Vertebral Fracture Assessment Increases Use of Pharmacologic Therapy for Fracture Prevention in Clinical Practice
ABSTRACT
The impact of vertebral fracture assessment (VFA) on lateral spine images in clinical practice on subsequent patient use of fracture prevention medication is unknown. Our objective was to determine the association of prevalent vertebral fracture identified on bone density lateral spine images (positive VFA) with subsequent use of fracture prevention therapy in usual clinical practice, using the Manitoba Bone Density Program database prospective observational cohort. Since 2010, targeted VFA imaging has been done at the time of bone densitometry in Manitoba for 21% of women and men meeting criteria based on age, bone mineral density (BMD), height loss, and glucocorticoid use. Among 6652 treatment-naive individuals with at least 90 days follow-up who had VFA imaging, 923 (13.9%) had one or more definite vertebral fractures identified using a modified algorithm-based qualitative (ABQ) method. For those with a positive VFA, their bone density reports stated the patient was at high risk of subsequent fracture and qualified for fracture prevention therapy. Subsequent osteoporosis treatment initiated within the next 12 months was identified using population-based pharmacy data. Logistic regression models were used to estimate the association of positive VFA with subsequent prescription (Rx), compared to negative VFA. Fracture prevention medication was started by 2127 (32%) individuals, 52.3% with positive versus 28.4% with negative VFA (p value <0.001). This association was substantially stronger in those designated (before VFA results were known) to have low or moderate fracture risk compared to high fracture risk (interaction p value <0.001), and in those with osteopenia (OR 4.51; 95% CI, 3.48 to 5.85) compared to those with osteoporosis by BMD criteria (OR 1.72; 95% CI, 1.43 to 2.08, interaction p value <0.001). Targeted VFA imaging at the time of bone densitometry substantially improves identification of those at high fracture risk and fracture prevention medication use among those with prevalent vertebral fracture. © 2019 American Society for Bone and Mineral Research. © 2019 American Society for Bone and Mineral Research.
Introduction
Over the past several years, the proportion of older individuals with osteoporosis and/or high risk of fracture who are being treated to reduce their fracture risk has been decreasing.1 Reversing this treatment gap requires that patients and their healthcare providers be aware that prior fractures, including vertebral fractures, are a marker of bone fragility warranting fracture prevention therapy.2 Prevalent vertebral fractures increase with age among postmenopausal women and older men, indicate a higher risk for subsequent fractures independent of bone mineral density (BMD),3-6 and if unexplained by prior major trauma are an indication for pharmacologic fracture prevention therapy.7-9 However, two-thirds to four-fifths of vertebral fractures are not recognized clinically at the time of their occurrence,10-12 and require lateral spine imaging for their identification.
Densitometric thoracolumbar lateral spine images for vertebral fracture assessment (VFA) can be obtained at the time of bone densitometry with dual-energy X-ray absorptiometry (DXA) at very low cost and much less radiation exposure than standard radiography, and moderate to severe radiographic vertebral fractures can be identified on these images with high accuracy.13, 14 Prevalent vertebral fracture identified specifically on bone density VFA images predict, after adjustment for both age and BMD, incident clinical fractures (regardless of skeletal site);15, 16 osteoporotic fractures;15, 16 hip fractures;16, 17vertebral fractures;16, 17and fracture hospitalizations.17 Importantly, these associations are equally strong in the subsets without osteoporosis by BMD criteria or low-to-moderate estimated fracture risk (before prevalent vertebral fracture status is known), who otherwise might not be considered candidates for pharmacologic fracture prevention therapies.16, 17
Two small studies have shown that documentation of prevalent vertebral fractures on VFA images changes physician management of patients with low bone mass,18, 19 and increases prescription of pharmacologic fracture prevention therapies.19 However, no study to date has examined whether or not documentation of prevalent vertebral fracture alters patient medication use behavior, either in research setting or usual clinical practice.
Our primary objective was to estimate the association of prevalent vertebral fracture identified on lateral spine VFA images obtained at the time of bone densitometry with subsequent fracture prevention medication use, using pharmacy claims data. Our secondary objective was to estimate if this association varied by BMD category or fracture risk estimated by Fracture Risk Assessment Tool (FRAX).
