) | 56.0 (9.88) | |
| Referral statusc | ||||
| Complete | 530 (93.5) | 530 (93.5) | ||
| Patient refusal | 14.0 (2.47) | 14.0 (2.47) | ||
| No contactd | 23.0 (4.06) | 23.0 (4.06) | ||
- Note: For variable clarification.
- a Wait time was measured in days referral date to date of first scheduled appointment.
- b Distance was measured in miles from patient's primary residence to genetics clinic.
- c Referral status was not considered as a covariate.
- d No contact made with the patient after three attempts by the genetics clinic to schedule.
- * Significant independent variable of outcome.
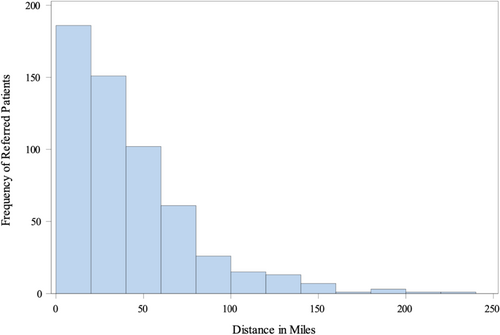
The majority of referred patients lived within 60 miles of the genetics clinic (75%), as shown in Figure 1. There was a wide range of travel distance (234 miles) from patient's primary residence to the medical genetics clinic with a median travel distance of 32.0 miles. The middle 50% of referred patients lived between 11.0 and 58.0 miles of the genetics clinic with a standard deviation of 36.7 miles, as shown in Table 2.
| b | p Value | Odds ratio | 90% CI | |
|---|---|---|---|---|
| First model | ||||
| Intercept | −3.52 | <0.01 | ||
| Insurance coveragea | 0.306 | 0.08 | 1.84 | 1.05, 3.25 |
| Wait time | 0.0108 | <0.01* | 1.01 | 1.01, 1.02 |
| Second model | ||||
| Intercept | −3.50 | <0.01 | ||
| Insurance coveragea | 0.311 | 0.08 | 1.86 | 1.04, 3.35 |
| Wait time | 0.0108 | <0.01* | 1.01 | 1.01, 1.02 |
| Distance | −0.000320 | 0.943 | 1.00 | 0.992, 1.01 |
| Third model | ||||
| Intercept | −3.18 | <0.01 | ||
| Distance | 0.000609 | 0.92 | 1.00 | 0.991, 1.01 |
| Sexb | 0.301 | 0.08 | 1.82 | 1.03, 3.30 |
| Ethnicityc | −0.182 | 0.63 | 0.695 | 0.155, 2.22 |
| Languaged | −0.506 | 0.27 | 0.364 | 0.0780, 1.87 |
| Insurance coveragea | 0.314 | 0.08 | 1.87 | 1.02, 3.44 |
| Income | 0.124 | 0.70 | 1.14 | 0.429, 2.80 |
| Education | 0.200 | 0.50 | 1.21 | 0.399, 4.81 |
| Wait time | 0.0100 | <0.01* | 1.01 | 1.01, 1.02 |
- Note: For variable clarification.
- a Insurance coverage coded as government = 1, commercial = −1.
- b Sex coded as female = 1, male = −1.
- c Ethnicity coded as Hispanic = 1, non-Hispanic = −1.
- d Language coded as English = 1, Other = −1.
- * Significant independent variable of outcome.
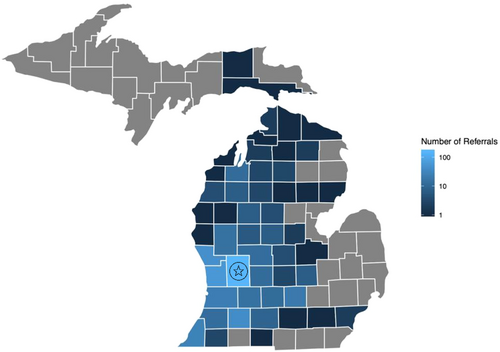
Figure 2 is a map of Michigan showing locations and frequency of medical genetic referrals by county of patient's primary residence. The medical genetics clinic serves over half of the state (51 of 83 counties, 61.5%). As travel distance from the clinic increases, counties get darker representing few referrals with increased travel distance.
