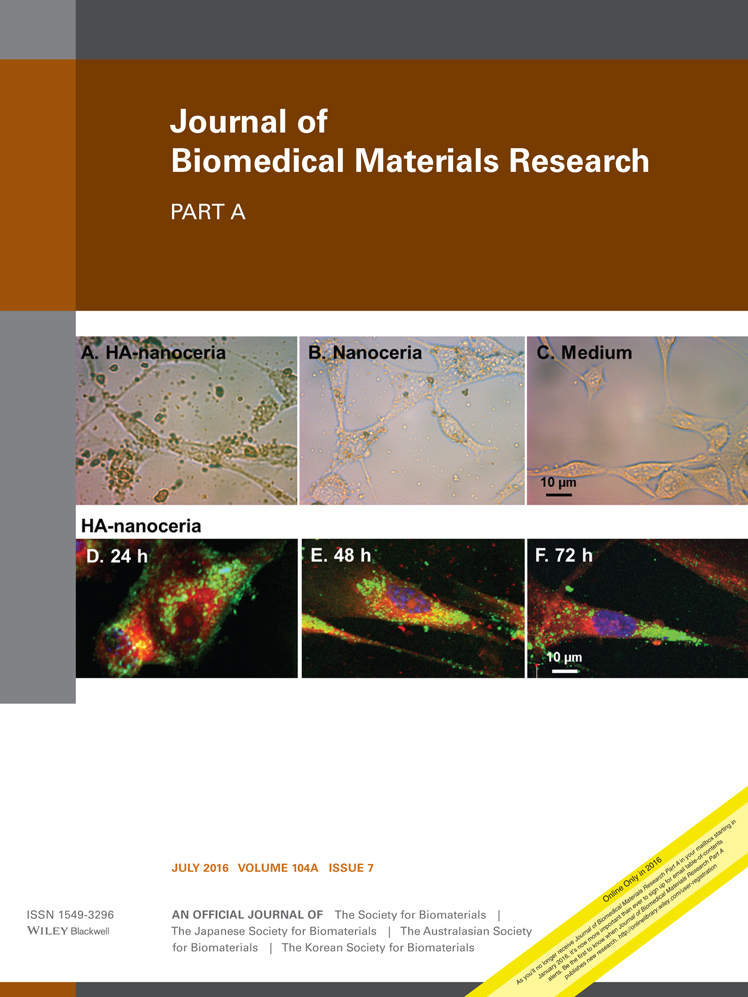
Sequential culture on biomimetic nanoclay scaffolds forms three-dimensional tumoroids
Corresponding Author
Kalpana S. Katti
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Correspondence to: K.S. Katti; e-mail: [email protected]Search for more papers by this authorMD Shahjahan Molla
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorFataneh Karandish
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorManas K. Haldar
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorSanku Mallik
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorDinesh R. Katti
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorCorresponding Author
Kalpana S. Katti
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Correspondence to: K.S. Katti; e-mail: [email protected]Search for more papers by this authorMD Shahjahan Molla
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorFataneh Karandish
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorManas K. Haldar
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorSanku Mallik
Department of Pharmaceutical Sciences, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorDinesh R. Katti
Department of Civil and Environmental Engineering, North Dakota State University, Fargo, North Dakota, 58105
Search for more papers by this authorAbstract
In recent times, the limitation of two-dimensional cultures and complexity of in vivo models has paved the way for the development of three-dimensional models for studying cancer. Here we report the development of a new tumor model using PCL/HAPClay scaffolds seeded with a sequential culture of human mesenchymal stem cells (hMSCs) followed by human prostate cancer cells (HPCCs). This nanocomposite system is used as a test-bed for studying cancer metastasis and efficacy of anti-cancer drugs using a polymersome delivery method. A novel sequential cell culture system in three-dimensional in vitro bone model provides a unique bone mimetic environment. The hMSCs seeded scaffolds are seeded with prostate cancer cells after the hMSCs have differentiated into osteoblasts. Sequential culture on the scaffolds has shown formation of tumoroids or microtissue consisting of organized, densely packed round cells with hypoxic core regions similar to in vivo tumors. Such tumoroids are not observed on HPCC seeded scaffolds or when HPCCs sequentially cultured with human osteoblast cells. Clearly, the newly differentiated hMSCs play a vital role in the ability of cancer cells to grow into tumoroids and cause disease. The PCL/HAPclay scaffold system seeded with the sequential culture of hMSCs, and HPCCs presents a good model system for study of the interactions between prostate cancer cells and bone microenvironment. © 2016 Wiley Periodicals, Inc. J Biomed Mater Res Part A: 104A: 1591–1602, 2016.
