The Association Between Recreational Cannabis Use and 24-hour Movement Behaviours: Perceptions of Youth Citizen Scientists
ABSTRACT
Introduction
The prevalence of cannabis use among youth is rising globally, making it crucial to understand its role in health and well-being. While cannabis use is linked to various health outcomes, evidence on its relationship with 24-h movement behaviours (moderate-to-vigorous physical activity, sedentary behaviour, and sleep) in youth is limited. This study uses a digital citizen science approach to examine these associations among Canadian youth aged 13 to 21 years.
Methods
As a part of the Smart Platform, a digital citizen science initiative for ethical population health surveillance and policy interventions, this study engaged with 208 youth citizen scientists from Saskatchewan, Canada (August to December 2018). Participants used their smartphones to report moderate-to-vigorous physical activity, sedentary behaviour, sleep, substance use, mental health, and sociodemographic data over eight consecutive days. Linear regression models assessed associations between cannabis use and 24-h movement behaviours. Sedentary behaviour was further stratified into recreational screen time and other sedentary behaviour to explore distinct relationships with cannabis use.
Results
After adjusting for age, gender, parental education, and school, cannabis use was associated with higher hours/day of sedentary behaviour in the overall (β = 8.92, 95% CI = 1.11, 16.72; p-value = 0.02) and weekend models (β = 5.32, 95% CI = 0.89, 9.75; p-value = 0.02). Cannabis use was also associated with higher recreational screen time in both overall (β = 4.65, 95% CI = 0.19, 9.13; p-value = 0.04) and weekend models (β = 2.70, 95% CI = 0.08, 5.32; p-value = 0.04).
Conclusions
These findings need to be confirmed with longitudinal studies to develop holistic population health interventions focusing on policy solutions to address complex negative behaviours among youth.
1 Introduction
Cannabis is the most commonly used illicit psychoactive substance among youth in the world (UN 2018). Although many countries such as Canada have legalized recreational cannabis use, defined as the nonmedical use of cannabis for its psychoactive effects, while restricting cannabis sales to youth below the age of 18 years, youth seem to have easy access to cannabis (Nguyen and Mital 2022; Wadsworth et al. 2022), with evidence indicating that substance use is more common during youth (West et al. 2020; Lesjak and Stanojević-Jerković 2015). For instance, cannabis use was found to be two times higher among Canadian youth aged 15–24, compared to adults aged 25–64, with 26% of youth aged 20-24 using cannabis daily or almost daily in the past year Canada 2020. Similarly, an increasing trend of cannabis use was found among Canadian students in grades 7–12 (7% in grades 7 to 9% and 29.4% in grades 10–12) (Canada 2022).
The rising prevalence of recreational cannabis use is concerning because despite the growing evidence of the medicinal benefits of cannabis (Bridgeman and Abazia 2017), research on the benefits of cannabis use has primarily been conducted on adults (Nugent et al. 2017; Walsh et al. 2017). Moreover, evidence shows that cannabis has several negative impacts on youth (Grant and Bélanger 2017; Jager et al. 2010; Doggett et al. 2019). For instance, evidence indicates that cannabis use has been associated with adverse educational and mental health outcomes among youth (Grant and Bélanger 2017; Jager et al. 2010). Cannabis use has also been reported to contribute to substance use disorders, particularly when it becomes frequent, heavy, and commences at an early age (Doggett et al. 2019). Numerous studies not only indicate that cannabis use among adolescents is associated with a higher risk of depression, anxiety and suicidality in young adulthood (Fresán et al. 2022; Gobbi et al. 2019), but cannabis use is also making youth three times more likely to experience new onset of manic symptoms (Gibbs et al. 2015). There is some evidence suggesting that medical cannabis use may be used as a therapeutic intervention among youth for chemotherapy-induced nausea and vomiting, multiple sclerosis, epilepsy, chronic pain, and inflammatory bowel disease (Wong et al. 2017); however, studies also indicate that given the potential adverse effects of cannabis, additional research is needed to evaluate the impact of recreational cannabis use in apparently healthy or asymptomatic youth (Solmi et al. 2023; Stockings et al. 2018). The developmental transitions that occur during youth, biologically, psychologically, and socially, make this period critical for studying how cannabis use may influence healthy behaviours, such as moderate-to-vigorous physical activity (MVPA), sedentary behaviour (SB), and sleep (Backes and Bonnie 2019).
