Inorganic phosphate enhances sensitivity of human osteosarcoma U2OS cells to doxorubicin via a p53-dependent pathway
Abstract
Osteosarcoma is the most common malignant primary bone tumor in children and adolescents. The clinical outcome for osteosarcoma remains discouraging despite aggressive surgery and intensive radiotherapy and chemotherapy regimens. Thus, novel therapeutic approaches are needed. Previously, we have shown that inorganic phosphate (Pi) inhibits proliferation and aggressiveness of human osteosarcoma U2OS cells identifying adenylate cyclase, beta3 integrin, Rap1, ERK1/2 as proteins whose expression and function are relevantly affected in response to Pi. In this study, we investigated whether Pi could affect chemosensitivity of osteosarcoma cells and the underlying molecular mechanisms. Here, we report that Pi inhibits proliferation of p53-wild type U2OS cells (and not of p53-null Saos and p53-mutant MG63 cells) by slowing-down cell cycle progression, without apoptosis occurrence. Interestingly, we found that Pi strongly enhances doxorubicin-induced cytotoxicity in U2OS, and not in Saos and MG63 cells, by apoptosis induction, as revealed by a marked increase of sub-G1 population, Bcl-2 downregulation, caspase-3 activation, and PARP cleavage. Remarkably, Pi/doxorubicin combination-induced cytotoxicity was accompanied by an increase of p53 protein levels and of p53 target genes mdm2, p21 and Bax, and was significantly reduced by the p53 inhibitor pifithrine-alpha. Moreover, the doxorubicin-induced cytotoxicity was associated with ERK1/2 pathway inhibition in response to Pi. Altogether, our data enforce the evidence of Pi as a novel signaling molecule capable of inhibiting ERK pathway and inducing sensitization to doxorubicin of osteosarcoma cells by p53-dependent apoptosis, implying that targeting Pi levels might represent a rational strategy for improving osteosarcoma therapy. J. Cell. Physiol. 228: 198–206, 2013. © 2012 Wiley Periodicals, Inc.
Abbreviations:
cAMP, 3′-5′-cyclic adenosine monophosphate; PKA, protein kinase A; ERK, extracellular signal-regulated kinases; MAPK, mitogen-activated protein kinases; MEK-1, mitogen-activated kinase kinase; Rap1, Ras-associated protein-1; Epac, exchange proteins activated by cAMP; Pi, inorganic phosphate; GSTP1, human glutathione S-transferase P1; Bcl2, B-cell lymphoma 2; Bax, Bcl-2-associated X protein; mdm2, murine double minute 2; PARP, poly-(ADP-ribose) polymerase; DDTD, 3′,4′-dichloro-3-(3,4-dichlorophenylacetyl)-2,4,6-trihydroxydeoxybenzoin.
Osteosarcoma is the most common primary malignant tumor of bone, occurring most frequently in children and adolescents (Chou et al., 2008). Surgery, radiotherapy, and high-dose chemotherapy (with agents such as doxorubicin, methotrexate, cisplatin, etoposide, and ifosfamide) are mainly effective in patients with localized disease and have improved overall survival over the last several years (Dai et al., 2011).
However, clinically evident metastatic disease is present in 10–20% of patients at diagnosis. Despite aggressive treatment, more than one-third of patients develop recurrent high-grade osteosarcomas, with metastatic disease typically affecting the lung, liver, and bone itself, so that the 5-year survival rates are still not more than 60%. The frequent acquisition of drug-resistant phenotypes and occurrence of second malignancies associated with chemotherapy remain serious problems (Kim and Helman, 2009). Moreover, toxic effects of chemotherapy still remain a major drawback in treatment of osteosarcoma patients. Thus, there is a pressing need for the development of new and alternative approaches to the treatment of osteosarcoma (Hattinger et al., 2010).
Combination chemotherapy has received more attention in order to find compounds that could increase the therapeutic index of clinical anticancer drugs (Gutierrez et al., 2009). In this regard, dietary supplements, phytotherapeutic agents, and naturally occurring molecules (such as silibinin, resveratrol, plumbagin, benzyl isothiocyanate, 2-methoxyestradiol, DDTD) with antitumor activity and with the least toxicity to normal tissues are suggested as possible candidates to be investigated for their synergistic efficacy in combination with antineoplastic drugs (Raina and Agarwal, 2007; Chen et al., 2008; Maran et al., 2008; Kim et al., 2010; Szekeres et al., 2011; Tian et al., 2012).