Subjects and Methods
In the Province of Manitoba, health services are provided to virtually all residents through a single public healthcare system, and DXA services have been managed as an integrated program since 1997.20 The program maintains a database of all DXA results with completeness and accuracy in excess of 99%, that can be linked with other provincial population-based computerized health databases through an anonymous personal identifier.21 The study was approved by the Health Research Ethics Board for the University of Manitoba.
Study population
From the DXA database we identified 47,944 women and men age 50 years and older who were registered with Manitoba Health and underwent bone densitometry of the hip and lumbar spine between February 24, 2010 (when VFA testing was introduced) and March 30, 2016. Among these, 10,053 (21%) had VFA imaging performed at the time of the DXA test (Fig. 1). Before VFA imaging was started in Manitoba, all DXA technologists had 3 days of rigorous training on how to acquire high-quality lateral spine VFA images. Indications for VFA were a T-score of ≤ −1.5 (at the lumbar spine, total hip, or femoral neck) plus: (i) age ≥70 years or (ii) age 50 to 69 years and historical height loss (recalled young adult height minus current height) >5 cm, or measured height loss >2.5 cm, or corticosteroid exposure of ≥7.5 mg prednisone daily for at least 3 months over the past year. These criteria were chosen based in part on a cost-effectiveness modeling study showing VFA is cost-effective for postmenopausal women with T-scores of −1.5 or lower,22 and to ensure that the pretest probability of a prevalent vertebral fracture would be high enough (10% or more) to justify screening. As has been done in other studies and clinical practices,19 bone densitometry technologists evaluated whether or not the person undergoing DXA met one of the indication for VFA listed above, and proceeded accordingly. An audit of bone density tests done in a representative month (June 2015) showed that among 675 individuals meeting criteria for a VFA, the procedure was not done in only six individuals (0.9%). Moreover, among all individuals who actually had a VFA, 95.5% met the criteria listed above, and for all of the remaining 4.5% the VFA was done because the technologist suspected a possible vertebral fracture based on the anteroposterior (AP) spine image.
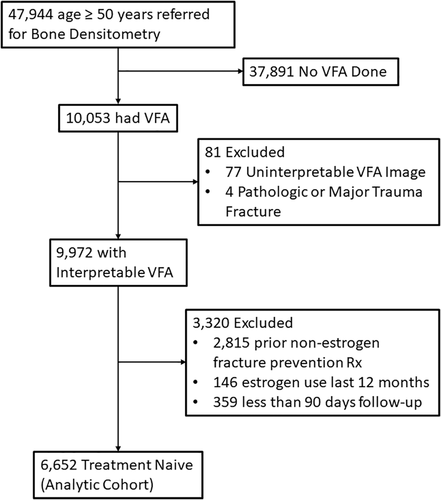
After excluding 77 individuals with poor-quality VFA images, four with a pathologic or major trauma fracture, and 150 (0.15%) who could not be matched to pharmacy claims, 9822 (93% women) were included in the analytic cohort (Fig. 1). Of these, 6652 (92% women) were treatment-naive (had not received any bisphosphonate, denosumab, raloxifene, calcitonin, teriparatide, or systemic estrogen product in the prior 12 months) and had at least 90 days of observation. Pharmacologic therapy initiation was considered to have occurred if identified in claims data within 12 months following the DXA-VFA date.
BMD measurements
Hip and lumbar spine DXA scans were performed and analyzed according to manufacturer recommendations (Lunar Prodigy or iDXA; GE Healthcare, Madison, WI, USA), as has been thoroughly described in prior publications.16, 20
VFA
VFA image interpretation was performed by the same physician (certified by the International for Clinical Densitometry [ISCD]) who also read the accompanying DXA scans for BMD measurement. Poor quality images (ie, most vertebrae uninterpretable) were excluded. For the remaining images, the reporting physician assessed for presence of vertebral fracture with the modified algorithm-based qualitative (ABQ) method, using the morphologic criteria of endplate depression or cortical discontinuity and excluding nonfracture causes of vertebral deformity (such as degenerative remodeling, Scheuermann's disease, Schmorl's nodes).23-25 Ancillary imaging on the provincial picture archiving and communications system (PACS) was reviewed when available to assist in VFA reporting. Subsequently, on a random sample of 127 images, one-half of which were reported to be VFA-positive and one-half VFA-negative, interrater agreement with two expert readers, both blinded to the clinical readings, were very high (kappa scores 0.86 and 0.78, respectively). VFA images at the individual level were recorded as: (i) one or more vertebral fractures definitely present (positive VFA); (ii) vertebral fractures definitely not present (negative VFA); or (iii) possible prevalent vertebral fracture (uncertain VFA, usually with a recommendation for additional imaging).