Social Cognitive Theory (SCT) posits that behaviour is influenced by the interaction between personal, environmental, and behavioural factors, with a focus on self-regulation, observational learning, and self-efficacy (Schunk and DiBenedetto 2023). SCT suggests that cognitive processes, such as motivation and self-regulation, influence how cannabis use impacts movement behaviours. A key component of SCT is reciprocal determinism – behaviour not only responds to cognitive and environmental influences but also shapes them over time. For instance, youth with cannabis-related motivation deficits may experience greater reductions in physical activity due to diminished self-efficacy and lower outcome expectations regarding exercise. In contrast, the Social Ecological Model (SEM) emphasizes that behaviour is influenced by multiple layers, from individual factors to social, community, and policy levels (Kilanowski 2017). SEM highlights how social norms, peer pressure, community resources, and access to recreational spaces shape the relationship between cannabis use and movement behaviours. For example, neighbourhood safety and cultural attitudes toward cannabis use can modify the effects of cannabis on physical activity and sleep. Additionally, the Biopsychosocial Model (BPS) underscores the interaction between biological, psychological, and social factors in shaping health behaviours (Lugg 2022). This model suggests that mental health and motivation can interact with the physiological effects of cannabis, amplifying or mitigating its impact on movement behaviours. Youth with cannabis-induced motivation deficits may show more pronounced reductions in physical activity or increased SB, especially in contexts where inactivity is normalized.
Although individual studies have linked cannabis use to reduced physical activity among adults (Boutouis et al. 2024; Merrill et al. 2024), there is a dearth of recent evidence on the relationship between cannabis use and 24-h movement behaviours among youth (Neilson and Lin 2019; Coelho et al. 2023). Additionally, research on the relationship between cannabis use and 24-h movement behaviours within the same cohort of youth is limited (Vancampfort et al. 2019a). Given the health benefits of adhering to 24-h movement guidelines, such as reduced risks of mortality, cardiovascular diseases, type 2 diabetes, cancers, negative mental health outcomes, and dementia in adulthood (Tremblay et al. 2016), it is crucial to address this gap. Moreover, there is a lack of data collected through youth-owned digital devices, despite their potential to reduce stigma and improve compliance (Wies et al. 2021; Katapally et al. 2021). With nearly universal smartphone ownership among youth in Western nations (Ratham; 2023; Government of Canada 2023; Rideout 2015), digital approaches offer an effective means of studying cannabis use in this population. This study, using a digital citizen science approach (Katapally, Bhawra, et al. 2018; Katapally 2019; Katapally and Chu 2020; Katapally 2022; Hammami and Katapally 2022), aims to explore the association between cannabis use and 24-h movement behaviours, including MVPA, SB, and sleep, in youth aged 13–21 years, providing valuable insights for public health strategies and interventions.
2 Methods
2.1 Study Design
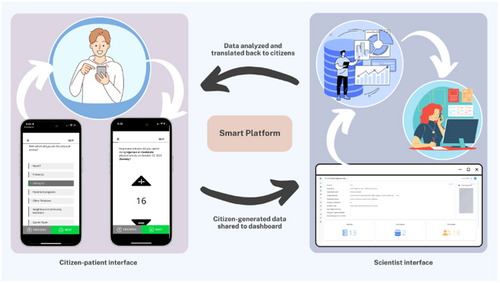
This study is a part of the Smart Platform, a citizen science initiative for ethical surveillance, integrated knowledge translation and policy, and real-time interventions (Katapally 2019; Katapally and Chu 2020). This cross-sectional study engaged 208 youth citizen scientists (aged 13–21 years) over 8 days in the provincial capital city of Regina, Saskatchewan, Canada (Katapally, Bhawra, et al. 2018). Ethics approval was obtained from the universities of Regina and Saskatchewan through a synchronized review protocol (EB # 2017-29) before any data collection. All data were obtained via time-triggered retrospective validated measures deployed via a custom-designed application (app) downloaded onto youth-owned smartphones (Katapally, Bhawra, et al. 2018).