Inorganic phosphate (Pi) is an essential nutrient to living organisms. It plays a key role in diverse physiological functions, including osteoblast differentiation and skeletal mineralization (Yoshiko et al., 2007). Serum Pi level is maintained within a narrow range through a complex interplay between intestinal absorption, exchange with intracellular and bone storage pools, and renal tubular reabsorption and depends mainly on the activity of Na/Pi cotransporters (Takeda et al., 2004). Pi is abundant in the diet, and intestinal absorption of Pi is efficient and minimally regulated. The kidney is a major regulator of Pi homeostasis and can increase or decrease its Pi reabsorptive capacity to accommodate Pi need. Adequate control of Pi homeostasis is crucial, as a moderate increase in serum Pi concentration and polymorphisms in genes involved in Pi metabolism may result in bone impairment and influence the aging process and lifespan (Prié et al., 2005). Relevantly, Pi is emerging as an important signaling molecule capable of modulating multiple cellular functions by altering signal transduction pathways, gene expression, and protein abundance in many cell types (Khoshniat et al., 2011).
Recently, we have provided evidence that Pi inhibits proliferation and aggressiveness of human osteosarcoma U2OS cells identifying adenylate cyclase, beta3 integrin, Rap1, ERK1/2 as proteins whose expression and function are relevantly affected in response to Pi (Naviglio et al., 2006, 2011).
Tumor suppressor pathways governed by p53 and Rb genes are known to be involved in the pathogenesis of osteosarcoma (Giordano et al., 2007; Ottaviani and Jaffe, 2009). Particularly, mutations or inactivation of p53 are found in almost 50% of OS patients and are thought to be associated with poor prognosis and drug resistance (Ognjanovic et al., 2012).
Strategies aimed to restoration and up-regulation of p53 function are being actively investigated and considered a promising way to treat human tumors including osteosarcoma (Ganjavi et al., 2006; Ternovoi et al., 2006; Graat et al., 2007; Oshima et al., 2007; Yuan et al., 2007; Hedström et al., 2008). Moreover, available evidence suggests that the molecular profile may affect biological response of tumor cells, thereby suggesting to design combined therapies based on the disease molecular background (Le Tourneau et al., 2010).
In this study, we asked whether Pi could affect chemosensitivity of osteosarcoma cells and investigated the possible involvement of p53 and the underlying mechanisms. Our data indicate that Pi is capable of inducing sensitization to doxorubicin in a p53-dependent manner and through a mechanism involving Erk1/2 down-regulation in U2OS osteosarcoma cells, implying that targeting Pi levels and its signaling might represent a novel simple way for therapeutic intervention in osteosarcoma.
Materials and Methods
Materials
All cell culture materials were from Gibco–Life Technologies (Gaithersburg, MD). Doxorubicin and p53 inhibitor pifithrine-α was purchased from Sigma (Sigma–Aldrich, St. Louis, MO). Anti-tubulin antibodies were obtained from Oncogene-Calbiochem (La Jolla, CA). Anti-procaspase-3 and anti-poly (ADP ribose) polymerase (PARP) antibodies were obtained from Upstate (Lake Placid, NY). Anti-p-ERK and anti-Bad antibodies were obtained from Cell Signaling Technology (Danvers, MA). All other antibodies were obtained from Santa Cruz Biotechnology (San Diego, CA).
Cell culture and treatments
Human osteosarcoma U2OS, Saos-2, and MG-63 cell lines were obtained from the American Type Culture Collection (Rockville, MD). U2OS, Saos-2, and MG-63 cells were grown in Dulbecco's Modified Eagle's Medium (DMEM) supplemented with 2 mM glutamine, 100 U/ml penicillin, 100 µg/ml streptomycin, and 10% fetal bovine serum (FBS) and cultured at 37°C in a 5% CO2 humidified atmosphere. Unless noted, all experiments were done in the above medium which contains 1 mM of Pi, and concentrations listed in the figures are final Pi medium concentrations. Added Pi was in the form of NaPO4, pH 7.4, from Sigma (Naviglio et al., 2006; Camalier et al., 2010). Doxorubicin was dissolved in ddH2O, stored at 4°C and diluted with culture medium to final concentrations indicated in the figures (Zou et al., 2010). Typically, subconfluent cells were split (5 × 105/10 cm plate) and grown in 10% serum containing medium. After 24 h, the medium was removed, the cells were washed with PBS and incubated with 10% FBS fresh medium (time 0), supplemented or not with Pi and doxorubicin, alone or in combination, and grown for the times and at concentrations indicated in the figures.
Floating cells were recovered from culture medium by centrifugation, and adherent cells were harvested by trypsinization. Both floating and adherent cells were used in experiments aimed to study expression of proteins involved in apoptosis and to perform FACs analysis.
Cell proliferation assay
Viable cells were determined by the 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) assay, as previously described (Naviglio et al., 2010). Briefly, cells were seeded in 96-multiwell plates at the density of 5 × 103 cells/well. Cells were treated with Pi and doxorubicin alone or in combination for up to 72 h (see the figure legends). Before harvesting, 100 µl of MTT solution (5 mg/ml) was added to each well and incubated at 37°C for 3 h, then the formazan product was solubilized by the addition of 100 µl 0.04 N HCl isopropanol. The optical density of each sample was determined by measuring the absorbance at 570 nm versus 650 nm using an enzyme-linked immunosorbent assay reader (Molecular Device Inc, Silicon Valley, CA). Cell proliferation assays were performed at least three times (in replicates of six wells for each data point in each experiment). Data are presented as means ± standard deviation (SD) for a representative experiment.