REFERENCES
- 1Gill BJ, West JL. Modeling the tumor extracellular matrix: Tissue engineering tools repurposed towards new frontiers in cancer biology. J Biomech 2014; 47: 1969–1978.
- 2Verbridge SS, Chandler EM, Fischbach C. Tissue-engineered three-dimensional tumor models to study tumor angiogenesis. Tissue Eng Part A 2010; 16: 2147.
- 3Hutchinson L, Kirk R. High drug attrition rates—Where are we going wrong? Nat Rev Clin Oncol 2011; 8: 189–190.
- 4Bissell MJ, Radisky D. Putting tumours in context. Nat Rev Cancer 2001; 1: 46–54.
- 5Yoshii Y, Waki A, Yoshida K, Kakezuka A, Kobayashi M, Namiki H, Kuroda Y, Kiyono Y, Yoshii H, Furukawa T, Asai T, Okazawa H, Gelovani JG, Fujibayashi Y. The use of nanoimprinted scaffolds as 3D culture models to facilitate spontaneous tumor cell migration and well-regulated spheroid formation. Biomaterials 2011; 32: 6052–6058.
- 6Lin RZ, Chang HY. Recent advances in three-dimensional multicellular spheroid culture for biomedical research. Biotechnol J 2008; 3: 1172–1184.
- 7Elliott NT, Yuan F. A review of three-dimensional in vitro tissue models for drug discovery and transport studies. J Pharm Sci 2011; 100: 59–74.
- 8Bissell MJ, Kenny PA, Radisky DC. Microenvironmental regulators of tissue structure and function also regulate tumor induction and progression: The role of extracellular matrix and its degrading enzymes. Cold Spring Harbor Symp Quant Biol 2005; 70: 343.
- 9Ng KW, Leong DTW, Hutmacher DW. The challenge to measure cell proliferation in two and three dimensions. Tissue Eng 2005; 11: 182–191.
- 10Faute MAD, Laurent L, Ploton D, Poupon MF, Jardillier JC, Bobichon H. Distinctive alterations of invasiveness, drug resistance and cell-cell organization in 3D-cultures of MCF-7, a human breast cancer cell line, and its multidrug resistant variant. Clin Exp Metastasis 2002; 19: 161−168.
- 11Leung M, Kievit FM, Florczyk SJ, Veiseh O, Wu J, Park JO, Zhang MQ. Chitosan-alginate scaffold culture system for hepatocellular carcinoma increases malignancy and drug resistance. Pharm Res 2010; 27: 1939–1948.
- 12Beningo KA, Dembo M, Wang YI. Responses of fibroblasts to anchorage of dorsal extracellular matrix receptors. Proc Natl Acad Sci USA 2004; 101: 18024–18029.
- 13Rhodes NP, Srivastava JK, Smith RF, Longinotti C. Metabolic and histological analysis of mesenchymal stem cells grown in 3-D hyaluronan-based scaffolds. J Mater Sci: Mater Med 2004; 15: 391–395.
- 14Ghosh S, Spagnoli GC, Martin I, Ploegert S, Demougin P, Heberer M, Reschner A. Three-dimensional culture of melanoma cells profoundly affects gene expression profile: A high density oligonucleotide array study. J Cell Physiol 2005; 204: 522.
