Alternative option labeling impacts decision-making in noninvasive prenatal screening
Abstract
Prenatal genetic screening should be an informed, autonomous patient choice. Extrinsic factors which influence patient decision-making threaten the ethical basis of prenatal genetic screening. Prior research in the area of medical decision-making has identified that labeling may have unanticipated effects on patient perceptions and decision-making processes. This Internet-administered study explored the impact of option labeling on the noninvasive prenatal screening (NIPS) selections of US adults. A total of 1,062 participants were recruited through Amazon Mechanical Turk (MTurk) and randomly assigned to one of three possible label sets reflecting provider-derived and industry-derived option labels used in prenatal screening. Multinomial logistic regression analysis showed option labeling had a statistically significant impact on the NIPS selections of study participants (p = .0288). Outcomes of the Satisfaction with Decision Scale (SWD) indicated option labels did not play a role in participant satisfaction with screening selection. The results of this study indicate a need for further evaluation of the impact NIPS option labeling has on patient screening decisions in real-world clinical interactions. Clinical providers and testing laboratories offering NIPS should give careful consideration to the option labels used with prenatal screening so as to minimize influence on patient screening selection and decision-making processes.
1 INTRODUCTION
Noninvasive prenatal screening (NIPS) options for women and expectant couples have expanded with advances in the molecular analysis of circulating cell-free fetal DNA (cffDNA). Current NIPS options include evaluation for fetal aneuploidies, subchromosomal abnormalities, and more recently, monogenic disorders (Liu, Li, Fu, Chung, & Zhang, 2016). With the anticipated introduction of noninvasive prenatal whole genome sequencing (PWGS) into clinical practice, providers and patients may soon be navigating an even broader range of available screening options (Allen Chan et al., 2016; Bayefsky et al., 2016; Drury, Hill, & Chitty, 2016).
In addition, reference to screening options differs by provider and clinical setting. Genetic counselors may utilize colloquial or descriptive option labels to tailor complex information for patients in need of additional decision-making support (Farrell, Hawkins, Barragan, Hudgins, & Taylor, 2015; Floyd, Allyse, & Michie, 2016; Hibbard & Peters, 2003; Korngiebel et al., 2016; Lubitz et al., 2007). For instance, Korngiebel et al. (2016) sought input from patient focus groups in developing categorical option labels for preconception carrier testing. The resulting options labels, short phrases such as ‘conditions with significantly shortened life span’ or ‘conditions with unpredictable outcomes’, were meant to assist patients in drawing easy distinctions between the disorders available for testing. Furthermore, industry test menus often utilize trademarked NIPS option labels in patient and promotional materials. As a result, these industry-derived option labels may be introduced to patients alongside provider-derived option labels in clinical interactions.
Evidence suggests labels impact patient decision-making in other areas of prenatal screening. A study by Zikmund-Fisher, Fagerlin, Keeton, and Ubel (2007) found that when identical quantitative prenatal screening results were augmented with interpretive labels implying specific findings (e.g., ‘Positive’, ‘Abnormal’), women were more likely to perceive a greater risk for fetal aneuploidy and express intent to proceed with invasive diagnostic procedures; in contrast, women perceived lower risk with more neutral labels (e.g., ‘Negative’ ‘Normal’) or no additional labels. While this study examined labeling within the context of quantitative results, it highlights the potential for labels to alter patient perceptions or behaviors related to prenatal screening. As seen in other fields, labels providing contextual information about available options may have unanticipated effects on decision-making (Dolan, Cherkasky, Chin, & Veazie, 2015), or even be purposefully manipulated to encourage certain selections or behaviors (Ho, Shih, & Walters, 2012; Morris, Carranza, & Fox, 2008).
Informed, autonomous patient decision-making is crucial to the ethical practice of genetic screening. This is particularly relevant within the prenatal context given the potential for increased screening options and complex results to complicate patient decision-making and critically impact reproductive outcomes. Therefore, because the study of labeling in other areas of prenatal screening suggests labels influence decision-making processes and behavioral intent, it is imperative to study empirically the implication of NIPS option labels on patient screening selection. We conducted an experimental study in which adult Internet-users participating in an online survey randomly received one of three possible label sets describing NIPS options in a hypothetical prenatal screening menu. Label sets included technical language or a combination of industry- and provider-derived labels to reference included NIPS options. This design allowed us to assess the effect of differing NIPS option labels on two outcome variables: (a) participant NIPS selection and (b) the reported decisional confidence of participants.
