Trends in coverage and reimbursement for reproductive genetic counseling in New Jersey by multiple payers from 2010 to 2018
Abstract
Lack of consistent insurance coverage for genetic counseling services billed under Current Procedural Terminology (CPT) code 96040 creates a barrier for access to this service. This retrospective study examined coverage and reimbursement for reproductive genetic counseling encounters billed under CPT code 96040 as a professional fee over an eight-year period at Rutgers Robert Wood Johnson Medical School, a regional perinatal center in New Jersey, a state requiring licensure. Descriptive statistics were tabulated to assess the disparity between Medicare/Medicaid, Managed Care Medicaid, and commercial insurance payers, including how often encounters were covered and if reimbursed, at what percentage of the amount billed. A comparison of individual plan types (Health Maintenance Organization, Point of Service, and Preferred Provider Organization) was carried out. Overall trends in reimbursement were assessed across payers. The study found 61% of 60-min encounters billed to Medicare/Medicaid, Managed Care Medicaid, and commercial insurance payers received coverage. Of all covered 60-min encounters billed to Managed Care Medicaid and commercial insurance payers, an average of 36% of the amount billed was reimbursed. Medicare/Medicaid encounters were never reimbursed. Commercial insurance covered 65% of encounters billed but this varied between payers. Across all payers, an overall downward trend of reimbursement was demonstrated over the eight-year period. Lack of consistent service coverage creates a barrier and patients cannot universally access genetic counseling services. Steps to improve coverage need to include passing of legislation, notably the next bill to replace the former H.R. 3235, ‘Access to Genetic Counselor Services Act of 2019’ and provisions within third-party payers that allow for credentialing of genetic counseling providers.
What is known about this topic
There are limited data regarding the billing, coverage, and reimbursement of genetic counseling services via CPT code 96040. Available data demonstrate there is a lack of understanding of genetic counseling services among third-party payers causing inconsistency in coverage and reimbursement of CPT code 96040.
What this paper adds to this topic
To our knowledge, this is the largest study (4,760, 60-min reproductive genetic counseling encounters) evaluating the longest time period (8 years) of billing, coverage, and reimbursement of CPT code 96040 when billed as a professional fee. The evidenced lack of consistent coverage and reimbursement creates a barrier for patient access to care.
1 INTRODUCTION
The field of genetic counseling is an established, rapidly growing division of health care with several states successfully advocating for and passing licensure legislation. The goal of licensure is to protect the public by ensuring credentialed professionals are appropriately trained to provide care within the confines of the law. Conversely, if licensed professionals provide inadequate care, licensure legislation outlines the indicated repercussions. Licensure was secured for New Jersey in April 2009 via the ‘The Genetic Counselor's Licensing Act’ (A269). Although licensure has been procured in some states, it is not ubiquitous across the United States. Certified genetic counselors are primarily involved in the ordering of appropriate genetic testing across several specialties. A lack of insurance coverage for genetic counseling services creates a barrier for patients to affordably access this medically necessary service.
Most private insurance payers lack an existing infrastructure to credential genetic counselors as in-network providers. Thus, CPT code 96040 when billed as a professional fee is applied to the patient's out-of-network benefits. In the case, a patient does not have out-of-network benefits, the individual is entirely responsible for the genetic counseling service fee.
The CPT code 96040 is intended to encompass 30 min of face-to-face counseling (National Society of Genetic Counselors, 2013) and is a stackable code. Currently, the Centers for Medicare and Medicaid Services (CMS) does not recognize CPT code 96040. Thus, the large patient population of CMS beneficiaries cannot access genetic counseling services if the out-of-pocket expense is not affordable. The American Medical Association/Specialty Society RVS Update Committee (RUC) created a relative value unit (RVU) that is multiplied by the physician conversion factor to give the suggested payment amount (National Society of Genetic Counselors, 2013). In 2007, the RVU for CPT code 96040 was 0.98 and this increased to 1.34 in 2018 (The American College of Obstetricians & Gynecologists, 2018). The physician conversion factor was $37.8975 in 2007 and decreased to $35.99 in 2018. Using the 2018 RVU and conversion factor, $48.23 of reimbursement is suggested for each billed unit of 96040. While CMS does not currently recognize CPT code 96040, Managed Care Medicaid payers will inconsistently reimburse some encounters. To address the lack of CMS recognition and reimbursement, the former federal bill, H.R. 3235, ‘Access to Genetic Counselor Services Act of 2019’ has been introduced. If the next bill to replace the former H.R. 3235, ‘Access to Genetic Counselor Services Act of 2019’ is passed, genetic counselors would be recognized by CMS via amendment of title XVIII of the Social Security Act, making genetic counseling services eligible for coverage under part B of the Medicare program and subsequently increase access for its beneficiaries.