- 15Kenny PA, Lee GY, Myers CA, Neve RM, Semeiks JR, Spellman PT, Lorenz K, Lee EH, Barcellos-Hoff MH, Petersen OW, Gray JW, Bisell MJ. The morphologies of breast cancer cell lines in three-dimensional assays correlate with their profiles of gene expression. Mol Oncol 2007; 1: 84–96.
- 16Jarrahy R, Huang W, Rudkin GH, Lee JM, Ishida K, Berry MD, Sukkarieh M, Wu BM, Yamaguchi DT, Miller TA. Osteogenic differentiation is inhibited and angiogenic expression is enhanced in MC3T3-E1 cells cultured on three-dimensional scaffolds. Am J Physiol Cell Physiol 2005; 289: C408.
- 17Wolf K, Friedl P. Mapping proteolytic cancer cell-extracellular matrix interfaces. Off J Metastasis Res Soc 2009; 26: 289–298.
- 18Talukdar S, Kundu SC. Engineered 3D Silk-based metastasis models: Interactions between human breast adenocarcinoma, mesenchymal stem cells and osteoblast-like cells. Adv Funct Mater 2013; 23: 5249–5260.
- 19Marlow R, Honeth G, Lombardi S, Cariati M, Hessey S, Pipili A, Mariotti V, Buchupalli B, Foster K, Bonnet D, Grigoriadis A, Rameshwar P, Purushotham A, Tutt A, Dontu G. A novel model of dormancy for bone metastatic breast cancer cells. Cancer Res 2013; 73: 6886.
- 20Fischbach C, Chen R, Matsumoto T, Schmelzle T, Brugge JS, Polverini PJ, Mooney DJ. Engineering tumors with 3D scaffolds. Nat Methods 2007; 4: 855.
- 21Wang X, Sun L, Maffini MV, Soto A, Sonnenschein C, Kaplan DL. A complex 3D human tissue culture system based on mammary stromal cells and silk scaffolds for modeling breast morphogenesis and function. Biomaterials 2010; 31: 3920–3929.
- 22Roussos ET, Condeelis JS, Patsialou A. Chemotaxis in cancer. Nat Rev Cancer 2011; 11: 573–587.
- 23Adjei IM, Blanka S. Modulation of the tumor microenvironment for cancer treatment: a biomaterials approach. J Funct Biomater 2015; 6: 81–103.
- 24Kwon H, Kim HJ, Rice WL, Subramanian B, Park SH, Georgakoudi I, Kaplan DL. Development of an in vitro model to study the impact of BMP-2 on metastasis to bone. J Tissue Eng Regenerative Med 2010; 4: 590–599.
- 25Hartman O, Zhang C, Adams EL, Farach-Carson MC, Petrelli NJ, Chase BD, Rabolt JF. Biofunctionalization of electrospun PCL-based scaffolds with perlecan domain IV peptide to create a 3-D pharmacokinetic cancer model. Biomaterials 2010; 31: 5700–5718.
- 26Pathi SP, Lin DDW, Dorvee JR, Estroff LA, Fischbach C. Hydroxyapatite nanoparticle-containing scaffolds for the study of breast cancer bone metastasis. Biomaterials 2011; 32: 5112–5122.
- 27Pranav S, Kelber JA, Lee JW, Wright TN, Vecchio KS, Klemke RL, Chen SC. Cancer cell migration within 3D layer-by-layer microfabricated photocrosslinked PEG scaffolds with tunable stiffness. Biomaterials 2012; 33: 7064–7070.
- 28Szot CS, Buchanan CF, Freeman JW, Rylander MN. 3D in vitro bioengineered tumors based on collagen I hydrogels. Biomaterials 2011; 32: 7905–7912.
- 29Sieh S, Taubenberger AV, Lehman ML, Clements JA, Nelson CC, Hutmacher DW. Paracrine interactions between LNCaP prostate cancer cells and bioengineered bone in 3D in vitro culture reflect molecular changes during bone metastasis. Bone 2014; 63: 121–131.