Evaluation of apoptosis by flow cytometry
After drug treatment, cells were recovered as described in the above “cell culture and treatments” paragraph, fixed by resuspension in 70% ice-cold methanol/PBS and incubated overnight at 4°C. After fixing, samples were pelleted at 400g for 5 min, and pellets were washed once with ice-cold PBS and centrifuged for a further 5 min. Pellets were resuspended in 0.5 ml DNA staining solution (50 µg/ml of propidium iodide, PI, and 100 µg RNase A in PBS), and incubated at 37°C for 1 h in the dark. Samples were transferred to 5-ml Falcon tubes and stored on ice until assayed. Flow cytometric analysis was performed using a FACSCalibur flow cytometer (Becton Dickinson, San Jose, CA) interfaced with a Hewlett-Packard computer (mod. 310) for data analysis. For the evaluation of intracellular DNA content, at least 20,000 events for each point were analyzed, and regions were set up to acquire quantitative data of cells with fragmented DNA (sub-G1 or apoptotic events) compared with the events that fell into the normal G1, S, G2 regions (Naviglio et al., 1998, 2009).
Small interfering RNA transfection
The U2OS cells were plated onto six-well plates at a density of 3 × 105 cells/well with growth medium without antibiotics. After overnight incubation, transfection was performed at a confluency of 50% by using Opti-MEM media (Gibco-Life Technologies), Lipofectamine 2000 (Gibco-Life Technologies), and specific siRNA for p53 (Cell Signaling Technology) or non-specific siRNA (Santa Cruz Biotechnology), according to the manufacturer's recommendations. Six hours later, the medium was replaced with growth medium without antibiotics. After transfection for 24 h, the cells were trypsinized, counted, and used, in part, to check p53 protein levels by immunoblotting analysis, or sub-seeded onto 96-well plates and subjected to MTT assay.
Preparation of cell lysates
Cell extracts were prepared as follows. Briefly, 3–5 volumes of RIPA buffer (PBS, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS) containing 10 µg/ml aprotinin, leupeptin, and 1 mM phenylmethylsulfonyl fluoride (PMSF) were added to recovered cells. After incubation on ice for 1 h, samples were centrifuged at 18,000g in an Eppendorf microcentrifuge for 15 min at 4°C and the supernatant (SDS total extract) was recovered. Some aliquots were taken for protein quantification according to Bradford method (Bradford, 1976); others were diluted in 4× Laemmli buffer, boiled and stored as samples for immunoblotting analysis.
Immunodetection of proteins
Typically, we employed 20–40 µg of total extracts for immunoblotting. Proteins from cell preparations were separated by SDS–PAGE and transferred onto nitrocellulose sheets (Schleicher & Schuell, Dassel, Germany) by a Mini Trans-Blot apparatus BioRad (Hercules, CA). II goat anti-rabbit or anti-mouse antibodies, conjugated with horseradish peroxidase (BioRad), were used as a detection system (ECL) according to the manufacturer's instructions Amersham Biosciences (Buckinghamshire, UK).
Statistical analysis
Most of experiments were performed at least three times with replicate samples, except where otherwise indicated. Data are plotted as mean ± SD. The means were compared using analysis of variance (ANOVA) plus Bonferroni's t-test. P-values of <0.05 were considered significant. National Institutes of Health Image J 1.42Q (NIH, Bethesda, MD) software were used for densitometric analysis.
Results
Pi inhibits proliferation of p53-wild type human osteosarcoma U2OS cells through a slowing-down of cell division cycle and not apoptosis occurrence
We have previously shown that inorganic phosphate (Pi) inhibits dose-dependently proliferation of human osteosarcoma U2OS cells via an adenylate cyclase/cAMP-mediated mechanism (Naviglio et al., 2006). Throughout our studies, we have used a spectrum of final concentration of Pi to cover the physiologic range in humans and in agreement with most of the published studies on Pi-triggered effects (Naviglio et al., 2006, 2011; Camalier et al., 2010; Khoshniat et al., 2011).
To evaluate the possible role of p53 in Pi-induced growth suppressive effect in U2OS cells, first we looked at the impact of inorganic phosphate on proliferation of osteosarcoma cells with different status of endogenous p53. To this purpose, p53-wild type U2OS, p53-null Saos, and p53-mutant MG63 human osteosarcoma cell lines (Huang et al., 2007; Li et al., 2011) were exposed to 5 mM Pi (sub-maximal dose) for up to 72 h, after which cell proliferation was determined by conventional MTT assay and by direct cell number counting. Figure 1A, shows that in U2OS cells (containing functional p53 protein) Pi causes a statistically significant reduction of cell viability (P < 0.001) of 12%, of 20%, of 30% at 24, 48, 72 h, respectively; in contrast, such growth inhibitory effect was not observed in Saos and MG63 cells (lacking of p53 function). Particularly, in Saos-2 cells, indeed, Pi treatment does result in an increase of cell proliferation. Parallel direct cell counting and growth curves provided similar results (data not shown).