Coverage and reimbursement of genetic counseling services under CPT code 96040 code have been studied since its 2007 inception. The first study completed in 2010 by the National Society of Genetic Counselors (NSGC) working group evaluated whether CPT code 96040 was used by genetic counselors across all specialties. They found 69% of respondents were billing for their services, and of those, only 24% used CPT code 96040. There was a lack of knowledge regarding the utility of 96040, for which Harrison et al. called for continued education to encourage the use of and reimbursement for CPT code 96040 (Harrison et al., 2009).
A 2010 study based in Illinois used a combination of surveys, interviews, and policy review to evaluate insurance plan coverage of genetic services. Of the participating payers, there was variability in attitudes toward genetic counseling and noted barriers to reimbursement. Through policy review, the authors found the payer policies for genetic counseling services and genetic testing to be inconsistent. The study called for strategies to be implemented for ‘improvement of billing, reimbursement, and insurance coverage of genetic services’ (Latchaw et al., 2010).
To assess whether an alternative billing practice would increase CPT code 96040 reimbursement, a 2011 study by Gustafason et al. reviewed billing using 96040 under a supervising physician NPI for a 14-month period. The authors did recognize billing under a physician provider was not consistent with the provisions of CPT code 96040, which requires a non-physician genetic counselor NPI be used. Of the 289 encounters billed to third-party payers, 62.6% received some level of reimbursement. Of the 108 encounters not reimbursed, 87 encounters included reasoning for lack of reimbursement. One third of these reasons were related to CPT code 96040. This study noted that for billing and reimbursement to move forward, ‘federal CMS should include genetic counselors as non-physician providers’ (Gustafson et al., 2011).
A 2015 study by Doyle et al. evaluated potential barriers for genetic counseling reimbursement. Data were collected by surveying 22 chief medical officers or medical directors at payer organizations who were asked to rate defined barriers to reimbursement. ‘Evidence that use of genetic counselors improves health outcomes’ and ‘licensure’ were cited as the largest barriers. Other payers noted they follow CMS’s infrastructure for reimbursement of genetic counseling services. There was also a concern about a return of investment on coverage of genetic counseling services, which notes an underlying apprehension about the validity of genetic counseling (Doyle et al., 2015).
Increased coverage of genetic counseling services will allow for genetic counselors to more consistently be involved in the selection and ordering of genetic testing. A 2017 oncology-based study by Haidle et al. (2017) demonstrated the utility in a genetic counselor ordering oncology genetic testing compared to other provider types. A genetic counselor's specialized training in analyzing a family history and selecting the most appropriate test or laboratory allows for the most cost-effective approach. The involvement of a genetic counselor reduces the financial burden on the healthcare system. In contrast, the studied non-genetic counseling providers made double the amount of test order errors, in turn increasing the financial burden on the healthcare system. By utilizing genetic counselors, the most appropriate testing can be completed first while lowering healthcare system and payer expenses alike. This is further demonstrated by Miller et al. in a 2014 study demonstrating the utility of laboratory genetic counselors reviewing ordered testing (Miller et al., 2014). Over a 21-month period, Associated Regional University Pathologists (ARUP) Laboratories genetic counselors recommended modification to 26% of molecular testing ordered after clinical review. These adjustments resulted in a net savings of almost $1.2 million dollars between the client, payer, and patient, again reducing the financial burden on the healthcare system. If genetic counselors are involved in ordering of genetic testing, a decrease in clinical and financial error is appreciated. For genetic counselors to be consistently involved in selecting the appropriate genetic testing, the primary barriers to access genetic counseling services need to be addressed.
As many medical specialties benefit from genetic counseling services, leading organizations and governing bodies have released guidelines for genetic counseling referrals. For reproductive genetics, The American College of Obstetricians and Gynecologists Committee Opinion 693 (American College of Obstetricians and Gynecologists Committee on Genetics, 2017) notes referrals to genetic counselors are appropriate when the genetics knowledge needed to counsel patients is outside of the physician's purview. For oncology genetics, both The National Comprehensive Cancer Network (2020) and the U.S. Preventive Services Task Force (2019) set several guidelines for the recommendation of patients to receive genetic counseling and risk assessment. Even if a patient is recommended to receive genetic counseling services, insurance coverage could be a barrier, preventing access to medically necessary care.