- 30Bersini S, Jeon JS, Dubini G, Arrigoni C, Chung S, Charest JL, Moretti M, Kamm RD. A microfluidic 3D in vitro model for specificity of breast cancer metastasis to bone. Biomaterials 2014; 35: 2454–2461.
- 31Seib FP, Berry JE, Shiozawa Y, Taichman RS, Kaplan DL. Tissue engineering a surrogate niche for metastatic cancer cells. Biomaterials 2015; 51: 313–319.
- 32Subia B, Dey T, Sharma S, Kundu SC. Target specific delivery of anticancer drug in silk fibroin based 3D distribution model of bone-breast cancer cells. ACS Appl Mater Interfaces 2015; 7: 2269–2279.
- 33Vu LT, Jain G, Veres BD, Rajagopalan P. Cell migration on planar and three-dimensional matrices: A hydrogel-based perspective. Tissue Eng Part B 2015; 21: 67–74.
- 34Zhu W, Wang M, Fu Y, Castro NJ, Fu SW, Zhang LG. Engineering a biomimetic three-dimensional nanostructured bone model for breast cancer bone metastasis study. Acta Biomater 2015; 14: 164–174.
- 35Suzuki K, Sun R, Origuchi M, Kanehira M, Takahata T, Itoh J, Umezawa A, Kijima H, Fukuda S, Saijo Y. Mesenchymal stromal cells promote tumor growth through the enhancement of neovascularization. Mol Med 2011; 17: 579–587.
- 36Qiao L, Xu Z, Zhao T, Zhao Z, Shi M, Zhao RC, Ye L, Zhang X. Suppression of tumorigenesis by human mesenchymal stem cells in a hepatoma model. Cell Res 2008; 18: 500–507.
- 37Wakitani S, Goto T, Pineda SJ, Young RG, Mansour JM, Caplan AI, Goldberg VM. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am 1994; 76: 579–592.
- 38Beresford JN. Osteogenic stem cells and the stromal system of bone and marrow. Clin Orthop Relat Res 1989; 240: 270–280.
- 39Beresford JN, Bennett JH, Devlin C, Leboy PS, Owen ME. Evidence for an inverse relationship between the differentiation of adipocytic and osteogenic cells in rat marrow stromal cell cultures. J Cell Sci 1992; 102: 341–351.
- 40Saito T, Dennis JE, Lennon DP, Young RG, Caplan AI. Myogenic expression of mesenchymal stem cells within myotubes of mdx mice in vitro and in vivo. Tissue Eng 1995; 1: 327–343.
- 41Bruder SP, Jaiswal N, Haynesworth SE. Growth kinetics, self-renewal, and the osteogenic potential of purified human mesenchymal stem cells during extensive subcultivation and following cryopreservation. J Cell Biochem 1997; 64: 278–294.
10.1002/(SICI)1097-4644(199702)64:2<278::AID-JCB11>3.0.CO;2-F CAS PubMed Web of Science® Google Scholar
- 42Jaiswal N, Haynesworth SE, Caplan AI, Bruder SP. Osteogenic differentiation of purified, culture-expanded human mesenchymal stem cells in vitro. J Cell Biochem 1997; 64: 295–312.
10.1002/(SICI)1097-4644(199702)64:2<295::AID-JCB12>3.0.CO;2-I CAS PubMed Web of Science® Google Scholar
- 43Katti KS, Ambre AH, Peterka N, Katti DR. Use of unnatural amino acids for design of novel organomodified clays as components of nanocomposite biomaterials. Philos Trans R Soc A Math Phys Eng Sci 2010; 368: 1963–1980.
- 44Ambre AH, Katti DR, Katti KS. Nanoclays mediate stem cell differentiation and mineralized ECM formation on biopolymer scaffolds. J Biomed Mater Res A 2013; 101: 2644–2660.