2 METHODS
2.1 Participants
Participants were US adults recruited through Amazon Mechanical Turk (MTurk), a crowdsourcing platform which connects researchers and developers with Internet-users willing to complete ‘human intelligence tasks’ (HITs), that is, tasks which cannot be performed by computational analysis. MTurk ‘workers’ are considered to be more heterogeneous than traditional survey samples, having greater demographic and occupational diversity (Buhrmester, Kwang, & Gosling, 2011; Cheung, Burns, Sinclair, & Sliter, 2016). Inclusion criteria considered (a) residency within the United States, (b) age between 18 and 50 years (i.e., within reproductive range), and (c) an approval rating of 95% or greater for previously completed HITs. Peer, Vosgerau, and Acquisiti (2014) have suggested MTurk HIT approval ratings are a sufficient means for ensuring high-quality data and participant attentiveness.
Unique MTurk worker-ID numbers were used to screen out duplicate respondents. Additionally, submissions were rejected if participants (a) spent less than 90 s completing the survey or (b) did not provide a valid survey completion code.
The HIT posting viewed by MTurk workers described the online survey as a ‘Survey of Medical Decision-Making for Health Screening’. This general description was used to prevent the selection of participants with strong attitudes toward prenatal screening for genetic conditions. Participants were compensated $0.75 consistent with reimbursement rates for MTurk surveys estimated at 90–180 s in length. This study was approved by the University of Wisconsin-Madison Institutional Review Board (IRB# 00038065).
2.2 Procedures
To begin, participants were directed to a clinical vignette outlining a hypothetical scenario in which they are a pregnant woman, or the partner of a pregnant woman, speaking with their healthcare provider. The provider discusses general information about NIPS and reviews that NIPS is performed using a single maternal blood draw. To reduce the impact of monetary concerns on decision-making for this study, the vignette additionally clarifies that the full cost of screening will be covered by health insurance.
Identical information was presented to all participants about the following NIPS options: (a) NIPS for select aneuploidies, (b) combined NIPS for select aneuploidies and genome sequencing (i.e., PWGS), and (c) an option to decline screening listed as ‘No Screening’ across all three experimental groups. Included screening options were meant to reflect the most widely accessible NIPS option (i.e., screening for select aneuploidies), as well as consider future directions for NIPS (i.e., PWGS). Screening options were restricted in this study design to maintain the clarity of the experimental manipulation (Figure 1).
The sole difference between experimental groups was NIPS option labels used to reference available screening throughout the vignette and testing menu (Table 1). With this manipulation, we investigated the impact of differing option labels on the relative proportion of participants selecting each NIPS option and participant decisional satisfaction across experimental groups.
| Screening options | Label set A | Label set B | Label set C |
|---|---|---|---|
| No screening | No screening | No screening | No screening |
|
Select aneuploidies Trisomy 13, trisomy 18, trisomy 21 |
Trisomy screening | Core screening | Traditional screening |
|
Select aneuploidies + sequencing Trisomy 13, trisomy 18, trisomy 21 + >5,000 health conditions |
Sequencing + trisomy screening | Comprehensive screening | Global screening |
Using a survey randomizer tool, participants were randomly assigned to one of three unique label sets designed by the research team and intended to reflect current language used in the area of prenatal screening and preconception genetic testing. Label Set A (‘Trisomy Screening’ and ‘Sequencing + Trisomy Screening’) presented screening options with objective, technical language meant to reduce contextual information about screening options. In the absence of this contextual information, we anticipated participants assigned Label Set A would encounter greater difficulty making screening selections consistent with their values and possibly lower their level of decisional satisfaction.