Many patients who meet consensus criteria for genetics services may not receive genetic counseling due to lack of coverage for the service by insurance carriers. This is a challenging issue across all genetic counseling specialties as a 2012 study by Anderson et al. (2012) reviewed the patient-reported barriers and facilitators for utilization of genetic counseling and risk assessment services among young breast cancer survivors. Of study subjects, 23.4% identified medical insurance coverage issues as the primary barrier of access to genetic counseling services. These patients were unable to obtain the standard level of care per consensus guidelines as a direct consequence of a lack of insurance coverage. To address this increasing concern, the genetic counseling profession must advocate for improved coverage and reimbursement for genetic counseling services.
To our knowledge, the largest published study evaluating the longest time period of billing and reimbursement was published in 2017 using data from a single institution in South Dakota, a state requiring licensure. The study focused on comparing credentialing of genetic counselors by the 31 payers billed for 582 encounters over a 4-year period. This study excluded encounters where patients saw a physician on the same day, were self-pay, or were billed to Medicare/Medicaid. The authors suggest licensure may be the key to credentialing with commercial payers, thus leading to improved rates of coverage and reimbursement (Leonhard et al., 2017).
The necessity to assess the reimbursement patterns of CPT code 96040 was seen in New Jersey, a state requiring licensure. The purpose of this retrospective study was to evaluate coverage and reimbursement for CPT code 96040 at a regional perinatal center.
Using data from Rutgers Robert Wood Johnson Medical School (Rutgers-RWJMS) Perinatal Genetics Division from 2010 to 2018, this study evaluated coverage and reimbursement by individual payers for genetic counseling services billed under the licensed genetic counselor's NPI using CPT code 96040 billed as a professional fee. This is an outpatient setting located in New Brunswick, New Jersey. In addition, the study evaluated difference between Health Maintenance Organizations (HMO), Point of Service plan (POS), and Preferred Provider Organizations (PPO). We sought to determine whether there are differences between coverage and reimbursement of encounters billed to different commercial and Managed Care Medicaid payers. We also reviewed the trends in coverage of encounters billed to commercial and Managed Care Medicaid payers over the study period.
2 METHODS
2.1 Procedures
Rutgers-RWJMS Perinatal Genetics Division collected data from 2010 to 2018 using billing, coverage, and reimbursement information. The Institutional Review Board at Rutgers University established on 3/3/2010 that this study does not meet the regulatory definition of human subjects' research and does not require IRB approval. The data included billing using CPT code 96040 as a professional fee by ten licensed genetic counselors. Each patient encounter had a record of the amount charged, amount paid, amount adjusted, invoice balance, insurance type, and individual encounter time. ‘Self pay’ encounters were excluded from the analysis as these encounters were not billed to a third-party payer. Diagnosis code data were not available in this database. Thus, we were not able to determine if the indication for the consultation affected coverage and reimbursement.
2.2 Data analysis
Descriptive statistics were performed for three categories: Medicare/Medicaid, Managed Care Medicaid, and commercial insurance. For each category, we calculated how often encounters were covered and percent reimbursed.
3 RESULTS
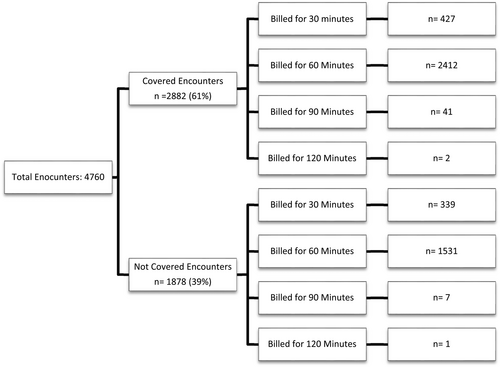
During the time period of April 2010 to May 2018, there were a total of 5,694 genetic counseling encounters. Of those, 934 fell into the ‘self pay’ category and were excluded from analysis. The data analysis was focused on the remaining 4,760 encounters. A total of 2,882 of the 4,760 (61%) encounters billed received coverage. Encounters were billed for 30, 60, 90, or 120 min, depending on the length of genetic counseling services provided.