If one or more definite vertebral fractures was present (regardless of their severity or grade), the DXA report sent back to the primary care physician advised that the patient was at high risk of subsequent fracture, qualifying for pharmacologic fracture prevention therapy under the Osteoporosis Canada guidelines. Vertebral level, number, and severity of fractures were included in the DXA reports, but the database recorded only whether the VFA was positive, uncertain, or negative for one or more vertebral fractures.
Covariate measurement and fracture probability calculations
Ten-year probability of a major osteoporotic fracture (MOF) and hip fracture with femoral neck BMD was calculated for each subject using the Canadian FRAX tool (FRAX® Desktop Multi-Patient Entry, version 3.7), incorporating femoral neck BMD (FRAX with BMD) but without taking into consideration VFA status. The inputs used for generating the FRAX scores have been described thoroughly in a recent publication.16 The Canadian FRAX tool was calibrated using nationwide hip fracture and mortality data.26-28
Assessment of fracture prevention medication use
All retail prescriptions dispensed within the province of Manitoba are captured in the provincial pharmacy claims database. We used this database, linked to the Manitoba Bone Density database, to ascertain if one or more prescriptions for a fracture prevention medication (etidronate, alendronate, risedronate, zoledronic acid, denosumab, raloxifene, calcitonin, teriparatide or systemic estrogen product) was dispensed within 12 months following the index DXA-VFA study.
Statistical analyses
Baseline characteristics (ascertained at time of the DXA) of individuals with VFA positive for one or more vertebral fractures were compared to those with VFA negative for vertebral fractures using t tests for continuous variables and chi-square tests of independence for categorical variables. A Kaplan-Meier estimator was used to plot the proportions of individuals not being treated with fracture prevention medication as a function of follow-up time, stratified by prevalent vertebral fracture status (VFA positive, uncertain, or negative).
Logistic regression models were used to estimate the association of positive VFA and uncertain VFA with subsequent treatment compared to negative VFA, unadjusted and adjusted for: (i) FRAX with BMD 10-year risk for MOF by category (low [<10%], moderate [10% to 20%], or high [>20%]); or (ii) for BMD T-score category based on the minimum T-score of the lumbar spine, total hip, and femoral neck. Unadjusted models were also run within subsets defined by FRAX with BMD risk category and subsets defined by BMD T-score category. Secondary models were created adjusting for: (i) FRAX risk (as a continuous variable) and an interaction term between prevalent vertebral fracture status and FRAX risk; and (ii) femoral neck BMD and an interaction term prevalent vertebral fracture status and femoral neck BMD. Unadjusted analyses were also re-run separately for men versus women. ORs and 95% CI) are reported.
Finally, to assess the influence of VFA on fracture prevention medication use over time, we performed an interrupted time series analysis illustrating the year by year changes in fracture prevention medication use among all of those who met criteria for VFA, and (starting in year 2010) the subsets with a positive and negative VFA.