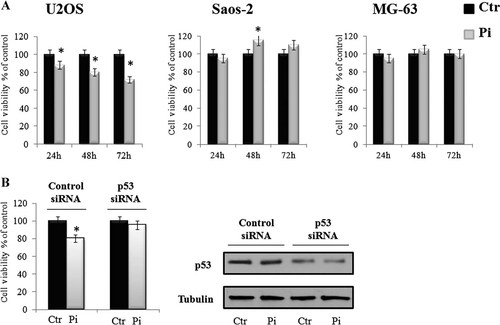
Effects of Pi on the cell viability of various osteosarcoma cell lines. Part A: U2OS, Saos-2, and MG-63 cells were cultured in medium supplemented with 5 mM Pi or not (control) for 24, 48, 72 h. Then, cell viability was measured by MTT assay. Data represent the average of three independent experiments. The means and SD are shown. *P < 0.05 versus control untreated cells. Part B: U2OS cells were transfected with p53 specific or non-specific siRNA and then cultured in medium supplemented with 5 mM Pi or not (control) for 48 h. p53 protein level was examined by Western blotting. Cell viability was measured by MTT assay. Data represent the average of two independent experiments. The means and SD are shown. *P < 0.05 versus control untreated cells.
To extend data on relationship between p53 expression and cell viability in response to Pi, we next used p53-specific siRNA transfection to suppress p53 expression in the U2OS cells. p53 siRNA effectively inhibited p53 protein expression in the U2OS cells This p53 silencing significantly prevented the antiproliferative effect induced by Pi (Fig. 1B).
Thereafter, distribution of cells in cell cycle phases was evaluated by flow cytometric analysis of propidium iodide-stained cells. We also looked at the proportion of cells with hypoploid DNA content (sub-G1 population), characteristic of cells having undergone to DNA fragmentation which is a biochemical hallmark of apoptosis. Figure 2 shows that at each time point considered (from 24 up to 72 h) in Pi-treated U2OS cells the percentage of G1 phase cells is higher than that of control untreated cells, with a concomitant decrease of S phase. Moreover, no obvious appearance of sub-G1 population in response to Pi was observed up to 72 h. As far as Saos and MG63 cells concerned, no relevant changes of cell cycle phases upon Pi treatment occurred (data not shown).

Effects of Pi on the distribution of U2OS cells in sub-G1 and cell cycle phases. Cells were cultured in medium supplemented with 5 mM Pi or not (control) for 24, 48, and 72 h. Then, FACS analysis of propidium iodide-stained cells was performed. Quantitative data indicating the percentage of hypoploid sub-G1, G1, S, and G2/M cells from three independent experiments are shown. The means and SD are shown.
Overall the above data suggest that anti-proliferative effect caused by inorganic phosphate in U2OS cells (and not in p53-deficient Saos and MG63 cells) is mainly due to a slowing-down of cell division cycle and not to apoptosis occurrence and that p53 could be involved in.
Pi enhances doxorubicin-induced cytotoxicity in U2OS, but not in p53-deficient Saos and MG-63 cells
Doxorubicin is a DNA-damaging agent that generates DNA double-strand breaks (DNA DSBs) by inhibiting Topoisomerase II (Gewirtz, 1999). Doxorubicin is used as a clinically relevant antitumor drug widely included in most of chemotherapic treatment protocols for treating human osteosarcoma (Dai et al., 2011).
We then investigated whether Pi could enhance doxorubicin-induced cytotoxicity in osteosarcoma cells. To this purpose, we treated osteosarcoma U2OS cells with varying concentrations of doxorubicin, in the presence or absence of 5 mM Pi. Specific treatment conditions were examined encompassing exposure to no (0 mM, control), very low (0.1 µM), low (1 µM), or high (5 µM) doxorubicin, in the presence or absence of 5 mM Pi for 24 h.
After treatments a conventional tetrazolium-based (MTT) assay was performed (Fig. 3, part A).
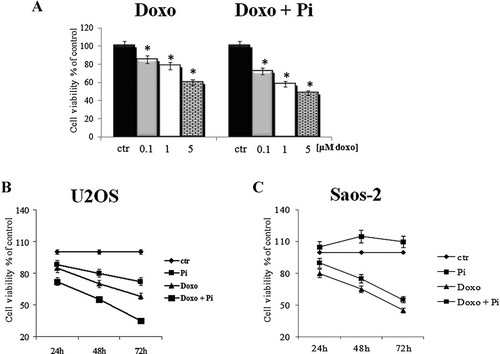
Effects of Pi on doxorubicin-induced cytotoxicity. Part A: Dose–response experiments U2OS cells were treated or not with increasing concentrations of doxorubicin alone or in combination with 5 mM Pi for 24 h. Then, the cell viabilitiy was measured by MTT assay. Data represent the average of three independent experiments. The means and SD are shown. *P < 0.05 versus control untreated cells. Parts B and C: Time-course experiments. U2OS (part B) and Saos-2 (part C) cells were treated or not with 0.1 µM doxorubicin alone or in combination with 5 mM Pi for 24, 48, and 72 h. Then, the cell viabilitiy was measured by MTT assay. Data represent the average of three independent experiments. The means and SD are shown.