Label Set B (‘Core Screening’ and ‘Comprehensive Screening’) drew directly from labels and colloquial terms used clinically or derived from industry marketing materials. The ‘Core Screening’ option label, referring to NIPS for select aneuploidies, was derived from the current test menu and marketing materials of Sequenom's MaterniT21 PLUS (Sequenom, 2017). Sequenom uses the ‘core’ label with their current noninvasive prenatal aneuploidy screening. The research team coined ‘Comprehensive Screening’ as the corresponding combined NIPS for select aneuploidies and PWGS label. After reviewing existing NIPS menus and considering a variety of different terms, the research team elected the colloquial term ‘comprehensive’ as it was felt to adequately contextualize the breadth of screening included in the combined NIPS option. This term was felt to be additionally appropriate as Merriam-Webster's online thesaurus lists ‘comprehensive’ under the correlative term (‘global’) used in Label Set C.
Label Set C (‘Traditional Screening’ and ‘Global Screening’) was derived in a similar fashion as Label Set B. The ‘Traditional Screening’ label was elected by the research team for the NIPS for select aneuploidies option. The colloquial term ‘traditional’ was determined appropriate as screening for Trisomy 13, Trisomy 18, and Trisomy 21 has historically been offered in this area of prenatal genetic counseling. Additionally, the term ‘traditional’ has been utilized in industry educational materials to reference maternal serum screening – a prenatal screen for limited fetal aneuploidies (Ariosa Diagnostics, 2016). The combined NIPS for select aneuploidies and PWGS option was labeled as ‘Global Screening’, a term appropriated from Progenity's Preparent Global Carrier Screening Panel (Progenity, 2017). Carrier screening panels, such as Progenity's, look broadly for genetic conditions with variable severity and a wide range of clinical features – similar to the combined NIPS for select aneuploidies and PWGS option. For this reason, current industry labels for carrier testing were considered appropriate correlates for the combined option in this study.
In all, we hypothesized that the colloquial and industry-derived option labels in Label Sets B and C would act as potential sources of decision-making support by providing contextual information about the screening options. We hypothesized contextual labels would allow participants to better select screening most in line with their personal values and preferences, thereby increasing decisional satisfaction for participants assigned Label Sets B and C.
2.3 Measures
The instrument for data collection in this study was a 23-item survey developed by the research team to evaluate the impact of differing option labels (referencing identical NIPS options) on respondent screening selection. Participants were first presented with a short vignette providing relevant clinical background and information about NIPS. Two NIPS options and an option to decline screening (‘No Screening’) were displayed as part of a hypothetical test menu; respondents were asked to select one of the three screening options. Screening selection was the primary measure of this study. Participants opting for screening were directed to describe how they came to a decision between the available NIPS options in a free-text box. Study participants who selected the ‘No Screening’ option were asked to briefly explain their reasons for declining screening. Participant satisfaction with screening selection was assessed using an abbreviated version of the Satisfaction with Decision (SWD) scale developed by Holmes-Rovner et al. (1996). This adapted survey tool asked participants to indicate their level of agreement with several statements using a five-item Likert scale ranging from ‘Strongly Agree’ to ‘Strongly Disagree’. In addition, participants answered a series of multiple-choice questions intended to gather demographic information, including age, race, gender, marital status, education level, current religious practice, and political views. Finally, multiple-choice questions were utilized to assess participant experience with pregnancy and prenatal genetic counseling. The full text for both the clinical vignettes and survey may be found in the Supplemental Materials for this study (SM1–SM4).
2.4 Data analysis
We reported descriptive statistics, such as counts and percentages. Additionally, we conducted Chi-squared and Fisher's Exact Tests to look for relationships between categorical variables. To examine the influence of option labeling on participant screening selection, we completed multinomial logistic regression analyses while adjusting for demographic variables through the use of stepwise selection methods. All collected demographic variables (Table 2) were considered in the stepwise selection methods for multinomial logistic regression analysis. We conducted all statistical analyses with the use of SAS (SAS Analytics, Version 9.4). Results with a p ≤ .05 were considered significant.