Figure 1 showcases the coverage of the total billed 30-, 60-, 90-, and 120-min encounters. Of the 4,760 patient encounters, 766 encounters were billed for 30 min, 3,943 encounters were billed for 60 min, 48 encounters were billed for 90 min, and three encounters were billed for 120 min. As the majority of the encounters were billed for 60 min (82.8%), the remaining data analysis was limited to these 3,943 encounters.
The three main payer categories in our study were Medicaid/Medicare, Managed Care Medicaid, and commercial insurance. Of the 60-min encounters, 519 (13%) were billed to Managed Care Medicaid, 166 (4%) were billed to Medicaid/Medicare, and 3,258 (83%) were billed to commercial insurance. A total of 59% of encounters billed to Managed Care Medicaid and 65% of encounters billed to commercial insurance received coverage. None of the Medicaid/Medicare encounters were covered. Commercial insurance and Managed Care Medicaid reimbursed 38% and 23% of the amount billed, respectively (Table 1).
| Payer type | Total number of encounters (n) | % Encounters covered | Of covered encounters, % reimbursed of amount billed |
|---|---|---|---|
| Medicare/medicaid | 166 | 0% | 0% |
| Managed care medicaid | 519 | 59% | 23% |
| Commercial | 3,258 | 65% | 38% |
| Total | 3,943 | 61% | 36% |
We compared the rates of coverage for the four most common commercial insurance companies, which we labeled A, B, C, and D. These four companies represented a total of 2,825 encounters, which is 87% of total 60-min encounters billed to commercial payers. We then subdivided the rate of coverage for the individual plan types: Health Maintenance Organization (HMO), Point of Service (POS), or Preferred Provider Organization (PPO) (Table 2).
| Commercial Payer | Total number of encounters (n) | % Encounters covered | Average % reimbursed of the average amount billed | Health Maintenance Organization encounters (n) | % Health Maintenance Organization plan encounters covered | Point of Service plan encounters (n) | % Point of Service plan encounters covered | Preferred Provider Organization plan encounters (n) | % Preferred Provider Organization plan encounters covered |
|---|---|---|---|---|---|---|---|---|---|
| Company A | 706 | 81% | 32% | 124 | 68% | 299 | 82% | 283 | 85% |
| Company B | 1,459 | 66% | 41% | 60 | 67% | 322 | 57% | 1,077 | 68% |
| Company C | 263 | 86% | 39% | 74 | 93% | 109 | 87% | 80 | 78% |
| Company D | 395 | 51% | 40% | 45 | 62% | 187 | 47% | 163 | 52% |
| Total | 2,823 | 69% | 38% | 303 | 73% | 917 | 67% | 1,603 | 70% |
The following are the rates of coverage for encounters billed to each company: Company A (81%), Company B (66%), Company C (86%), and Company D (51%). Company B and Company D covered significantly less billed encounters than Company A and Company C. For the covered encounters, we then calculated the average rate of reimbursement for Company A (32%), Company B (41%), Company C (39%), and Company D (40%). When we tabulated the average amount reimbursed for each payer, Companies B, C, and D reimbursed essentially the same monetary amount. However, Company A reimbursed on average $27 less per covered encounter than Companies B, C, and D.
The rates of coverage for Companies A, B, C, and D were further broken down to the individual plan type: HMO, POS, and PPO. Company A covered encounters billed to POS and PPO plans at similar rates but covered significantly less encounters billed to an HMO plan. Company B covered encounters billed to all three plan types at similar rates. Company C covered encounters billed to HMO plans at a higher rate than those billed to a PPO plan. Company D followed a similar pattern to Company C (Table 2).
Our analysis included an extensive review of Company A–D's internal policies for genetic counseling services and testing. To avoid disclosing the identity of the Company A, Company B, Company C, and Company D, we have chosen not to discuss specific tenets of their internal guidelines or criteria.
The primary Managed Care Medicaid payers are Company E and Company F. Of the encounters billed to Company E and Company F, 44% and 86% received coverage, respectively. For the covered encounters, we then calculated the average rate of reimbursement for Company E (23%) and Company F (22%). When we tabulated the average monetary amount reimbursed for each payer, Companies E and F reimbursed essentially the same monetary amount (Table 3).
| Managed Care Medicaid payer | Total number of encounters (n) | % Encounters covered | Of covered encounters, % reimbursed of amount billed |
|---|---|---|---|
| Company E | 328 | 44% | 23% |
| Company F | 176 | 86% | 22% |
| Total | 504 | 59% | 22% |
The trends in coverage and reimbursement over the assessed 8 years were evaluated based on payer type. Figure 2 depicts the percentage of coverage for all 60-min encounters per year investigated. The highest percentage of coverage was in 2011 (73%) while the lowest percentage was in 2015 (46%). An overall downward trend was appreciated.