As expected, proliferation of U2OS cells was slightly inhibited by doxorubicin in a dose-dependent manner (Bednarski et al., 2009; Tentner et al., 2012). Interestingly, we found that in all combinations the presence of Pi strongly enhanced the anti-proliferative effects of doxorubicin (to note, at very low dose 0.1 µM doxorubicin the inhibition increases from 15% to 35% in presence of Pi).
Moreover, we also looked at Pi/doxorubicin combination-induced cytotoxicity during a time course.
U2OS cells were exposed to no (0 mM, control) or very low (0.1 µM) doxorubicin in the presence or absence of 5 mM Pi for 24, 48, and 72 h. Thereafter, MTT assay was performed (Fig. 3, part B). As expected, proliferation of U2OS cells was greatly decreased by doxorubicin in a time-dependent manner. Remarkably, the growth inhibitory effects induced by Pi/doxorubicin combination are significantly higher than those caused by doxorubicin alone (at 48 h the inhibition increases from 30% to 45%; at 72 h from 42% to 75%).
Similarly, we performed time course and dose effects cotreatments with Pi and doxorubicin in p53-null Saos and p53-mutant MG63 human osteosarcoma cells. Figure 3, part C shows that doxorubicin-induced cytotoxicity in Saos cells was not enhanced by Pi. Similar results were obtained in MG63 cells (data not shown).
Overall, the above data suggest that Pi enhances doxorubicin-induced cytotoxicity in osteosarcoma U2OS cells (and not in p53-deficient Saos and MG63 cells) and that p53 may contribute to this phenomenon.
Pi potentiates the doxorubicin-induced cytotoxicity in U2OS cells by inducing apoptosis
To better understand the enhancement by Pi of doxorubicin-induced cytotoxicity, U2OS cells were exposed to no (0 mM, control), very low (0.1 µM) doxorubicin in the presence or absence of 5 mM Pi for 24 and 48 h.
Then, cells were fixed and used for flow cytometry-based assays of cell-cycle progression and cell death.
In agreement with previous results (Varmeh and Manfredi, 2008), Figure 4, part A shows that doxo-treated U2OS cells strongly accumulated in G2 phase with a concomitant decrease of G1 and S phases of cell cycle; G2 accumulation was already evident at 24 h (more than 70% cells in G2) and increased at 48 h (more than 90% cells in G2). Moreover, a sub-G1 population (20%) in response to doxo was observed at 48 h. Interestingly, Figure 4 shows that doxo/Pi combination induced a time-dependent increase of sub G1 population (from 9% at 24 h, up to 41% at 48 h), whereas the treatment with Pi alone did not cause any relevant change in the sub-G1 fraction (Fig. 4, part B; Fig. 2). Accumulation of cells with a hypodiploid DNA content is consistent with cell death by apoptosis. This was further confirmed by examining activation of the terminal caspase 3, executioner of apoptosis and cleavage of poly(ADP-ribose)polymerase, PARP, a known target for apoptosis-associated caspase cleavage (Yuan et al., 2007; Naviglio et al., 2009).
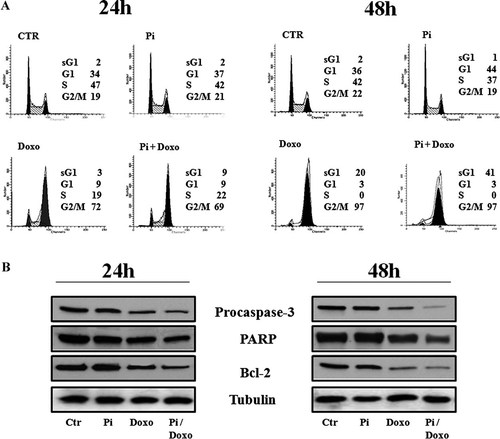
Effects of Pi, doxorubicin, and Pi/doxorubicin combination on apoptosis of U2OS cells. Treatments with Pi 5 mM, doxorubicin 0.1 µM, Pi 5 mM/doxorubicin 0.1 µM were carried out for 24 and 48 h. Part A: Representative FACS histograms of propidium iodide stained cells (20,000 events/sample) are shown. The percentage of hypoploid sub-G1 and of each cell-cycle phases is indicated. In Part B the effects on pro-caspase-3, PARP, and Bcl-2 protein levels are shown. Thirty microgram of cell extracts from cells were subjected to SDS–PAGE and blotted with antibodies against the indicated proteins (α-tubulin was used as a standard for the equal loading of protein in the lanes). The image is representative of three immunoblotting analysis from three different cellular preparations with similar results.