Results
One or more definite prevalent vertebral fractures (positive VFA) were identified in 923 (13.9%) analytic cohort members, one or more uncertain fractures (without any definite vertebral fracture) in 204 (3.1%), and no vertebral fractures (negative VFA) in 5525 (83.1%). Compared to those with a negative VFA, those with a positive VFA were older, had lower BMD at all skeletal sites, had higher estimated 10-year risks of major osteoporotic and hip fractures by FRAX, were more likely to be male, and more likely to have had a prior fracture (Table 1). Among 3369 analytic cohort members with osteopenia (minimum T-score < −1.0 and > −2.5), 327 (9.7%) had a positive VFA, and among 3711 with moderate FRAX risk (before VFA status was known), 436 (11.7%) had a positive VFA. Fracture prevention medication was subsequently dispensed for 2127 (32%) of the analytic cohort (alendronate, n = 1408 [66.2%]; risedronate, n = 491 [23.1%]; subcutaneous denosumab, n = 131 [6.2%]; intravenous zoledronic acid, n = 35 [1.6%]; teriparatide, calcitonin, etidronate, or raloxifene, n = 62 [2.9%]). Among those with a positive VFA, 52.3% were dispensed fracture prevention medication, compared to 28.4% with a negative VFA and 36.3% of those with an uncertain VFA (p value < 0.001, Fig. 2). Without VFA, 1606 (24.1%) of the analytic cohort would have met Osteoporosis Canada guideline criteria for fracture prevention therapy (FRAX 10-year major osteoporotic fracture risk of ≥20%).9 With known VFA results, an additional 568 individuals were identified as being at high fracture risk, a 35% increase in treatment candidates.
| Characteristic | Total n = 6652 | VFA-negative n = 5525 | VFA-positive n = 923 | VFA-uncertain n = 204 | pa |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 75.8 ± 6.9 | 75.6 ± 6.7 | 77.0 ± 7.8 | 76.0 ± 8.0 | <0.001 |
| Sex, n (%) | <0.001 | ||||
| Female | 6148 (92.4) | 5157 (93.3) | 811 (87.9) | 180 (88.2) | |
| Male | 504 (7.6) | 368 (6.7) | 112 (12.1) | 24 (11.8) | |
| BMI (kg/m2), mean ± SD | 26.3 ± 4.9 | 26.4 ± 5.0 | 26.2 ± 4.4 | 26 ± 4.5 | 0.175 |
| Prior fracture, n (%) | 1439 (21.6) | 1068 (19.3) | 319 (34.6) | 52 (25.5) | <0.001 |
| Parental hip fracture, n (%) | 872 (13.1) | 715 (12.9) | 131 (14.2) | 26 (12.7) | 0.297 |
| Current smoking, n (%) | 567 (8.5) | 458 (8.3) | 89 (9.6) | 20 (9.8) | 0.172 |
| Glucocorticoid use, n (%) | 356 (5.4) | 299 (5.4) | 49 (5.3) | 8 (3.9) | 0.898 |
| Rheumatoid arthritis, n (%) | 177 (2.7) | 146 (2.6) | 27 (2.9) | S | 0.623 |
| High alcohol use, n (%) | 9 (0.1) | 6 (0.1) | 0 (0) | S | 0.388 |
| Femoral neck T-score, mean ± SD | −2.0 ± 0.7 | −2.0 ± 0.7 | −2.2 ± 0.8 | −2.1 ± 0.8 | <0.001 |
| Lumbar spine T-score, mean ± SD | −2.0 ± 1.1 | −2 ± 1.1 | −2.4 ± 1.1 | −2.3 ± 1.2 | <0.001 |
| Total hip T-score, mean ± SD | −1.7 ± 0.8 | −1.6 ± 0.8 | −2.0 ± 0.9 | −1.9 ± 0.9 | <0.001 |
| Minimum T-score osteoporotic, n (%) | 3168 (47.6) | 2485 (45.0) | 583 (63.2) | 101 (49.5) | <0.001 |
| FRAX MOF percent (with BMD), mean ± SD | 16.3 ± 8.1 | 15.8 ± 7.7 | 19.1 ± 9.5 | 16.9 ± 9.1 | <0.001 |
| Initiated osteoporosis treatment, n (%) | 2127 (32.0) | 1570 (28.4) | 483 (52.3) | 74 (36.3) | <0.001 |
- S = suppressed small cell size.
- a Value of p for test that VFA-positive and VFA-negative groups are not significantly different.