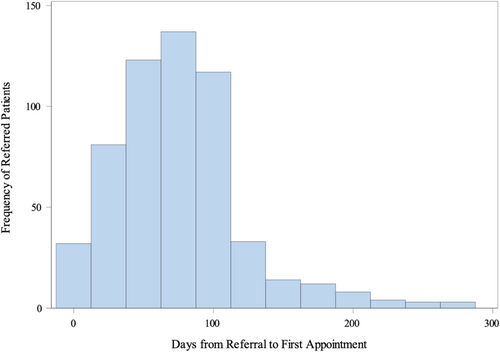
The majority of referred patients waited less than 3 months for their first genetics appointment (75.0%), as shown in Figure 3. There is a wide range of wait time (287 days) from the patient's referral to the medical genetics clinic appointment with a median wait time of 73.0 days. The middle 50.0% of referred patients waited between 44.0 and 97.0 days for their first genetics appointment with a standard deviation of 46.1 days.
Similar to the results of the Chi-square analysis, distance was not associated with the receipt of clinical genetic services as it was the first variable removed from the model. The last variables to be removed in the backward elimination were sex, insurance coverage and wait time. Wait time was the only significant variable (p < 0.01; Table 2). Sex and insurance coverage revealed an association with marginal significance (p = 0.08; p = 0.08, respectively; Table 2).
According to the first model, the log of the odds of insurance coverage and wait time were both positively associated with not receiving clinical genetic services (p = 0.08; p < 0.01, respectively; Table 2). The odds of a patient with government insurance not receiving clinical genetic services were nearly two times greater than patients with private insurance while controlling for wait time (OR = 1.84, 90% CI [1.05, 3.25]; Table 2). Furthermore, adjusting for all variables, for each additional day in wait time patients had a 1% increased risk of not seeking clinical genetic services (OR = 1.01, 90% CI [1.01, 1.02]); Table 2.
Similar to the previous model, the second model demonstrates that the log of the odds of insurance coverage and wait time were both positively associated with not receiving clinical genetic services (p = 0.08; p < 0.01; Table 2).
According to the third model, the log of the odds of wait time, insurance coverage, distance, sex, income, and education were all positively associated with not receiving clinical genetic services (p < 0.01; p = 0.08; p = 0.92; p = 0.08; p = 0.70; p = 0.50, respectively; Table 2). Income and education were county level variables, which limit the interpretation of these results. Wait time, insurance coverage, and sex were found to be associated with referral compliance, as shown in Table 2. Similar to previous models, increased wait time slightly increased the likelihood of patients not receiving clinical genetic services with significance (OR = 1.01, 90% CI [1.01, 1.02]; Table 2). Furthermore, the odds of a patient with government insurance not receiving clinical genetic services was 1.87 times greater than patients with private insurance, (OR = 1.87, 90% CI [1.02, 3.44]; Table 2). This model also revealed that the odds of females missing their appointment for clinical genetic services are 1.82 times greater than the odds of males missing their appointment (OR = 1.82, 90% CI [1.03, 3.30]; Table 2). Increased odds of sex and insurance coverage are questionable due to non-significance and lower limit of confidence intervals being close to one. Distance, ethnicity, language, income, and education were not significantly associated with the likelihood of not receiving clinical genetic services. Language, education, and ethnicity were not significantly associated with the likelihood of not receiving clinical genetic services (p = 0.27, p = 0.50, p = 0.63; Table 2).
7 DISCUSSION
This study explored factors and potential barriers relating to patients who were referred for medical genetic services and received those services. Our results suggested that the wait time, insurance coverage, and sex are all associated with referral compliance and therefore act as potential barriers to genetics care in this population. Our analyses showed that with increased time between referral and first scheduled appointment, defined as wait time, there was an increased likelihood of a patient not complying with their genetics referral by missing their first scheduled appointment. While statistically significant this suggests there are greater odds of not receiving genetic services with increased wait time, however, clinically the odds of not receiving services due to increased wait time is small in this sample with marginal impact on patient care. Associated delays in days related to this finding were not investigated in this study. Whether this effect is clinically or practically significant is difficult to ascertain. Small effect sizes can be meaningful statistically for serious outcomes. Applied to an entire population, this finding could be relevant; however, for this sample alone, it is most likely not.
Wait time, measured in days with a median of 73 days, was found to be associated with receiving genetic services and with increased wait time and increased odds of referral non-compliance with confidence, supporting current research suggesting demand for genetic services. This suggests from the time of referral to the date of appointment was less than 3 months. This is similar to data presented by Maiese et al. (2019), where 62% of geneticists in their study had wait times for new patients over a month, and 39% were more than 3 months. They did find over a 10-year time frame that wait time had increased particularly in the 1–3 month range (Maiese et al., 2019). An implication of this research finding to improve access was employing additional genetic counselors to decrease wait times and having genetic counselors seek licensures to provide more services covered through insurance (Nowlen & Flores, 2021).