2.2 Recruitment
Of the twelve high schools in the city of Regina that were approached to participate in the study, five schools agreed to participate. Only youth whose parents or caregivers did not object to their participation and who confirmed that they did not have any medical condition that prevented them from being physically active were recruited. The schools emailed implied informed consent forms to parents and caregivers of youth aged 13–16 1 week before recruitment. The Smart Platform team coordinated closely with each school and conducted separate recruitment presentations to students in each grade (grades 8–12). Following the class presentations, youth who chose to participate in the study downloaded a custom-built app on their smartphones and provided informed consent via the app (Figure 1).
Once youth joined the study via the app, retrospective measures were time-triggered and completed in the presence of the research team on day one of the study. These measures included validated questionnaires on various health behaviours and outcomes, including MVPA, ST, SB, sleep, school environment, bullying, substance use, and mental health. To be included in the study, youth must have provided complete data pertaining to cannabis use via the retrospective measures.
2.3 Measures
2.3.1 MVPA (Outcome Variable)
MVPA was captured using a modified version of the International Physical Activity Questionnaire (IPAQ). The IPAQ has demonstrated strong test-retest reliability (ICC = 0.71–0.89) and weak to modest criterion validity when compared to accelerometer data (ρ = 0.15–0.26) in youth populations (Dinger et al. 2006). Youth were asked: “How many minutes did you spend doing vigorous or moderate physical activity on each day of the week?” (Open-ended) depending on when the youth citizen scientist joined the study. For instance, if a youth joined the study on December 15th, the question would be prompted by the app in a manner that allows youth to report MVPA accumulation for December 14, 13, 12, 11, 10, 9, and 8. From these responses, average hours of MVPA on weekdays, weekends, and overall (weekday MVPA plus weekend MVPA) were derived.
2.3.2 SB (Outcome Variable)
SB was captured using a modified version of the SB Questionnaire (SBQ). The SBQ showed moderate to excellent test-retest reliability (ICC = 0.64–0.90 weekdays, 0.51–0.93 weekends) and low to moderate validity (ρ = 0.20–0.44, p < 0.05) for accelerometer-measured SB (Rosenberg et al. 2010). However, its validation has primarily been conducted in adults rather than youth, which may limit its applicability in this population. Youth were asked about the amount of time spent on various activities. For each activity, separate questions were asked about weekdays and weekends. These activities included time spent watching television, internet surfing, doing homework on a desktop, laptop, or tablet, playing video games, use of smartphone for internet surfing, playing video games using a smartphone, texting, sitting, reading paper-based books or magazines, sitting and listening to music, talking on the phone, doing artworks, doing crafts, sitting and playing musical instruments, and driving or riding in motorized transportation on both weekdays and weekends. Responses to these questions included: ‘none’, ‘15 min or less’, ‘30 min’, ‘1 h’, ‘2 h’, ‘3 h’, ‘4 h’, ‘5 h’, and ‘6 h or more’. From these responses, the average hours of SB on weekdays, weekends, and overall (weekday plus weekend) were derived.
Recreational screen time (ST) was derived from responses related to watching television, internet surfing, playing video games, and smartphone use for browsing, gaming, and texting, while other SB was derived from the remaining activities in this category.
2.3.3 Sleep (Outcome Variable)
Sleep was assessed using custom open-ended questions adapted from those used in previous studies to measure sleep duration (Mallinson et al. 2019). However, to the best of our knowledge, no validation studies have been conducted to assess the psychometric properties of these questionnaire items. Youth were asked: “On a typical weekday, how many hours do you spend on sleep at night” (Open-ended) and “On a typical weekend, how many hours do you spend on sleep at night” (Open-ended). From these responses, we derived the average hours of sleep at night on weekdays and weekends.
2.3.4 Weight Status (Independent Variable)
The BMI of youth was calculated from the information about their “Weight” and “Height” (weight in kilograms divided by height in metres squared). Afterwards, using the World Health Organization recommendation (Zaballa et al. 2012), youth were categorized into (1) healthy weight status, and (2) underweight, overweight, and/or obese weight status.
2.3.5 Cannabis Use (Independent Variable)
Cannabis use was captured by asking youth: “Did you use cannabis in the last 30 days” (Close-ended), with response options of “No, I did not use cannabis in the last 30 days” corresponding to “No” and “Yes, I used cannabis in the last 30 days” corresponding to “Yes”.