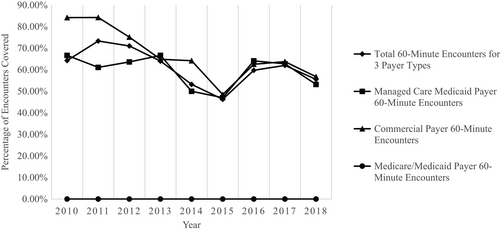
For the 3,258 60-min encounters billed to commercial payers, there was an overall downward trend as 84% of encounters were covered in 2010 and only 57% were covered in 2018. The lowest rate of coverage was in 2015 (48%), and the highest rate of coverage was in 2010 and 2011 (84%). For the 519 60-min encounters billed to Managed Care Medicaid payers, there was an overall downward trend as 67% of encounters were covered in 2010 and only 53% were covered in 2018. The lowest rate of coverage was in 2015 (47%), and the highest rate of coverage was in 2010 and 2013 (67%).
4 DISCUSSION
We found the coverage and reimbursement of encounters billed under CPT code 96040 as a professional fee are both inconsistent across payer types and within the individual payers. It is important to recognize the overall fees collected are not limited to insurance reimbursement but include co-pays, co-insurance, and deductibles. Thus, these data do not fully reflect the fees collected by the clinical institution for genetic counseling services. Rather these data are meant to reflect coverage and reimbursement trends by different payers. The CPT code 96040 is billed as a professional fee at this institution. To our knowledge, this is the largest study to date, which includes the longest duration of time and largest sample size.
Between the total 2,412 60-min encounters covered by either Medicare/Medicaid, Managed Care Medicaid, or commercial payers, there was a notable lack of consistency. Our primary hypothesis to explain the lack of consistent coverage is that commercial payers generally do not credential genetic counselors, which bars the billing of genetic counseling services at an in-network rate. Rutgers Robert Wood Johnson Medical School approached Companies A, B, C, and D to obtain credentialing for its licensed genetic counselors; however, none of the companies were able to credential genetic counselors as there was no precedence nor mechanism in place to do so. Given this, only Company A granted Rutgers-RWJMS licensed genetic counselors ‘preferred provider’ status. This allowed genetic counseling services billed under CPT code 96040 as a professional fee to be applied to a patient's in-network benefit—a process akin to credentialing. As a result, Company A was able to cover 81% of 60-min encounters billed to their plans. If the other studied commercial payers recognized genetic counselors in a similar manner, we predict an increase in the consistency of coverage for encounters billed under CPT code 96040.
Encounters billed to commercial insurance in this study were covered at 65%, similarly to the 62.6% of encounters covered reported by Gustafason et al. and 52.75% of encounters covered reported by Leonhard et al. However, there is incongruence between the rate of coverage between the studied commercial payers. Of the 60-min encounters billed to commercial insurance, Company C covered at the highest rate (86%) and Company D covered at the lowest rate (51%). Of the total encounters billed to commercial payers, only 9.3% were billed to Company C whereas 51.7% of encounters were billed to Company B, which can skew the data. Of the covered encounters, the percentage reimbursed of the amount billed ranged from 32% to 41% between the four commercial payers. These percentages are like those reported by Harrison et al. in 2009 (10%–71%) and Leonhard et al. in 2017 (42.44%).
When comparing the rates of coverage between the four commercial payers, Companies A and C covered 81% and 86% of encounters, respectively, while Companies B and D only covered 66% and 51% of encounters, respectively. This could be a direct outcome of Companies A and C having incorporated genetic counselors into their workflow whereas Companies B and D did not. Company A recognized the licensed genetic counselors included in the study as ‘preferred providers’ allowing CPT code 96040 billed a professional fee to be applied to a patient's in-network benefit. Although Company C did not credential or recognize the licensed genetic counselors as preferred providers, it is possible their specific internal guidelines and criteria promoted the coverage of genetic counseling services. Companies B and D have internal guidelines regarding genetic counseling services, but neither company credentialed nor recognized the licensed genetic counselors as preferred providers when approached by Rutgers-RWJMS. Given this information, the infrastructures of Companies A and C can be considered as an example for other commercial payers to increase the rate of coverage via the implementation of credentialing or recommendation of genetic services prior to genetic testing.