- 45Ambre AH, Katti DR, Katti KS. Biomineralized hydroxyapatite nanoclay composite scaffolds with polycaprolactone for stem cell based bone tissue engineering. J Biomed Mater Res A 2015; 103: 2077–2101.
- 46Boonrungsiman S, Gentleman E, Carzaniga R, Evans ND, McComb DW, Porter AE, Stevens MM. The role of intracellular calcium phosphate in osteoblast-mediated bone apatite formation. Proc Natl Acad Sci USA 2012; 109: 14170–14175.
- 47Katti KS, Ambre AH, Payne S, Katti DR. Vesicular delivery of crystalline calcium minerals to ECM in biomineralized nanoclay composites. Mater Res Expr 2015; 2: 8.
- 48Mahamid J, Sharir A, Gur D, Zelzer E, Addadi L, Weiner S. Bone mineralization proceeds through intracellular calcium phosphate loaded vesicles: A cryo-electron microscopy study. J Struct Biol 2011; 174: 527–535.
- 49Ambre AH, Katti DR, Katti KS. Biomineralized hydroxyapatite nanoclay composite scaffolds with polycaprolactone for stem cell-based bone tissue engineering. J Biomed Mater Res A 2015; 103: 2077–2101.
- 50Sharma A, Payne S, Katti KS, Katti DR. Evaluating molecular interactions in polycaprolactone-biomineralized hydroxyapatite nanocomposites using steered molecular dynamics. JOM 2015; 67: 733–743.
- 51Zorlutuna P, Annabi N, Camci-Unal G, Nikkhah M, Cha JM, Nichol JW, Manbachi A, Bae H, Chen S, Khademhosseini A. Microfabricated biomaterials for engineering 3D tissues. Adv Mater 2012; 24: 1782–1804.
- 52Fong ELS, Lamhamedi-Cherradi S-E, Burdett E, Ramamoorthy V, Lazar AJ, Kasper FK, Farach-Carson MC, Vishwamitra D, Demicco EG, Menegaz BA, Amin HM, Mikos AG, Ludwig JA. Modeling ewing sarcoma tumors in vitro with 3D scaffolds. Proc Natl Acad Sci USA 2013; 110: 6500–6505.
- 53Fong EL, Santoro M, Farach-Carson MC, Kasper FK, Mikos AG. Tissue engineering perfusable cancer models. Curr Opin Chem Eng 2014; 3: 112–117.
- 54Ambre A, Katti KS, Katti DR. In situ mineralized hydroxyapatite on amino acid modified nanoclays as novel bone biomaterials. Mater Sci Eng C Mater Biol Appl 2011; 31: 1017–1029.
- 55Verma D, Katti KS, Katti DR. Osteoblast adhesion, proliferation and growth on polyelectrolyte complex-hydroxyapatite nanocomposites. Philos Trans R Soc A Math Phys Eng Sci 2010; 368: 2083–2097.
- 56Khanna R, Katti KS, Katti DR. Bone nodules on chitosan-polygalacturonic acid-hydroxyapatite nanocomposite films mimic hierarchy of natural bone. Acta Biomater 2011; 7: 1173–1183.
- 57Nahire R, Haldar MK, Paul S, Ambre AH, Meghnani V, Layek B, Katti KS, Gange KN, Singh J, Sarkar K, Mallik S. Multifunctional polymersomes for cytosolic delivery of gemcitabine and doxorubicin to cancer cells. Biomaterials 2014; 35: 6482–6497.
- 58Toschi L, Finocchiaro G, Bartolini S, Gioia V, Cappuzzo F. Role of gemcitabine in cancer therapy. Fut Oncol 2005; 1: 7–17.
- 59Mussi S, Sawant R, Perche F, Oliveira M, Azevedo R, Ferreira LM, Torchilin V. Novel nanostructured lipid carrier co-loaded with doxorubicin and docosahexaenoic acid demonstrates enhanced in vitro activity and overcomes drug resistance in MCF-7/Adr cells. Pharm Res 2014; 31: 1882–1892.