2.3.6 Mental Health (Independent Variable)
Self-reported depression was captured by asking youth “When was the last time you felt depressed?” (Close-ended), with the response options: “Past month”, “Never”, “Past 3 months”, “Past 6 months”, “Past year”, “Over a year ago”, and “I do not know”. The responses were categorized into (1) “Never” corresponding to “Never”; (2) “Past month” corresponding to “Past month” (3) “Past 3 months or more” corresponding to “Past 3 months”, “Past 6 months”, “Past year”, “Over a year ago”, and (4) “I don't know”. Self-reported mental health was captured by asking youth, “How would you rate your mental health” (Close-ended) with the response options: “Fair”, “Good”, “Very Good”, “Excellent”, “Poor”, and “None offered”. The responses “Fair”, “Good”, “Very Good”, and “Excellent”, were grouped as “Good”, while “Poor” was the second category, and “None offered” was the third category. Stress was captured by asking youth, “Are you stressed during most days?” (Close-ended), with response options: “Not at all stressful”, “Not very stressful”, “A bit stressful”, “Very stressful”, and “Extremely stressful”. The responses were dichotomized into “Yes” equivalent to “Not very stressful”, “A bit stressful”, “Very stressful”, “Extremely stressful”, and “No” equivalent to “Not at all stressful.”Anxiety was assessed using the Generalized Anxiety Disorder-2, which asked youth, “Over the last 2 weeks, how often have you felt nervous, anxious, or on edge?” and “How often have you been unable to stop or control worrying?” Responses ranged from 0 (“not at all”) to 3 (“nearly every day”), with a total score of 0–6. A score of ≥ 3 indicated “clinically significant anxiety symptoms”, while < 3 was considered “None”.
2.3.7 Sociodemographic Covariates
Sociodemographic information used in this study included gender, age, parental education, school, and ethnic background. Gender was captured by asking youth “What is your gender?” (Close-ended), with five response options: “male”, “female”, “transgender”, “other (please specify)”, and “prefer not to disclose”. To address the low counts within the categories, responses that were “transgender,” “other,” and “prefer not to disclose” were combined into a single category. Age was captured with the question “How old are you?” (Open-ended). Parental education was captured by asking them about the highest level of education of one of their parents or guardians through six response options: “elementary school”, “some secondary/high school”, “completed high school”, “some postsecondary (university/college)”, “received university or college degree/diploma”, and “does not apply”. Each of the six responses was organized into three categories of parental education: (1) “less or equal than secondary/high school” corresponds to “elementary school or below”, and “some secondary/high school”; (2) “Some postsecondary (university or college) or more” corresponds to “completed high school”, “some postsecondary (university/college)”, and “received university or college degree/diploma”, and (3) “does not apply”. Youth were also asked if they had a part-time job (Close-ended), with the following response options: “Yes” or “No”. Participants were required to indicate their school, which was recoded to schools 1, 2, 3, 4, and 5. The ethnicity of youth was captured through the following response options: “First Nations”, “Dene”, “Cree”, “Metis”, “Inuit”, “African”, “Asian”, “Canadian”, “Caribbean/West Indian”, “Eastern European”, “European”, “South Asian”, “Other”, and “Mixed”. The responses were grouped into two categories: (1) “Canadians”, which corresponds to “First Nations”, “Dene”, “Cree”, “Metis”, “Inuit”, “Canadian”, and (2) “Others”, which includes “African”, “Asian”, “Caribbean/West Indian”, “Eastern European”, “European”, “South Asian”, “Other” and “mixed”. School was controlled for using a categorical variable (1-5) representing the different schools that participated in the study.
2.4 Statistical Analysis
All statistical analyses were conducted using R 4.2.1, an open-source statistical software tool (R Core Team 2021). Independent variables included in this study were selected based on descriptive cross-tabulations and previous findings from peer-reviewed articles. Frequencies and percentages were used to describe the categorical variables, while mean and standard deviation were used to describe continuous variables used in this study. Descriptive statistics were stratified by cannabis use to better understand the nuances of movement behaviours in relation to cannabis use. Linear regression models were used to assess the association between 24-h movement behaviours (including MVPA, sleep, and SB) and cannabis use. SB was stratified into recreational ST and other SB to explore their distinct relationships with cannabis use. Given that multiple comparisons are being carried out in this study, the Benjamini-Hochberg (BH) procedure was applied to adjust p-values and control for false discovery rate (Chen et al. 2017). The sample size calculation determined that 77 participants would provide sufficient power (80%) to detect a moderate effect size of 0.176 (Cohen's f2) at a significance level of 0.05. All statistical analyses were considered significant at p < 0.05.