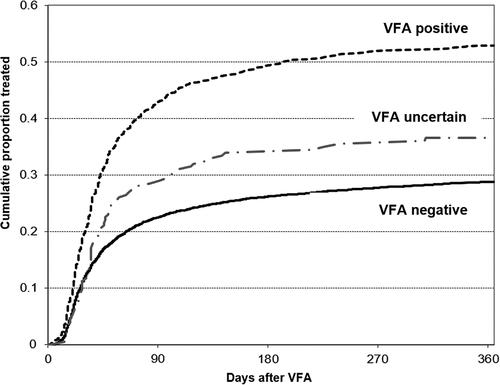
Compared to those with a negative VFA, those with a positive VFA had an unadjusted OR of 2.77 (95% CI, 2.40 to 3.19) for commencement of fracture prevention medication. These associations changed little with adjustment for FRAX as a continuous measure (OR 2.37; 95% CI, 2.04 to 2.75), FRAX risk category (OR 2.41; 95% CI, 2.08 to 2.80) or BMD T-score category (OR 2.38; 95% CI, 2.03 to 2.79). Among those with an uncertain VFA, possible prevalent vertebral fractures had weaker but still statistically significant associations with subsequent dispensation of a fracture prevention medication compared to those with a negative VFA (Table 2). No differences were noted in these results for men compared to women (p value = 0.85 for interaction term between VFA status and sex); the unadjusted association of a positive VFA with subsequent initiation of fracture prevention medication was as strong in men (OR 3.32; 95% CI, 2.12 to 5.21) as in women (OR 2.79; 95% CI, 2.40 to 3.24).
| Study population subset | Prevalent vertebral fracture status (n) | OR (95% CI)b |
|---|---|---|
| All | VFA positive (n = 923) | 2.77 (2.40 to 3.19) |
| VFA uncertain (n = 204) | 1.43 (1.07 to 1.92) | |
| FRAX MOF subsets | ||
| FRAX 10-year MOF risk <10% | VFA positive (n = 132) | 4.18 (2.84 to 6.16) |
| VFA uncertain (n = 36) | 1.55 (0.67 to 3.61) | |
| FRAX 10-year MOF 10% to 20% | VFA positive (n = 436) | 2.99 (2.43 to 3.66) |
| VFA uncertain (n = 113) | 1.44 (0.97 to 2.15) | |
| FRAX 10-year MOF >20% | VFA positive (n = 355) | 1.44 (1.14 to 1.83) |
| VFA uncertain (n = 55) | 1.14 (0.66 to 1.96) | |
| BMD T-score subsets | ||
| BMD category: osteopenia | VFA positive (n = 327) | 4.51 (3.48 to 5.85) |
| VFA uncertain (n = 101) | 1.80 (1.06 to 3.08) | |
| BMD category: osteoporosis | VFA positive (n = 576) | 1.72 (1.43 to 2.08) |
| VFA uncertain (n = 101) | 1.25 (0.84 to 1.87) |
- a Reference category for all models: VFA negative.
- b Associations significant at p value <0.5 are in bold.
Across subsets defined by FRAX risk category, a positive VFA was most strongly associated with filling a prescription for a fracture prevention medication compared to negative VFA in the subset with a FRAX 10-year MOF risk of <10% (OR 4.18; 95% CI, 2.84 to 6.16), versus the subset with a FRAX 10-year risk of 10% to 20% (OR 2.99; 95% CI, 2.43 to 3.66), and versus the subset with a FRAX 10-year risk of >20% (OR 1.44; 95% CI, 1.14 to 1.83, p value < 0.001 for interaction between prevalent vertebral fracture status and FRAX risk category, Table 2). The absolute increase in percentages prescribed medication in those with a positive compared to a negative VFA was 25.9% for those with FRAX 10-year risk <10%, 25.2% for those with FRAX 10-year risk of 10% to 20%, and 9.1% for those with FRAX 10-year risk >20% (Fig. 3).
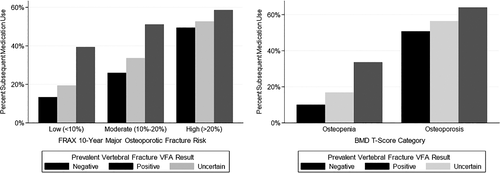
Similarly, a positive VFA was much more strongly associated with filling a prescription for a fracture prevention medication compared to a negative VFA among those with osteopenia (OR 4.51; 95% CI, 3.48 to 5.85) compared to those with osteoporosis (OR 1.72; 95% CI, 1.43 to 2.08, p value < 0.001 for interaction between prevalent vertebral fracture status and BMD T-score category). The absolute increase in the proportions of those filling a fracture prevention medication following a positive vs negative VFA was 23.5% amongst those with osteopenia, compared to 13.2% amongst those with osteoporosis (Fig. 3).