Figure 4, part B shows a strong decrease of the uncleaved isoform of caspase-3 in 24 h doxo/Pi-treated cells suggesting the increase of its activity that is correlated to its fragmentation. Doxo alone induced similar effects on caspase 3 activation but at later time point, 48 h.
Notably, no decrease of procaspase-3 protein level was observed in U2OS cells treated with Pi alone for up to 48 h. Finally, we have evaluated the effects of the different treatments on the fragmentation of PARP that is a substrate for caspase-3. The pattern of the PARP processing paralleled that of caspase-3 cleavage (Fig. 4, part B).
In addition, Bcl2 anti-apoptotic protein was consistently down-regulated in doxo/Pi-treated U2OS cells and a less pronounced decrease was recorded in cells treated with doxo alone.
Overall the above data suggest that Pi potentiates the doxo-induced antiproliferative effects by inducing apoptosis of G2-arrested U2OS cells.
The enhancement by Pi of doxorubicin-induced cytotoxicity in U2OS cells is mediated by p53
The regulation of p53 involves a complex network of proteins, with MDM2 being a primary regulator of p53 protein levels and activity (Moll and Petrenko, 2003).
The p53 tumor suppressor is phosphorylated in response to various cellular stress signals, such as DNA damage, leading to its release from MDM2 and consequent stabilization and activation as a transcription factor. It is known that in U2OS cells, treatment with the DNA-damaging agent doxorubicin causes p53 to be phosphorylated on serine residues (mainly at Ser-15), leading to the dissociation of p53 from MDM2 and transcription of target genes (Jackson et al., 2004; Yuan et al., 2007).
To explore the possible role of p53 in the enhancement of doxo-induced cytotoxicity in p53-wild type U2OS cells, Western blotting was applied to examine the expression of p53 and well-known transcriptional target genes of p53, such as Bax, MDM2, and p21 (Fig. 5, part A, left part).
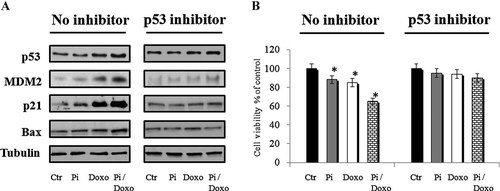
Effects of p53 inhibitor pifithrine-α on the cell viability of U2OS and on p53, MDM2, p21, Bax protein levels in response to Pi, doxorubicin, and Pi/doxorubicin combination. Part A: U2OS cells were treated or not with 0.1 µM doxorubicin alone or in combination with 5 mM Pi for 24 h, in absence or presence of 20 µM p53 inhibitor pifithrine-α (PFT-α). Thirty microgram of cell extracts were subjected to SDS–PAGE and blotted with antibodies against the indicated proteins. The image is representative of three immunoblotting analysis from three different cellular preparations with similar results. Part B: U2OS cells were treated or not with 0.1 µM doxorubicin alone or in combination with 5 mM Pi for 24 h, in absence or presence of 20 µM p53 inhibitor pifithrine-α (PFT-α). Then, the cell viabilitiy was measured by MTT assay. Data represent the average of three independent experiments. The means and SD are shown. *P < 0.05 versus control untreated cells.
The p53 protein level was not greatly affected by Pi, but was enhanced by doxorubicin and further augmented by the Pi/doxorubicin combination. The expression of pro-apoptotic Bax and p21 was further increased by the Pi/doxorubicin combination than doxo alone. The MDM2 expression level was also enhanced. Adversely, the expression of anti-apoptotic Bcl-2 was decreased by the Pi/doxorubicin combination compared with doxorubicin alone (Fig. 4, part B).
To further prove the role of p53 in the sensitization to doxorubicin by Pi, we next examined the cell viability and the expression of p53 and Bax, MDM2, and p21 transcriptional p53 target genes in response to doxorubicin, Pi, and doxorubicin/Pi combination in presence of the p53 inhibitor pifithrine-α (Alkhalaf and Jaffal, 2006; Li et al., 2011). Very interestingly, Figure 5, part B shows that the p53 inhibition by pifithrine-α significantly reduced the doxorubicin/Pi combination-induced cytotoxicity. Accordingly, Bax, MDM2, and p21 protein levels increase in response to Pi/doxorubicin combination was also prevented by p53 pifithrine-α inhibitor (Fig. 5, part A, right part).
Altogether, the above results strongly suggest that the enhancement by Pi of doxorubicin-induced cytotoxicity in osteosarcoma U2OS cells is p53 dependent.
Pi impairs Erk1/2 activation in response to doxorubicin in U2OS cells
The signaling events implicated in survival, growth arrest, or programmed cell death in response to DNA damaging stress include the activation of mitogen-activated protein kinase pathways (Huang et al., 2007).
In several types of cancers, including osteosarcoma, ERK1/2 are up-regulated in response to DNA-damaging chemotherapeutic agents, such as cisplatin or doxorubicin (Tentner et al., 2012). Activation of the ERK pathway by DNA-damaging agents has been described to correlate with increased apoptosis or lead to an antiapoptotic effect (Discussion section).