At the onset of this study, we suspected the PPO plans to provide higher and more consistent rates of coverage than the POS and HMO plans across all commercial payers. However, we did not observe this trend, and our data do not support this assumption. We cannot conclude if one individual plan type would trend better or worse for coverage of billed encounters than other plan types as there was inconsistency between the individual payers. When comparing the amount reimbursed for encounters covered by commercial payers, the rate of reimbursement was poor and inconsistent. There was no correlation between the rate of reimbursement and the individual plan type.
Of the 60-min encounters billed to and covered by Managed Care Medicaid payers, Company E covered 44% of the encounter billed and Company F covered 86% of the encounters billed. To note, only 34.9% of encounters billed to Managed Care Medicaid payers were billed to Company F. This disparity between the sample sizes may be influencing observed difference in the rates of coverage.
During our eight-year study period, there was an overall downward trend in coverage of all 60-min encounters billed, regardless of payer type. The average percentage of 60-min encounters covered in 2010 was 72% while the average percentage of 60-min encounters covered in 2018 was 55%. The fluctuation in coverage for Managed Care Medicaid payers and commercial payers is exemplified in Figure 2 as there are unpredictable patterns of reimbursement between each year investigated. Between Managed Care Medicaid and commercial payers, the only demonstrated consistency is that 2015 had the lowest percentage of encounters covered at 47% and 48%, respectively. While it is unknown if an event within the studied institution or change in billing practice is responsible, the percentage of encounters covered was also trending downward in 2014.
While genetic counseling encounters are being covered and reimbursed, it is not at a predictable nor consistent rate. Companies A, B, C, D, E, and F on average are reimbursing 50% of the amount that was billed. These data do not support that there is a specific prediction, trend, or correlation between coverage and reimbursement of encounters billed to either commercial and Managed Care Medicaid Payers. This creates a significant barrier of access to patients as referrals for formal genetic counseling services are likely to increase with the growing role of genetics in medicine. Because research has shown genetic counselors order the most appropriate and cost-effective testing, payers could benefit from creating a clear infrastructure for the credentialing of genetic counselors and for the coverage and reimbursement of genetic counseling services via CPT code 96040. As coverage of genetic counseling services increases and becomes more consistent, the monetary amount reimbursed can increase via payer contract negotiations. The first step to addressing this widespread issue is the passage of the new bill that will replace the former H.R 3235, ‘Access to Genetic Counselor Services Act of 2019’.
As expected, none of the 166 Medicare or Medicaid encounters received coverage. This creates disparity in access to care between the beneficiaries of public and private payers. CMS beneficiaries often are a patient population with more limited personal resources whereas commercial insurance is typically offered as part of an employment package. As 30% of the New Jersey population are CMS beneficiaries (The Henry J. Kaiser Family Foundation, 2020), the given lack of coverage and associated out of pocket expenses for genetic counseling services creates a barrier to access for these beneficiaries. If genetic counselors were to be recognized as healthcare providers by CMS via passage of the next bill that will replace the former H.R 3235, ‘Access to Genetic Counselor Services Act of 2019’, genetic counseling encounters would be eligible for coverage, hence allowing beneficiaries affordable access.
This bill would require CMS to recognize genetic counselors as healthcare providers, hence making genetic counseling services billed under CPT code 96040 eligible for coverage. As a direct result, CMS beneficiaries would have significantly better access to medically necessary genetic counseling services. Even though most CMS beneficiaries may not use all specialties of genetic counseling, the passage of the next bill that will replace the former H.R. 3235 can set an example for private payers to credential genetic counselors and recognize CPT code 96040. In turn, the utility and financial benefit of genetic counselors coordinating testing can lower the overall burden on the healthcare system.
Patients should have access to affordable genetic counseling as a covered service to receive accurate risk assessment and targeted genetic testing. The next bill that will replace the former H.R 3235 will address the barrier of access to care for CMS beneficiaries and can serve as an example to private payers to increase consistency across payers. This study demonstrated inconsistency in genetic counseling services coverage and reimbursement via CPT code 96040 when billed as a professional fee. A lack of insurance coverage creates a barrier of access to care that discourages patients from accessing the genetic counseling services that can directly impact their care. To prevent this barrier from negatively impacting current and future patients, continued advocacy across all levels is critical beginning with increased support behind the passage of the next bill that will replace the former H.R 3235, ‘Access to Genetic Counselor Services Act of 2019’.