| Characteristic |
Label set A (N = 351) N (%) |
Label set B (N = 354) N (%) |
Label set C (N = 357) N (%) |
|---|---|---|---|
| Age* | |||
| 18–35 years | 259 (74%) | 222 (63%) | 255 (71%) |
| 36 years and older | 92 (26%) | 132 (37%) | 102 (29%) |
| Gender | |||
| Male | 191 (55%) | 200 (57%) | 187 (52%) |
| Female | 157 (45%) | 153 (43%) | 170 (48%) |
| Race | |||
| White | 275 (79%) | 277 (79%) | 295 (83%) |
| African American | 27 (8%) | 27 (8%) | 24 (7%) |
| Asian | 33 (9%) | 26 (7%) | 24 (7%) |
| Other | 14 (4%) | 19 (5%) | 12 (3%) |
| Marital status | |||
| Married/Domestic Part. | 152 (43%) | 171 (49%) | 178 (50%) |
| Single | 181 (52%) | 157 (45%) | 150 (42%) |
| Other | 18 (5%) | 22 (6%) | 27 (8%) |
| Education level | |||
| Graduate/ prof. degree | 29 (8%) | 48 (14%) | 42 (12%) |
| Bachelor/assoc. degree | 280 (80%) | 272 (77%) | 271 (76%) |
| High school/GED | 42 (12%) | 33 (9%) | 43 (12%) |
| Religious practice | |||
| Christian | 65 (19%) | 80 (23%) | 95 (27%) |
| Protestant Christian | 30 (9%) | 32 (9%) | 30 (8%) |
| Roman Catholic | 34 (10%) | 29 (8%) | 27 (8%) |
| Latter Day Saints (Mormon) | 2 (<1%) | 3 (<1%) | 3 (<1%) |
| Muslim | 2 (<1%) | 3 (<1%) | 4 (1%) |
| Jewish | 6 (2%) | 7 (2%) | 4 (1%) |
| Buddhist/Taoist | 3 (<1%) | 8 (2%) | 6 (2%) |
| Hindu | 2 (<1%) | 1 (<1%) | 1 (<1%) |
| Spiritual (no particular faith) | 53 (15%) | 48 (14%) | 57 (16%) |
| Secular | 81 (23%) | 66 (19%) | 50 (14%) |
| Other | 55 (16%) | 55 (16%) | 59 (17%) |
| Do not wish to report | 18 (5%) | 20 (6%) | 21 (6%) |
| Political views | |||
| Liberal | 187 (53%) | 173 (50%) | 167 (47%) |
| Moderate | 88 (25%) | 99 (28%) | 97 (27%) |
| Conservative | 76 (22%) | 76 (22%) | 90 (26%) |
| Previously pregnant/fathered a child | |||
| Yes | 115 (33%) | 144 (41%) | 134 (38%) |
| No | 234 (67%) | 206 (59%) | 218 (62%) |
| Pregnant at the time of survey | |||
| Yes | 6 (2%) | 14 (4%) | 9 (3%) |
| No | 343 (98%) | 337 (96%) | 344 (97%) |
| Prior prenatal genetic counseling | |||
| Yes | 32 (9%) | 41 (12%) | 38 (11%) |
| No | 309 (89%) | 305 (87%) | 302 (85%) |
| Not sure | 7 (2%) | 4 (1%) | 14 (4%) |
- a N may vary due to missing data (percentage missing data for all variables ≤1%).
- * χ2 = 11.3 (2), p = .0035.
3 RESULTS
A total of 1,188 participants submitted survey responses during a 3-week period in February 2017. Exclusion criteria reduced the number of responses analyzed to 1,062. Survey participants were predominantly men (54.4%), Caucasian (79.9%) and without a pregnancy history for either themselves or their partners (61.9%). The majority (69.3%) reported an age within the range of 18–35 years and approximately half (51.7%) cite a bachelor's or graduate level college degree. A modest number of participants (10.5%) had previously received prenatal genetic counseling. At the time of this survey, 2.7% of participants indicated that they or their partner were currently pregnant. Participant age was identified as the single demographic which significantly differed among experimental groups (χ2 (2) = 11.3, p = .0035). Table 2 describes the complete details of participant characteristics across experimental groups.