In order to investigate the possible role of ERK1/2 in the potentiation by Pi of doxo-induced cytotoxicity in U2OS cells, Western blotting was applied to examine the expression and phosphorylation (activation) of ERK1/2 from extracts of cells treated with Pi, doxorubicin and Pi/doxorubicn combination during a time course for up to 24 h (Fig. 6).
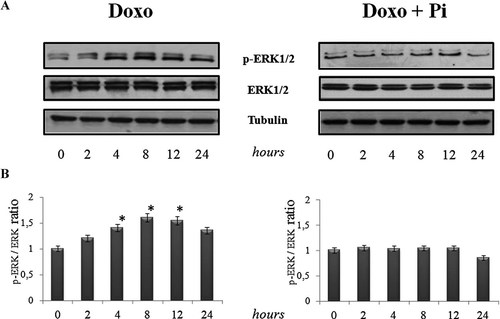
Effects of Pi, doxorubicin, and Pi/doxorubicin combination on ERK1/2 activation. U2OS cells were treated or not with 0.1 µM doxorubicin alone or in combination with 5 mM Pi during a time course for up 24 h. Part A: The activation (phosphorylation) and levels of ERK1/2 proteins were assessed by Western blotting from 30 µg of cell extracts using antibodies against the indicated proteins. The image is representative of three different experiments with similar results. Part B: Graphs showing the densitometric intensity of P-ERK1,2/ERK1,2 bands ratio are shown. The intensities of signals were expressed as arbitrary units. *P < 0.05 versus control untreated cells.
To note, previously we have provided evindence that Pi 5 mM treatment in U2OS cells resulted in a rapid and transient increase of ERK1/2 phosphorylation evident at 15 min that declined to basal level at 30 min and followed by a prolonged inhibition up to 24 h (Naviglio et al., 2011).
Figure 6 shows that doxorubicin induced a time-dependent increase in ERK activity starting at 4 h of doxorubicin incubation and declining after 12–24 h. Interestingly, the doxo-induced ERK1/2 activation was impaired in response to Pi. None of the treatments significantly affected the total amount of proteins examined.
Overall, the above findings indicate that Pi treatment of U2OS cells interferes with the modulation of ERK1/2 activation in response to doxorubicin and suggest that the Pi-mediated inhibition of ERK signaling might be involved in the enhancement by Pi of doxo-induced cytotoxicity in U2OS cells.
Discussion
Due to its high metastatic potential and the frequent acquisition of chemotherapeutic resistance, the clinical outcome for osteosarcoma remains discouraging despite aggressive treatments. Therefore, new treatment modalities for osteosarcoma are urgently needed (Gutierrez et al., 2009; Kim and Helman, 2009; Hattinger et al., 2010).
The primary role of Pi in osteoblast differentiation and skeletal mineralization is largely known.
Intriguingly, Pi is emerging also as an important signaling molecule capable of modulating multiple cellular functions by altering signal transduction pathways, gene expression and protein abundance in many cell types (Khoshniat et al., 2011).
Recently, we have provided evidence that Pi inhibits proliferation and aggressiveness of human osteosarcoma U2OS cells identifying adenylate cyclase, beta3 integrin, Rap1, ERK1/2 as proteins whose expression and function are relevantly affected in response to Pi (Naviglio et al., 2006, 2011).
Importantly, in agreement with our previous findings, it has been reported that L/B/K ALP, alkalin phosphatase, whose main action is to locally increase the Pi levels in extracellular environment, inhibits the aggressiveness and the metastatic ability of U2OS cells, by modulating the expression of genes involved in cell proliferation and adhesion (Zucchini et al., 2004).
In the current study, we describe that in wild p53 containing osteosarcoma U2OS cells, and not in p53 null Saos and p53 mutant MG63 osteosarcoma cells, Pi is capable of inducing sensitization to doxorubicin. We provide evidence that the enhancement of doxorubicin-induced cytotoxicity by Pi occurs via a p53-dependent apoptosis and through a mechanism involving ERK1/2 down-regulation.
It is well known that doxorubicin is able to induce DNA damage and leads to cell cycle arrest or apoptosis by activating p53 (Yuan et al., 2007; Varmeh and Manfredi, 2008; Tentner et al., 2012).
Here, we show that the enhanced apoptosis in response to Pi/doxorubicin combination in the U2OS cells is associated with an accumulation of the p53 protein. The Mdm2-p53 feedback loop is the main mechanism in the regulation of the p53 level. Mdm2, a transcriptional target of p53, inhibits p53 by directly binding to it to antagonize its activity and enhance its degradation (Moll and Petrenko, 2003).
Adversely, when the nuclear p53 level is elevated, it activates the transcription of the Mdm2 gene. After treatment with the Pi/doxorubicin combination, Mdm2 expression was consistent with p53 upregulation. This is possibly because p53 upregulation induced Mdm2 expression according to this negative feedback loop.