4.1 Study limitations
A limitation of this study is that we were not able to determine why a payer would reimburse for some encounters, but not others billed for the same amount. Differences in benefit coverage between patients receiving genetic counseling services may be an influencing factor. This study evaluated only one center and does not represent all states nor all perinatal center workflows and billing practices. The rates of reimbursement seen at any center can be directly influenced by their specific billing procedures. Diagnostic codes used when billing CPT code 96040 as a professional fee were not reviewed. It is possible some payers will provide coverage of the CPT code only if specific ICD-10 codes are used. As this information was not available, the impact of diagnostic codes could not be assessed. Analysis of the coverage and reimbursement data for 30-min encounters, 90-min encounters, and 120-min encounters were not included in this study. It is possible the coverage and reimbursement patterns can differ depending on how many units of CPT code 96040 are billed.
4.2 Research recommendations
This study can be expanded upon by evaluating the reimbursement of CPT code 96040 at different institutions offering reproductive genetic counseling services in states requiring licensure. If there is a statistically significant difference between the coverage rates or reimbursement amounts, a further comparison of billing procedures and ICD-10 codes can be completed. It would also provide insight to regional differences in reimbursement as different third-party payer companies may be assessed. Having nationwide data about the billing, coverage, and reimbursement of CPT code 96040 when billed as a professional fee would demonstrate the need for federal legislation. This study can also be completed in states without licensure to determine how licensure status affects the reimbursement of CPT code 96040. It would be expected that states without licensure would have lower levels of coverage as licensure is often required by third-party payers for credentialing. These data can be used to further demonstrate the need for genetic counselor licensure in those states. Further studies can be completed to better understand the downstream effect of improving trends in coverage and reimbursement of genetic counseling services. If this barrier of access to care is removed, there likely would be a marked increase in the number of patients seen and reimbursement provided to institutions. Given the increase in need, it is speculated that increased coverage of genetic counseling services may increase the number of genetic counselors employed by institutions to manage an increased patient load. A study can be carried out to observe the trends in employment of genetic counselors and the impact on the healthcare system in the wake of increased coverage and reimbursement of genetic counseling services. These research recommendations can provide novel data to expand upon the minimal public knowledge of coverage and reimbursement for genetic counseling services via CPT code 96040.
AUTHOR CONTRIBUTIONS
Francesca Spinosi, Elena Ashkinadze, Shama Khan, and Christine Seymour each fulfilled the International Committee of Medical Journal Editors criteria for authorship. Francesca Spinosi contributed to the conceptualization, formal analysis/data interpretation, methodology creation, investigation, visualization, and identification of resources for this study. She wrote the original draft and actively reviewed and revised additional drafts. Elena Ashkinadze contributed to the conceptualization, data curation, formal analysis/data interpretation, methodology creation, and supervision for this study. She assisted in writing the original draft and reviewed and revised additional drafts. Shama Khan contributed to the conceptualization, data curation, project administration, and supervision of this study in addition to reviewing and revising drafts. Christine Seymour participated in the conceptualization and supervision of this study in addition to reviewing and revising drafts. Authors Francesca Spinosi and Elena Ashkinadze confirm that they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All of the authors gave final approval of this version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ACKNOWLEDGEMENTS
This research was conducted to fulfill a degree requirement for the Rutgers University Genetic Counseling Master's Program, and the authors are grateful for this program's support. The research presented in this document was made possible by the support of the genetic counselors working at the Division of Maternal Fetal Medicine in the Department of Obstetrics and Gynecology at Rutgers Robert Wood Johnson Medical School.
COMPLIANCE WITH ETHICAL STANDARDS
CONFLICT OF INTEREST
Francesca Spinosi, Elena Ashkinadze, Shama Khan, and Christine Seymour declare that they have no conflict of interest.
HUMAN STUDIES AND INFORMED CONSENT
The Institutional Review Board at Rutgers University determined on March 3, 2010, that this application does not meet the regulatory definition of human subjects research and does not require IRB approval.
ANIMAL STUDIES
No non-human animal studies were carried out by the authors for this article.
DATA SHARING AND DATA ACCESSIBILITY
The data that support the findings of this study are available on request as they are not publicly available due to privacy or ethical restrictions.