- 60Liu Y, Fang J, Kim Y-J, Wong MK, Wang P. Codelivery of doxorubicin and paclitaxel by cross-linked multilamellar liposome enables synergistic antitumor activity. Mol Pharm 2014; 11: 1651–1661.
- 61Ambre AH, Katti DR, Katti KS. Nanoclays mediate stem cell differentiation and mineralized ECM formation on biopolymer scaffolds. J Biomed Mater Res A 2013; 101: 2644–2660.
- 62Ambre AH, Katti KS, Katti DR. Nanoclay based composite scaffolds for bone tissue engineering applications. J Nanotechnol Eng Med 2010; 1: 031013-031013.
- 63Katti DR, Ghosh P, Schmidt S, Katti KS. Mechanical properties of the sodium montmorillonite interlayer intercalated with amino acids. Biomacromolecules 2005; 6: 3276–3282.
- 64Chambers KF, Mosaad EMO, Russell PJ, Clements JA, Doran MR. 3D cultures of prostate cancer cells cultured in a novel high-throughput culture platform are more resistant to chemotherapeutics compared with cells cultured in monolayer. PloS one 2015; 10(4).
- 65Zhang C, Soori M, Miles FL, Sikes RA, Carson DD, Chung LWK, Farach-Carson MC. Paracrine factors produced by bone marrow stromal cells induce apoptosis and neuroendocrine differentiation in prostate cancer cells. Prostate 2011; 71: 157–167.
- 66Lee JS, Feijen J. Polymersomes for drug delivery: Design, formation and characterization. J Control Release 2012; 161: 473–483.
- 67Mayer LD, Tai LCL, Bally MB, Mitilenes GN, Ginsberg RS, Cullis PR. Characterization of liposomal systems containing doxorubicin entrapped in response to pH gradients. Biochim Biophys Acta 1990; 1025: 143–151.
- 68Logothetis CJ, Lin S-H. Osteoblasts in prostate cancer metastasis to bone. Nat Rev Cancer 2005; 5: 21–28.
- 69Pinski J, Parikh A, Bova GS, Isaacs JT. Therapeutic implications of enhanced G0/G1 checkpoint control induced by coculture of prostate cancer cells with osteoblasts. Cancer Res 2001; 61: 6372–6376.
- 70Berges RR, Vukanovic J, Epstein JI, CarMichel M, Cisek L, Johnson DE, Veltri RW, Walsh PC, Isaacs JT. Implication of cell kinetic changes during the progression of human prostatic cancer. Clin Cancer Res 1995; 1: 473–480.
- 71Reyes-Moreno C, Sourla A, Chpki I, Doillon C, Koutsilieris M. Osteoblast-derived survival factors protect PC-3 human prostate cancer cells from adriamycin apoptosis. Urology 1998; 52: 341–347.
- 72Bryden AA, Hoyland JA, Freemont AJ, Clarke NW, George NJ. Parathyroid hormone related peptide and receptor expression in paired primary prostate cancer and bone metastases. Br J Cancer 2002; 86: 322–325.
- 73Karaplis AC, Vautour L. Parathyroid hormone-related peptide and the parathyroid hormone/parathyroid hormone-related peptide receptor in skeletal development. Curr Opin Nephrol Hypertens 1997; 6: 308–313.
- 74Qin L, Li X, Ko J-K, Partridge NC. Parathyroid hormone uses multiple mechanisms to arrest the cell cycle progression of osteoblastic cells from G1 to S phase. J Biol Chem 2005; 280: 3104–3111.
- 75Plaisant M, Giorgetti-Peraldi S, Gabrielson M, Loubat A, Dani C, Peraldi P. Inhibition of hedgehog signaling decreases proliferation and clonogenicity of human mesenchymal stem cells. PLoS One 2011; 6: e16798.
- 76Filipak M, Estervig DN, Tzen CY, Minoo P, Hoerl BJ, Maercklein PB, Zschunke MA, Edens M, Scott RE. Integrated control of proliferation and differentiation of mesenchymal stem cells. Environ Health Perspect 1989; 80: 117–125.