Participant prenatal screening selections are presented in Table 3. Overall, study participants overwhelmingly preferred the combined screening option (69.8%) which included both NIPS for select aneuploidies and PWGS. Chi-squared analysis identified significant differences between the screening selections of participants randomized to Label Set A, B, or C (χ2 (4) = 12.7, p = .0126). After controlling for all other variables between experimental groups, multinomial logistic regression analysis confirmed that option labeling had a significant impact on prenatal screening selection (p = .0288)1 (Table 4). When comparing the screening selections of participants randomized to Label Sets B and C (i.e., label sets thought to provide contextual information about available NIPS options), participants assigned Label Set C were more likely to select NIPS for select aneuploidies over declining screening or the combined NIPS option (p < .05). Of the participants randomized to Label Sets A and C who opted for prenatal screening, those receiving Label Set C were more likely to select NIPS for select aneuploidies while those receiving Label Set A were more likely to select the combined NIPS option (OR = 0.566, CI = (0.376, 0.854), p < .01). Odds ratio pairwise comparisons did not demonstrate statistical significance when comparing the screening selections of participants randomized to Label Sets A and B.
| Screening choice | Label set A | Label set B | Label set C | Total |
|---|---|---|---|---|
| No screening | 44 (13%) | 56 (16%) | 42 (12%) | 142 |
| Select aneuploidies | 49 (14%) | 51 (14%) | 79 (22%) | 179 |
| SA + sequencing | 258 (74%) | 247 (70%) | 236 (66%) | 741 |
| Total | 351 | 354 | 357 | 1,062 |
Note
- χ2 = 12.7, df = 4, p = .0126; Fisher's Exact Test: p = .0154.
- Abbreviation: SA, select aneuploidies.
| Variable |
Aneuploidy versus no screening OR (95% CI) |
SA + sequencing versus no screening OR (95% CI) |
SA + sequencing versus no aneuploidy OR (95% CI) |
p-value |
|---|---|---|---|---|
| Label set | ||||
| Label set B versus A | 0.870 (0.485. 1.561) | 0.798 (0.498, 1.278) | 0.917 (0.590, 1.424) | .0288 |
| Label set C versus A | 1.686 (0.943, 3.014) | 0.955 (0.582, 1.567) | 0.566 (0.376, 0.854)** | |
| Label set C versus B | 1.938 (1.108, 3.390)* | 1.197 (0.745, 1.924) | 0.618 (0.411, 0.929)* | |
| Political views | ||||
| Moderate versus liberal | 0.587 (0.526, 1.055) | 0.414 (0.251, 0.681) | 0.705 (0.472, 1.053) | <.0001 |
| Conservative versus liberal | 0.351 (0 198, 0.623)*** | 0.205 (0.127, 0.331)**** | 0.584 (0.379, 0.900)* | |
| Conservative versus moderate | 0.599 (0.333, 1,077) | 0.496 (0.307, 0.802)** | 0.829 (0.518, 1.328) | |
| Previously pregnant/fathered a child | ||||
| Yes versus no | 0.292 (0 175, 0 488) **** | 0.229 (0.151, 0.346)**** | 0.782 (0.520, 1.177) | <.0001 |
| Prior prenatal genetic counseling | ||||
| Yes versus no | 4.062 (1.780, 9.267)*** | 4.457 (2.195, 9.051)**** | 1.097 (0.609, 1.976) | .0002 |
- Abbreviation: SA, select aneuploidies.
- * p < .05,
- ** p < .01,
- *** p < .001,
- **** p < .0001
Multinomial logistic regression analysis identified certain demographic characteristics significantly associated with participant prenatal screening selections including participant political views, prior experience with prenatal genetic counseling and pregnancy history. Participants with a pregnancy history or participants who have fathered children were more likely to decline screening compared to participants without a pregnancy history (p < .0001). Additionally, study participants who previously received prenatal genetic counseling services were more likely to pursue either available NIPS option (select aneuploidies: OR = 4.062, CI = (1.780,9.267), p < .001; select aneuploidies and PWGS: OR = 4.457, CI = (2.195,9.051), p < .0001). Participants identifying as politically conservative were more likely to decline screening when compared with participants identifying as politically liberal (select aneuploidies: OR = 0.351, CI = (0.198, 0.623), p < .001; select aneuploidies and PWGS: OR = 0.205, CI = (0.127, 0.331), p < .0001). Additionally, when comparing conservative and liberal participants who opted for screening, conservatives were significantly more likely to select NIPS for select aneuploidies (p < .01).