3 Results
A total of 208 participants were included in this study. Descriptive statistics of the independent variables are presented in Table 1. The result presents participant characteristics stratified by cannabis use (Using Cannabis: n = 33; Not Using Cannabis: n = 175). Cannabis users were slightly older (Mean = 16.10, SD = 1.40) than non-users (Mean = 15.58, SD = 1.27). Alcohol consumption showed a difference, with 27.27% of non-drinkers reporting cannabis use. In terms of weight status, cannabis users were less likely to have a healthy BMI (14.95%) compared to non-users (85.05%), with slightly higher rates among those classified as underweight, overweight, or obese (16.22% vs. 83.78%). Cannabis use was more common among participants with clinically significant anxiety (20.00%) compared to those without anxiety symptoms (14.79%). Similarly, cannabis use was higher among those reporting “Poor” mental health (21.43%) compared to those with better self-reported mental health (15.12%). Cannabis use was higher among males (15.39%) than females (14.41%) and among participants whose parents had lower education (24.44%) compared to those with postsecondary education (13.51%). Part-time employment (18.46%) and non-Canadian ethnicity (15.57%) were also associated with higher cannabis use. Lastly, school differences were evident, with the highest cannabis use in School 3 (75.00%) and the lowest in School 4 (8.16%).
| Cannabis use | |||
|---|---|---|---|
| Independent variables | Total | Using cannabis | Not using cannabis |
| Continuous Variable | |||
| Age: Mean [SD] | 15.57 [1.31] | 16.10 [1.40] | 15.58 [1.27] |
| Categorical Variable | |||
| Cannabis use | Frequency (Percentage)a | ||
| Using Cannabis | 33 (15.87) | N/A | N/A |
| Not using Cannabis | 175 (84.13) | N/A | N/A |
| Consumed alcohol at least once in their lifetime | |||
| No | 121 (58.17) | 33 (27.27) | 88 (72.72) |
| Yes | 87 (41.83) | — | 87 (100) |
| Weight Status: BMI | |||
| Healthy weight status | 107 (59.12) | 16 (14.95) | 91 (85.05) |
| Underweight, overweight, and/or obese weight status | 74 (40.88) | 12 (16.22) | 62 (83.78) |
| Depressed | |||
| Never | 24 (13.95) | 4 (16.67) | 20 83.33) |
| Past Month | 110 (63.95) | 23 (20.91) | 87 (79.09) |
| Past 3 months or more | 38 (22.09) | 4 (15.79) | 34 (84.21) |
| Anxiety Symptoms | |||
| None | 142 (70.30) | 21 (14.79) | 121 (85.21) |
| Clinically significant anxiety symptoms | 60 (29.70) | 12 (20) | 48 (80) |
| Self-Reported Mental Health | |||
| Fair/Good/Very Good/Excellent | 172 (86) | 26 (15.12) | 146 (84.88) |
| Poor | 28 (14) | 6 (21.43) | 22 (78.57) |
| Stressed during most days | |||
| No | 33 (15.94) | 8 (24.24) | 25 (75.76) |
| Yes | 174 (84.06) | 25 (14.37) | 149 (85.63) |
| Sociodemographic covariates | |||
| Gender | |||
| Female | 111 (54.95) | 16 (14.41) | 95 (85.59) |
| Male | 91 (45.05) | 14 (15.38) | 77 (84.61) |
| Parental education | |||
| Less or equal than secondary/high school | 45 (23.31) | 11 (24.44) | 34 (75.56) |
| Some postsecondary (university or college) or more | 148 (76.68) | 20 (13.51) | 128 (86.49) |
| Part time Job | |||
| No | 131 (66.83) | 18 (13.74) | 113 (86.26) |
| Yes | 65 (33.16) | 12 (18.46) | 53 (81.54) |
| Ethnicity | |||
| Canadian | 80 (39.60) | 11 (13.75) | 69 (86.25) |
| Others | 122 (60.40) | 19 (15.57) | 103 (84.43) |
| School | |||
| 1 | 51 (24.64) | 10 (19.61) | 41 (80.39) |
| 2 | 41 (19.81) | 4 (9.756) | 37 (90.244) |
| 3 | 8 (3.87) | 6 (75) | 2 (25) |
| 4 | 49 (23.67) | 4 (8.16) | 45 (91.83) |
| 5 | 58 (28.02) | 9 (15.52) | 49 (84.48) |
- a Some categories do not sum up to 208 due to incomplete information.