- 77Mets T, Verdonk G. In vitro aging of human bone marrow derived stromal cells. Mech Ageing Dev 1981; 16: 81–89.
- 78Gotoh Y, Hiraiwa K, Nagayama M. In vitro mineralization of osteoblastic cells derived from human bone. Bone Miner 1990; 8: 239–250.
- 79Stiehler M, Bunger C, Baatrup A, Lind M, Kassem M, Mygind T. Effect of dynamic 3-D culture on proliferation, distribution, and osteogenic differentiation of human mesenchymal stem cells. J Biomed Mater Res A 2009; 89: 96–107.
- 80Thibault RA, Scott Baggett L, Mikos AG, Kasper FK. Osteogenic differentiation of mesenchymal stem cells on pregenerated extracellular matrix scaffolds in the absence of osteogenic cell culture supplements. Tissue Eng Part A 2010; 16: 431–440.
- 81Yang J, Fizazi K, Peleg S, Sikes CR, Raymond AK, Jamal N, Hu M, Olive M, Martinez LA, Wood CG, Logothetis CJ, Karsenty G, Navone NM. Prostate cancer cells induce osteoblast differentiation through a Cbfa1-dependent pathway. Cancer Res 2001; 61: 5652–5659.
- 82Lian JB, Stein GS. Concepts of osteoblast growth and differentiation: basis for modulation of bone cell development and tissue formation. Crit Rev Oral Biol Med 1992; 3: 269–305.
- 83Sieh S, Lubik AA, Clements JA, Nelson CC, Hutmacher DW. Interactions between human osteoblasts and prostate cancer cells in a novel 3D in vitro model. Organogenesis 2010; 6: 181–188.
- 84Girard YK, Wang C, Ravi S, Howell MC, Mallela J, Alibrahim M, Green R, Hellermann G, Mohapatra SS, Mohapatra S. A 3D fibrous scaffold inducing tumoroids: A platform for anticancer drug development. PLoS One 2013; 8: e75345.
- 85Luo J, Lee SO, Liang L, Huang CK, Li L, Wen S, Chang C. Infiltrating bone marrow mesenchymal stem cells increase prostate cancer stem cell population and metastatic ability via secreting cytokines to suppress androgen receptor signaling. Oncogene 2014; 33: 2768–2778.
- 86Ishaug SL, Crane GM, Miller MJ, Yasko AW, Yaszemski MJ, Mikos AG. Bone formation by three-dimensional stromal osteoblast culture in biodegradable polymer scaffolds. J Biomed Mater Res 1997; 36: 17–28.
10.1002/(SICI)1097-4636(199707)36:1<17::AID-JBM3>3.0.CO;2-O CAS PubMed Web of Science® Google Scholar
- 87Zou X, Li H, Baatrup A, Lind M, Bunger C. Engineering of bone tissue with porcine bone marrow stem cells in three-dimensional trabecular metal: in vitro and in vivo studies. APMIS Suppl 2003; 127–132.
- 88Ghosh A, Heston WDW. Tumor target prostate specific membrane antigen (PSMA) and its regulation in prostate cancer. J Cell Biochem 2004; 91: 528–539.
- 89Yao V, Berkman CE, Choi JK, O'Keefe DS, Bacich DJ. Expression of prostate-specific membrane antigen (PSMA), increases cell folate uptake and proliferation and suggests a novel role for PSMA in the uptake of the non-polyglutamated folate, folic acid. Prostate 2010; 70: 305–316.
- 90Saito G, Swanson JA, Lee KD. Drug delivery strategy utilizing conjugation via reversible disulfide linkages: Role and site of cellular reducing activities. Adv Drug Deliv Rev 2003; 55: 199–215.
- 91West KR, Otto S. Reversible covalent chemistry in drug delivery. Curr Drug Discov Technol 2005; 2: 123–160.