Moreover, the wild-type p53 gene is a negative regulator of cell growth by the transcriptional activation of p21 which plays a crucial role in controlling DNA repair, cell differentiation, and apoptosis in response to p53 activation (el-Deiry et al., 1994). Accordingly, the expression of p21 was also further increased by the Pi/doxorubicin combination. Bax and Bcl-2, members of the Bcl-2 family, exert proapoptotic or anti-apoptotic functions, respectively, to regulate p53-dependent apoptosis (Cory and Adams, 2002). The Bcl-2 protein is able to inhibit a number of apoptotic death pathways. The 21 kDa protein partner Bax, which overexpresses to counter the death repressor activity of Bcl-2, can enhance apoptosis. The ratio of Bcl-2/Bax determines survival or death following an apoptotic stimulus (Thornborrow et al., 2002). Interestingly, the Pi/doxorubicin combination-induced p53 upregulation is followed also by a subsequent increase of Bax and decrease of Bcl-2 protein levels to culminate in apoptotic cell death.
Caspase-3 is a key executor of the apoptotic machinery. Once activated by apoptotic signals, caspase-3 is proteolytically cleaved to active its substrates, such as PARP, resulting in the activation of the DNA fragmentation of apoptosis (Mazumder et al., 2008). Consistent to the above data, we also found that Pi promoted caspase-3 activation and PARP cleavage in doxorubicin-treated U2OS cells. In addition, we also describe that p53 inhibitor pifithrine-α. significantly reduced the doxorubicin/Pi combination-induced cytotoxicity, strongly enforcing the evidence that p53 function is required for the Pi/doxorubicin combination-induced cytotoxicity.
In several types of cancers, including osteosarcoma, ERK1/2 are up-regulated in response to DNA-damaging chemotherapeutic agents, such as doxorubicin or cisplatin.
ERK1/2's role in promoting survival and progression into the cell cycle in the absence of DNA damage is well established (Ballif and Blenis, 2001; Chambard et al., 2007). Furthermore, several studies have implicated ERK activity in these same pro-survival and cell cycle progression responses in cells under DNA damaging conditions (Hayakawa et al., 1999; Kumar et al., 2007; Tsakiridis et al., 2008; Nishioka et al., 2009). In contrast, a small but growing number of studies have indicated roles for Erk in promotion of cell death under a variety of conditions including following DNA damage (Zhuang and Schnellmann, 2006; Cagnol and Chambard, 2010). Our data describing that Pi inhibits the ERK1/2 activation in response to low doses of doxorubicin in U2OS cells are consistent with a pro-survival, anti-apoptotic effect of doxorubicin-induced ERK1/2 activation. Our findings are also in agreement with those indicating that the protective roles of GSTP1 against apoptosis triggered by doxorubicin and cisplatin in osteosarcoma cells is mediated by the activation of ERK1/2 (Huang et al., 2007).
Our data indicate that Pi can dramatically enhance doxorubicin-induced cell death through modulation of p53 and ERK1/2 signaling pathways within the tumor cells themselves. The detailed molecular mechanism underlying this enhancement of doxorubicin-induced cytotoxicity by Pi remains unclear and interplay between these pathways (and others?) is very likely implicated in the observed enhancement of apoptosis in U2OS osteosarcoma cells (Alkhalaf and Jaffal, 2006; Tentner et al., 2012). However, we do know that further studies and more exhaustive experiments are warranted.
Importantly, so far we are accumulating evidence that ERK1/2 inhibition in response to Pi is accompanied by a consistent down-regulation of protein levels of upstream B-Raf and Raf-1 kinases (data not shown) and these events are actually under our investigation to further explore and explain how Pi affects ERK1/2 function to inhibit cell viability and to enhance doxorubicin-induced cytotoxicity.
By the way, whatever the exact mechanism(s) here we report that Pi may act as a potent enhancer of doxorubicin-induced cytotoxicity in osteosarcoma cells via p53 activation.
Combination chemotherapy has received more attention in order to find compounds that could increase the therapeutic index of clinical anticancer drugs.
Importantly, in our study, Pi was found to have a positive pharmacological interaction even with a very low dose (0.1 µM) doxorubicin that is expected to be more torelable and associated to minimal undesired side-effects in patients, thus increasing the potential clinical relevance of our data.
New drug delivery systems have been developed that incorporate anticancer drugs into calcium phosphate cement (CPC) to maintain high concentrations of anticancer drugs at bone local sites (Lopez-Heredia et al., 2011; Tanzawa et al., 2011). Very interestingly, inorganic phosphate release and its bone retention from CPC is predict to occur, thus affecting Pi concentrations locally.
Collectively, our data enforce the evidences of Pi as a signaling molecule in osteosarcoma cells, indicate that Pi may act as a potent enhancer of doxorubicin-induced cytotoxicity in U2OS cells via p53 activation and Erk1/2 inhibition, suggesting that targeting Pi levels might represent potentially a novel way for therapeutic intervention in osteosarcoma.