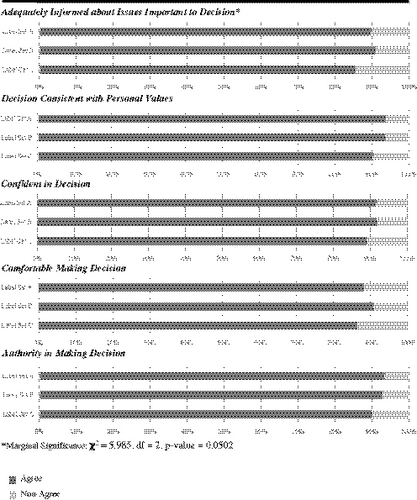
Outcomes of the SWD scale are shown in Figure 2. Participants randomized to Label Set C were less likely to report feeling adequately informed about factors important to their decision-making (marginal significance: χ2 (2) = 5.985, p = .0502). Responses to all other SWD scale measures did not differ significantly across experimental groups.
As the name indicated, the comprehensive screening is the more [broad] scan, and will detect more potential problems.
I don’t want to overly worry, but I do want to know if my baby will have a core issue.
I choose the traditional screening because I am a traditional kind of person who sees the risk of a defect is [too] low to try a different procedure.
I don’t trust the global screening… Traditional has been around for some time, so it’s more acceptable.
I did not want to take any chances with my [partner’s] or the baby’s health. The core option was safe.
4 DISCUSSION
The results of this study indicate that option labeling should be considered as a factor that significantly impacts the prenatal screening selections of adults. How providers reference NIPS options is one potential source of decisional influence which has been little explored, and therefore, careful evaluation of the language used in option labeling is a pertinent consideration in the preservation of client autonomy in prenatal screening decisions.
Odds ratio pairwise comparisons including Label Set C indicate participants viewing the ‘Traditional Screening’ label for NIPS for select aneuploidies were significantly influenced to select this option. In addition, odds ratio pairwise comparisons indicated participants assigned to Label Set A were more likely to select the combined NIPS for select aneuploidies and PWGS option (‘Sequencing + Trisomy Screening’). This preference may be explained by the presence of a ‘+’ sign and two labels (‘Sequencing’ and ‘Trisomy Screening’) which could imply the combined NIPS option is superior because of an assumption that more screening is better.
The overwhelming interest among study participants in the combined NIPS for select aneuploidies and PWGS option suggests women and expectant couples will increasingly seek emerging NIPS technologies. Novel NIPS options are typically introduced into clinical settings via testing laboratories. Laboratory patient and promotional materials proliferate the use of industry-derived option labels which should be considered as a prospective source of decision-making influence. As seen with this study, industry-derived terminology has the potential to impact clinical prenatal screening decisions. Consumer-driven advertising additionally creates the potential for patient attachment to industry-derived labels which may impact meaningful evaluation of screening options in a clinical setting.
Option labels for prenatal screening may have the ability to communicate information about decision-relevant option attributes. In addition, there is a potential for option labels to activate social identities, making them more salient in decision-making processes. Morris et al. (2008) found that individuals reminded of their Republican political affiliation were more likely to select financial options labeled as ‘conservative’ risk – an effect that was not seen when financial options were unlabeled. Participant political views were identified in this study to significantly affect screening selection. Therefore, terms or labels which trigger this social identity may have considerable effects on decision-making.
Additionally, the results of this study identified that individuals with a pregnancy history are less likely to consider NIPS options of any kind. This suggests that experience with pregnancy or childrearing provides a greater appreciation of the potential for increased information to create anxiety or contribute to further uncertainty about the health of a child. Furthermore, prior genetic counseling was associated with increased uptake of prenatal screening. This finding suggests that there may be differences in the screening intentions of individuals familiar with prenatal genetic counseling compared with those who are not.