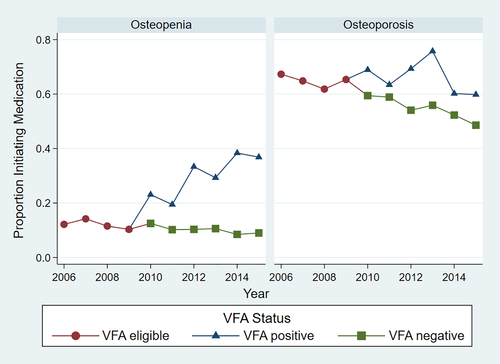
Interrupted time series analyses among all those with osteopenia who met criteria for a VFA showed stable rates of fracture prevention medication initiation over the years 2006 through 2010 (Fig. 4). Starting in 2010 there is a substantial increase in fracture prevention medication use amongst those with osteopenia and a positive VFA, and stable medication use among those with a negative VFA similar to all osteopenic individuals eligible for VFA years 2006 through 2009. Among all those with osteoporosis eligible for a VFA, there is a gradual decline in fracture prevention medication use from 2006 through 2010. In subsequent years there is a mild increase in those with a positive VFA compared to all who are VFA eligible, but a further decline in treatment rates for those with osteoporosis and a negative VFA at a rate similar to that seen prior to 2010.
Discussion
In this large population-based bone densitometry program, identification of prevalent vertebral fracture on VFA images at the time of a bone density test substantially influenced subsequent use of fracture prevention medication. This reflects both physician behavior (prescription of medication) and patient medication use behavior (going to pharmacy to have medication filled). This is the first study to our knowledge to show that documentation of prevalent vertebral fracture on any imaging modality in usual clinical practice increases fracture prevention medication use.
The impact was greatest in those without osteoporosis by BMD criteria, and in those judged by FRAX (before VFA results are known) to be at low-to-moderate risk of fracture with no evidence of a decrease in medication use among those with osteopenia and a negative VFA. The prevalence of vertebral fracture on VFA in these individuals is about 10%, but without documentation of their vertebral fracture these individuals are much less likely to be considered candidates for pharmacologic fracture prevention therapy. This is important, because the majority of incident osteoporotic fractures occur in those who do not have osteoporosis by BMD criteria29 and are designated to be at low-to-moderate fracture risk by FRAX before VFA results are known.30 Moreover, fracture prevention medication therapies have been proven to effectively reduce incident nonvertebral and (especially) vertebral fractures among those who have a prevalent vertebral fracture, regardless of BMD.31-35
Even among those with osteoporosis by BMD criteria or who before VFA results are known are designated to be at high fracture risk, who commonly decline recommended fracture prevention medication therapy,36, 37 we saw a moderate association of positive VFA with subsequent use of fracture prevention medication. Positive VFA has been shown in one prior study to be associated with increased patient perceived need for fracture prevention medication independent of BMD and other prior fracture history.38 Hence, our data is consistent with the hypothesis that among those with osteoporosis by BMD criteria VFA may have a role to play encouraging appropriate fracture prevention medication use. However, our time series analysis does not rule out the possibility that a negative VFA may be associated with a further decline in fracture medication use among those with osteoporosis, although this could also reflect declines over the past decade in osteoporosis treatment rates independent of VFA. Further research is needed to understand how patients and physicians are using VFA results to make fracture prevention treatment decisions. These results strongly suggest that if VFA is performed among those satisfying other indications for treatment, care has to be taken to communicate to providers if (and why) fracture prevention therapy is indicated in spite of a negative VFA.