- N/A—Not Applicable.
The summary statistics of the outcome variables are presented in Table 2. Cannabis users reported lower MVPA across weekdays (0.97 vs. 1.30 h/day), weekends (0.43 vs. 0.52 h/day), and overall (1.00 vs. 1.30 h/day). SB was consistently higher among cannabis users, particularly on weekends (11.06 vs. 8.03 h/day), with an overall SB of 5.96 versus 4.41 h/day. Sleep duration was lower in cannabis users on weekdays (6.52 vs. 7.00 h/day), weekends (8.39 vs. 8.77 h/day), and overall (7.45 vs. 7.89 h/day). Recreational ST and other SB followed a similar pattern, with cannabis users spending more time in these activities across all timeframes.
| Outcome variables | Measurement category | Cannabis use | |
|---|---|---|---|
| Using cannabis | |||
| Mean (SD) hours/day | Not using cannabis | ||
| MVPA | Weekday | 0.97 (0.42) | 1.30 (0.80) |
| Weekend | 0.43 (0.28) | 0.52 (0.40) | |
| Overall | 1.00 (0.45) | 1.30 (0.77) | |
| SB | Weekday | 3.92 (2.47) | 2.96 (1.72) |
| Weekend | 11.06 (6.52) | 8.03 (4.10) | |
| Overall | 5.96 (3.42) | 4.41 (2.25) | |
| Sleep | Weekday | 6.52 (1.31) | 7.00 (1.24) |
| Weekend | 8.39 (2.41) | 8.77 (2.01) | |
| Overall | 7.46 (2.76) | 7.89 (2.61) | |
| Recreational ST | Weekday | 2.24 (1.23) | 1.83 (1.03) |
| Weekend | 5.60 (3.60) | 4.18 (2.51) | |
| Overall | 3.20 (1.73) | 2.50 (1.30) | |
| Other SB | Weekday | 1.69 (1.56) | 1.13 (1.12) |
| Weekend | 5.46 (3.47) | 3.85 (2.35) | |
| Overall | 2.76 (1.94) | 1.91 (1.41) | |
The regression models (1–3) showing the associations between MVPA (hours/day) and cannabis use are presented in Table 3. Youth who reported healthy weight status also reported higher overall (β = 1.93, 95% [CI] = 0.21, 3.65, p-value = 0.031) and weekday (β = 1.54, 95% [CI] = 0.25, 2.82, p-value = 0.021) MVPA. Additionally, youth who had a part-time job reported higher overall (β = 2.52, 95% [CI] = 0.64, 4.40, p-value = 0.010) and weekend (β = 2.36, 95% [CI] = 0.96, 3.77, p-value = 0.002) MVPA in comparison to youth who had no part-time job.