Overall, high decisional satisfaction was reported across experimental groups. Outcomes of the SWD scale provide assurance that participants in this study felt informed and confident about their decisions regardless of any decisional influence exerted by extrinsic factors. However, considering all available NIPS options within the context of a real-world prenatal screening decision would undoubtedly complicate patient decision-making. The comparatively fewer screening options offered to study participants may have contributed to the high levels of decisional satisfaction reported.
4.1 Study limitations
A primary limitation of this study is the use of a non-patient population making hypothetical prenatal screening decisions. Use of a hypothetical clinical scenario may fail to induce emotions or decision-making processes which exist in a true prenatal patient population. The internal validity of our randomized experimental design suggests option labels significantly impact the prenatal screening selections of US adults. However, our clinical vignette did not include the full range of prenatal screening alternatives, their respective quantitative parameters, or simulate the actual emotional context of real-world screening selection.
In addition, significant variations in participant age between experimental groups was considered a limiting factor for this study. Theoretically, randomized experimental design should ensure an even distribution of participant characteristics across conditions. However, this was not the case for the reported age of respondents. Multinomial logistic regression analysis did not find that age significantly contributed to participant screening selection and therefore this variance is expected to be of limited impact.
As another limitation of this study, the administered survey did not explicitly assess participant understanding of prenatal screening or the presented screening options by use of a validated measure. This would be a valuable area for future study given the hypothesis that contextual labels allowed participants to more readily access decision-relevant option attributes.
4.2 Practice implications
There is a potential for option labeling to impact patient decision-making in prenatal screening selection and over-ride other more deliberative decision-making processes facilitated by genetic counselors. Further assessment and provider education about the impact of option labels on patient decision-making should be considered. Additionally, exploration of the labels used in industry materials and consumer-driven advertising is warranted and careful consideration should be given to the use of industry materials in clinical interactions.
4.3 Research recommendations
One important direction for future study would be to examine how various providers reference screening options in clinical interactions so as to determine the frequency with which colloquial, provider-derived, or industry-derived labels are used in prenatal screening discussions. Additionally, patient-directed surveys or focus groups may further clarify option labels which assist patients in making screening selections congruent with their values, and labels which may unduly influence patient decision-making processes.
5 CONCLUSIONS
Providers have a responsibility to promote informed, autonomous decision-making for patients considering prenatal screening or testing. As seen in this study, labeling of prenatal screening options ultimately impacts screening selection. Acknowledging, and further evaluating, the significant influence of labeling on screening selection is essential for the development of appropriate practice guidelines and conscientious integration of novel screening technologies into the clinical realm.
AUTHOR CONTRIBUTIONS
C.F.F. and L.E.B. conceived of the presented concept and designed the experiment. C.A.R. and E.M.P. coordinated and supervised the experimental design and data collection. B.J.Z.F. and C.G.S.P. contributed to the design and implementation of the research and to the analysis of results. Q.Z. performed the calculations and verified the analytical methods. C.F.F. wrote the manuscript in consultation with B.J.Z.F. and C.G.S.P. All authors helped shape the research, analysis, and manuscript by providing critical feedback.
ACKNOWLEDGMENTS
This work was performed in partial fulfillment of the first author's master's thesis requirement. This research received funding from the University of Wisconsin Genetic Counseling Program Research Fund. We would like to acknowledge the Department of Biostatistics and Medical Informatics for assisting with data analysis. Dr. Melanie Myers served as Editor on the manuscript review process and publication decision.
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of interest
Authors C.F.F., L.E.B., C.A.R., Q.Z., C.G.S.P., B.J.Z.F., and E.M.P. declare they have no conflict of interest. No author will derive any personal profit or gain, directly or indirectly, by involvement with this project.
Human studies and informed consent
This study was granted exemption from University of Wisconsin – Madison Institutional Review Board (IRB# 00,038,065). Participation in the online survey was voluntary and participant responses remained anonymous.
Animal studies
No non-human animal studies were carried out by the authors for this article.