This study revealed that male patients were slightly more likely to comply with their genetics referral compared to female patients (48.5% vs. 45.0%). This finding is in agreement with a study on willingness to undergo genetic testing. Males were found to have more positive attitudes regarding testing (Likhanov et al., 2023). Other studies were contradictory between males and females in genetic knowledge and biotechnology, questioning possible reasons for the results Likhanov et al., 2023. Utilization of genetic services may be more indicative of parental response in cases of pediatric patients. An example is found in a similar study where parents sought genetic services for a child which was unnecessary because of a lack of knowledge of the disease being adult-onset. This shows parental initiative for services when regarding children (King et al., 2022). Since more than half of the patients were < 10 years old at the date of referral in this sample (53.3%), and have adherence dependent of the parent/guardian, it is challenging to draw firm gender conclusions on complying with genetics referral.
This study showed that referred patients with government insurance were nearly twice as likely to not comply with their referral to genetics than those with private insurance. Approximately 61.4% of those with private insurance completed genetic services, and 32.1% with government insurance completed services. This is similar to a study by Lin et al. (2021) where insurance coverage was a factor in the receipt of clinical genetic services in nine countries. They reported lower rates of genetic testing for those who were uninsured compared to those who had insurance. Those who had been referred to genetic services and completed testing were 47% with private insurance, 26% with Medicare or Medicaid, and 23% who were not insured (Lin et al., 2021). On the contrary, no association was demonstrated between the receipt of clinical genetic services and travel distance to appointment, age at referral, sex, ethnicity, language, income, and education.
8 ADDRESSING BARRIERS
Overall, patient referral characteristics demonstrated that many individuals and families in Michigan are not benefiting from valuable genetics care due to the study population being primarily non-Hispanic White, English speaking, and insured. Uninsured and underserved populations may be missing potential diagnoses for treatable conditions as well as genetic counseling support for disease progression. Precision public health intervention would allow for long-term monitoring of population health for the phenotype genetic variant association of diseases. However, one of the major prerequisites for ensuring such benefit is to allow equal participation of all subpopulations in the genomic studies, which is still a challenge (Mamun et al., 2019). The “All of Us” research initiative launched by the NIH is a longitudinal cohort of Americans aiming to include 1 million or more people and is the most promising approach to maximize the benefits of precision medicine. However, to attain the maximum benefits of precision medicine, more actions are required to enhance diversity (Mamun et al., 2019). These variables may be considered when assessing access as potential barriers to medical genetic care and can serve as areas of focus for clinics to optimize their provision of genetics care.
Typical solutions include addressing the entire process beginning with a patient and provider encounter, a referral for genetic services, patient education, and genetic risk information to the patient (Dusic et al., 2022). According to Dusic et al. (2022), barriers exist at the patient level, primary care provider, and genetic testing processes. Solutions are believed to be found in all levels and stages, but admittedly, they have had little success (Dusic et al., 2022). Adding genomics to regular primary care has been suggested and met with such difficulties as clinician education in genomics, costs, time, and reimbursement issues (Dusic et al., 2022; National Library of Medicine, 2023). If even some of the challenges could be addressed, it may be a start toward changing the landscape of patients seeking and using genetic services. At the systems level, lowering the costs of genetic services and testing may help as it is a significant barrier (Korte & Terry, 2023).
Telehealth services were implemented at the Corewell Health Helen DeVos Children's Hospital shortly after this research concluded due to the COVID-19 pandemic and are readily available to patients. However, anecdotally the clinicians have found that patients prefer to attend in office appointments and suspect that patients want to make the most of their appointment due to the long wait time. With the scarce availability of genetic services across large areas of Michigan and geography in the United States, the challenge of travel distance could be a larger problem in other parts of the state, other states, and regions. With approximately 157 million Americans living paycheck to paycheck, such services may appear as an unaffordable luxury (Korte & Terry, 2023).
9 STRENGTHS AND LIMITATIONS
The primary strength of this study was its exploratory nature for the genetics clinic. It provides knowledge of current utilization of medical genetic services, benefiting providers and other key stakeholders and informants in the state of Michigan. To our knowledge, this is the first study of its kind presenting a unique challenge in comparability of results. The benefitof this is the inclusion of many important variables from the literature previously noted. In addition, the sample was representative of the general West Michigan population. According to The Right Place (2019), 80.3% of the population in West Michigan were White, non-Hispanic, and 7.3% Hispanic. The ethnicity of this sample population was similar to the demographics of West Michigan overall with White, non-Hispanic accounting for 90.7% and 9.16% Hispanic within the study population. According to Mack (2020), counties adjacent and in close proximity to the genetics clinic studied generally had lower percentages of uninsured populations (4.2%–6.2%) compared to all counties in the state of Michigan. Five-year estimates (2018–2022) of people who speak English at home in adjacent counties ranged from 87.6%–96.5% (United States Census Bureau, 2022a, United States Census Bureau, 2022b).