Both the International Society for Clinical Densitometry39, 40 and the National Osteoporosis Foundation8 have issued guidelines recommending targeted use of VFA at the time of bone densitometry to identify those with clinically unrecognized prevalent vertebral fracture, who therefore are candidates for fracture prevention therapy. However, VFA remains underutilized in most healthcare settings, perhaps because the accuracy and utility of the procedure are unclear to many healthcare providers and payers. In Canada, Manitoba is the only province that currently systematically employs VFA as part of their provincial bone densitometry and fracture assessment protocols. VFA at the time of bone densitometry is inexpensive, convenient, point-of-care testing with minimal patient radiation exposure and minimal added bone technologist time commitment to perform.13, 41-44 Our study and others19, 42 have shown that bone density technologists can successfully implement a decision rule to identify those referred for bone densitometry as also appropriate candidates for VFA. Prior studies that have shown that clinicians can be easily trained to identify vertebral fractures on lateral spine images.41, 45, 46 Recent studies have shown that prevalent vertebral fracture specifically identified on densitometric VFA images obtained at the time of bone densitometry predict subsequent fractures independent of BMD and other risk factors,15-17 and this current study shows that VFA can appropriately influence provider and patient fracture prevention medication use behavior. All of these data now constitute a comprehensive evidence base that strongly supports and can be used to promote systematic targeted VFA imaging at the point of bone density care by healthcare delivery organizations as part of a broader strategy to close the treatment gap for those who have an indication for fracture prevention medication.
A limitation of our study is that we do not know how physicians communicated VFA results to their patients, nor how well patients grasped their meaning. However, suboptimal communication to patients regarding the presence of their vertebral fracture and its significance would be expected to dampen the effect on patient medication use and bias our results toward the null. Hence our results and conclusions are robust to this limitation. Further research is warranted to investigate whether patient use of fracture prevention medication among those with a prevalent vertebral fracture is influenced by provider communication strategies regarding the VFA results, and patient understanding of the impact that prevalent vertebral fracture has on their subsequent risk of fractures and related morbidity.
A second limitation of our study is that we cannot in this observational cohort study prove that this targeted VFA imaging strategy reduces incident fractures, due to selection bias and confounding by indication. Additional limitations are that the Manitoba population is largely white, and it is not clear how applicable our results are to other countries and non-white populations. The study population reflects the selection filter of who is referred (and accepts that referral) for bone densitometry. In Manitoba, although all residents of have access to bone densitometry services under their provincial single-payer healthcare system, DXA is covered for all women over age 65 years, but only for women younger than 65 years and men who have additional fracture risk factors.47 These criteria may vary across different countries, geographic regions, and subsets of the older population. Finally, our associations of positive VFA with subsequent medication use were adjusted for FRAX risk score rather than FRAX individual fracture risk factors and does not fully account for time since prior fracture, fracture site, or for falls. However, we think it is highly unlikely our results would be altered by adjustment for these additional covariates.
There are important strengths of this study. The study setting is a large geographic area (an entire Canadian province). The study was conducted in usual clinical care, as opposed to populations selected specifically for a research study; hence, our results represent real-world clinical performance and outcomes. Our study sample size is large and representative of the broad older population referred for bone densitometry.
In conclusion, identification of prevalent vertebral fractures on VFA images is strongly associated with subsequent use of fracture prevention medication. The effect of VFA imaging was greatest among those without osteoporosis by BMD criteria and those who (in the absence of a prevalent vertebral fracture) would be judged to be at low-or-moderate risk of fracture. These data lend support to targeted use of VFA for older men and postmenopausal women referred for bone densitometry, strongly suggesting that this practice would help address declining rates of fracture prevention therapy among those at high risk of future fractures.
Disclosures
SNM discloses that she has research grants from Amgen Inc. and Merck Inc, paid to her institution, the Research Institute of the McGill University Health Centre. All other authors have no conflicts of interest to disclose.
Acknowledgments
We acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC 2016/2017-29). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, Seniors and Active Living, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee. Manitoba Health data-sharing agreements prohibit data sharing outside of the province.
Authors' roles
JTS: study concept and design, drafting of manuscript, critical review and revision of manuscript. LML: data acquisition and analysis, critical review and revision of manuscript. SNM: critical review and revision of manuscript. SD: critical review and revision of manuscript. MB: critical review and revision of manuscript. MA: critical review and revision of manuscript. WDL: study concept and design, data acquisition and analysis, critical review, and revision of manuscript.