| Variable | Hours/day MVPA Overall (Model 1)a | Hours/day MVPA Weekday (Model 2)a | Hours/day MVPA Weekend (Model 3)a |
|---|---|---|---|
| Cannabis use: Not Using Cannabis (Ref) | Ref | Ref | Ref |
| Cannabis use: Using Cannabis | −1.39 (−3.71, 0.93) | −1.57 (−3.31, 0.16) | 0.183 (−0.74, 1.11) |
| SRMH: Excellent (Ref) | Ref | Ref | Ref |
| SRMH: Poor | −0.23 (−2.67, 2.22) | −0.350 (−2.18, 1.48) | 0.123 (−0.85, 1.10) |
| Weight status: Underweight, overweight, and/or obese (Ref) | Ref | Ref | Ref |
| Weight status: Healthy weight | 1.93* (0.21, 3.64)κ | 1.53* (0.25, 2.82)κ | 0.389 (−0.30, 1.08) |
| Part time job: No (Ref) | Ref | Ref | Ref |
| Part time job: Yes | 2.52* (0.64, 4.40)κ | 2.36* (0.96, 3.77)κ | 0.15 (−0.60, 0.91) |
| Last time depressed: Never (Ref) | Ref | Ref | Ref |
| Last time depressed: Last Month | 1.51 (−1.48, 4.49) | 1.17 (−1.06, 3.40) | 0.34 (−0.85, 1.53) |
| Last time depressed: Past 3 months or more | 0.95 (−1.95, 3.85) | 0.64 (−1.53, 2.80) | 0.32 (−0.84, 1.47) |
| Consumed alcohol at least once in their lifetime: Yes (Ref) | Ref | Ref | Ref |
| Consumed alcohol at least once in their lifetime: No | −0.98 (−2.95, 0.99) | −0.45 (−1.93, 1.02) | −0.53 (−1.31, 0.26) |
| Stressed during most days: No (Ref) | Ref | Ref | Ref |
| Stressed during most days: Yes | −1.40 (−4.08, 1.27) | −1.30 (−3.30, 0.70) | −0.10 (−1.17, 0.97) |
| Anxiety symptoms: None (Ref) | Ref | Ref | Ref |
| Anxiety symptoms: Clinically significant | 0.65 (−1.44, 2.73) | 0.77 (−0.79, 2.33) | −0.13 (−0.96, 0.71) |
| Constant | 14.06 (−0.50, 28.61) | 10.40 (−0.48, 21.29) | 3.65 (−2.16, 9.47) |
| Observations | 131 | 131 | 131 |
- * p < 0.05.
- a These models controlled for gender, age, parental education, school, and ethnic background.
- κ p-values significant after adjusting for the BH correction.
The regression models showing the associations between SB (hours/day) and cannabis use are presented in Table 4. Youth who reported cannabis use also reported significantly higher overall (β = 8.92, 95% [CI] = 1.11, 16.72, p-value = 0.028) and weekends (β = 5.32, 95% [CI] = 0.89, 9.75, p-value = 0.021) SB in comparison to youth who did not report cannabis use. Moreover, youth who reported being depressed in the past 3 months or more reported more hours of SB on weekdays (β = 5.44, 95% [CI] = 0.44, 10.44, p-value = 0.036) in comparison to youth who had never experienced depression. However, the association was not significant after the BH correction.
| Variables | Hours/day SB Overall (Model 1)a | Hours/day SB weekday (Model 2)a | Hours/day SB weekend (Model 3)a |
|---|---|---|---|
| Cannabis use: Not Using Cannabis (Ref) | Ref | Ref | Ref |
| Cannabis use: Using Cannabis | 8.92* (1.11, 16.72)κ | 3.59 (-0.41, 7.60) | 5.32* (0.89, 9.75)κ |
| SRMH: Excellent (Ref) | Ref | Ref | Ref |
| SRMH: Poor | 3.54 (−3.98, 11.05) | 1.24 (−2.62, 5.09) | 2.30 (−1.97, 6.56) |
| Weight status: Underweight, overweight, and/or obese (Ref) | Ref | Ref | Ref |
| Weight status: Healthy weight | −0.17 (−5.91, 5.58) | −0.18 (−3.13, 2.77) | 0.02 (−3.25, 3.28) |
| Part time job: No (Ref) | Ref | Ref | Ref |
| Part time job: Yes | −6.04 (−12.37, 0.29) | −2.65 (−5.89, 0.60) | −3.39 (−6.99, 0.20) |
| Last time depressed: Never (Ref) | Ref | Ref | Ref |
| Last time depressed: Past month | 7.45 (−2.50, 17.40) | 3.58 (−1.52, 8.68) | 3.87 (−1.78, 9.52) |
| Last time depressed: Past 3 months or more | 8.79 (−0.96, 18.53) | 5.44* (0.44, 10.44) | 3.35 (−2.18, 8.88) |
| Consumed alcohol at least once in their lifetime: Yes (Ref) | Ref | Ref | Ref |
| Consumed alcohol at least once in their lifetime: No | 1.59 (−5.03, 8.21) | 0.90 (−2.50, 4.30) | 0.69 (−3.07, 4.45) |
| Stressed during most days: No (Ref) | Ref | Ref | Ref |
| Stressed during most days: Yes | 0.56 (−8.39, 9.52) | 0.08 (−4.52, 4.67) | 0.49 (−4.60, 5.57) |
| Constant | 15.51 (−33.44, 64.46) | 7.67 (−17.44, 32.78) | 7.84 (−19.96, 35.63) |
| Observations | 132 | 132 | 132 |
- * p < 0.05.