A limitation of this study was the small number of patients who did not keep their first clinical genetics appointment (n = 37) making referral non-compliance a rare event. A contributor may have been the implementation of an operational change in workflow within the genetics office during the time period of this study. Instead of immediately scheduling referred patients for an appointment, the genetics office began calling referred patients to ask if they knew about their referral and inquired about scheduling an appointment. This limited the analysis in two ways: (1) identifying significant associations between the receipt of clinical genetic services and independent variables, and (2) penalized the logistic regression models restricting the ability to associate referral compliance with independent variables. Perhaps a study with a larger sample may provide a more equal distribution of receiving genetic services providing enough power to better understand the significance of covariates.
Another potential limitation of this study included capturing only primary insurance coverage. Many known genetic conditions have special health care needs. In these circumstances, patients are often eligible for secondary Medicaid coverage, mitigating barriers to accessing genetic services. Additionally, since SES is not assessed at time of referral the use of income and education variables created represent only approximate estimates of SES from an ecological level. Therefore, this group level data cannot be used to make individual level associations.
Further consideration of the 1-unit increase in wait time (i.e. each day) measured in this study may be given due to the minimal impact on the overall log-odds of missing an appointment and could be more meaningful in a follow-up study to look at 30- or 60-unit increases in wait time.
10 FUTURE RESEARCH
Future research may consider including primary and secondary insurance coverage to fully understand access for genetic disorders. Additionally, income was based on county median values, and education was the percentage of those in the county with a high school diploma. More specific characterization of patient information could not be obtained for these variables. Referrals to cancer genetics were not incorporated into the data for this study, as those go through a separate queue and process at the hospital, introducing another potential limitation in capturing comprehensive referral characteristics and identifying disparities in care.
Although travel distance was not found to be associated with receiving genetic services in this population, it may be considered in future research as this finding could be related to the higher SES of the study population and that the majority of patients within this study were pediatric patients in close proximity to the hospital.
With the increased demand for genetic services, understanding barriers to referral compliance is crucial to effective utilization of genetic services. Demographic and cultural characteristics of referred patients exposed the underrepresentation of diverse populations, prompting the need for support of, and solutions to, expanding genetics care to underserved and uninsured populations while prohibiting increased wait time for referred patients. Policies aimed to improve equitable access should focus on extending genetics care to uninsured and underserved populations.
To validate the findings of this study, a larger sample consisting of referrals for all genetic disorders, the inclusion of patient and provider knowledge of medical genetics to inform programmatic education efforts as the benefits and expansion of genetics in medicine continue.
This knowledge may not only provide opportunities for medical genetics and public health but may also expand referrals to genetics and inform provider criteria for appropriate referrals improving the efficacy and utilization of medical genetic services. This knowledge is not only important at the individual level but also the population level as the onset of the genomic age is providing vital tools for disease prevention in the 21st century (Khoury, 2020). Together, precision medicine and public health may introduce the era of precision public health that will optimize prevention and treatment strategies for specific segments of the population (Mamun et al., 2019). Understanding access to clinical genetic services fosters these research advancements and provides a framework for similar investigations in the field of public health genetics.
AUTHOR CONTRIBUTIONS
Lacey N. Lemke: conceived and designed analysis, collected the data, performed analysis, and wrote the paper; Caleb P. Bupp: contributed to design, data collection and provided analysis tools and intrepretation; Karen L. Niemchick: contributed to design analysis, writing the paper and analysis intrepretation.
ACKNOWLEDGMENTS
This research was conducted to fulfill a degree requirement, and we acknowledge colleagues of Corewell Health Helen DeVos Children's Hospital and Grand Valley State University for their support.
CONFLICT OF INTEREST STATEMENT
We have no conflicts of interest to disclose.
ETHICS STATEMENTS
Human Studies and Informed Consent: This study was reviewed and waived by Corewell Health Helen DeVos Children's Hospital's Institutional Review Board (2019–643). No informed consent was obtained due to the exemption from Corewell Health Helen DeVos Children's Hospital's Institutional Review Board.
Animal Studies: Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.