- a These models controlled for gender, age, parental education, school, and ethnic background.
- κ p-values significant after adjusting for the BH correction.
The regression models showing the associations between recreational ST (hours/day) and cannabis use are presented in Table 5. Cannabis users reported significantly higher overall recreational ST compared to non-users (β = 4.66, 95% [CI] = 0.19, 9.13, p-value = 0.044) and on weekends (β = 2.70, 95% [CI] = 0.08, 5.32, p-value = 0.046). Youth with a part-time job had significantly lower overall recreational ST (β = -3.89, 95% [CI]= -7.51, -0.26, p-value = 0.038). These variables were not significant after the BH correction.
| Hours/day recreational ST overall (Model 1)a | Hours/day recreational ST weekday (Model 2)a | Hours/day recreational ST weekend (Model 3)a | |
|---|---|---|---|
| Cannabis use: Not Using Cannabis (Ref) | Ref | Ref | Ref |
| Cannabis use: Using Cannabis | 4.66* (0.19, 9.13) | 1.96 (−0.48, 4.40) | 2.70* (0.08, 5.32) |
| SRMH: Excellent (Ref) | Ref | Ref | Ref |
| SRMH: Poor | 0.62 (−3.69, 4.92) | 0.09 (−2.27, 2.44) | 0.53 (−1.99, 3.05) |
| Weight status: Underweight, overweight, and/or obese (Ref) | Ref | Ref | Ref |
| Weight status: Healthy | −0.75 (−4.04, 2.54) | −0.07 (−1.87, 1.73) | −0.68 (−2.60, 1.25) |
| Part time job: No (Ref) | Ref | Ref | Ref |
| Part time job: Yes | −3.89* (−7.51, -0.26) | −1.85 (−3.83, 0.13) | −2.04 (−4.16, 0.08) |
| Last time depressed: Never (Ref) | Ref | Ref | Ref |
| Last time depressed: Past month | 1.09 (−4.62, 6.79) | −0.03 (−3.15, 3.08) | 1.12 (−2.22, 4.45) |
| Last time depressed: Past 3 months or more | 2.27 (−3.32, 7.85) | 1.49 (−1.56, 4.54) | 0.78 (−2.49, 4.04) |
| Consumed alcohol at least once in their lifetime: Yes (Ref) | Ref | Ref | Ref |
| Consumed alcohol at least once in their lifetime: No | 0.40 (−3.40, 4.19) | 0.04 (−2.03, 2.12) | 0.35 (−1.87, 2.57) |
| Stressed during most days: No (Ref) | Ref | Ref | Ref |
| Stressed during most days: Yes | −0.13 (−5.26, 5.01) | −0.31 (−3.12, 2.49) | 0.19 (−2.81, 3.19) |
| Constant | −9.07 (−37.12, 18.98) | −3.25 (−18.58, 12.07) | −5.82 (−22.23, 10.59) |
| Observations | 132 | 132 | 132 |
- * p < 0.05.
- a These models controlled for gender, age, parental education, school, and ethnic background.
In the other SB (hours/day) models (Table 6), youth who use Cannabis exhibited significantly higher other SB on weekends compared to non-users (β = 2.62, 95% [CI] = 0.11, 5.13, p-value = 0.043). Youth who reported feeling depressed in the past month had significantly higher overall other SB (β = 6.36, 95% [CI] = 0.39, 12.33, p-value = 0.039), as well as increased SB on weekdays (β = 3.61, 95% [CI] = 0.18, 7.04, p-value = 0.042). These were not significant after applying the BH correction. Those who reported depression in the past 3 months or more showed higher overall SB (β = 6.52, 95% [CI] = 0.67, 12.37, p-value = 0.031) and weekday SB (β = 3.95, 95% [CI] = 0.59, 7.30, p-value = 0.023).
| Hours/day other SB overall (Model 1)a | Hours/day other SB weekday (Model 2)a | Hours/day other SB weekend (Model 3)a | |
|---|---|---|---|
| Cannabis use: Not Using Cannabis (Ref) | Ref | Ref | Ref |
| Cannabis use: Using Cannabis | 4.26 (−0.43, 8.94) | 1.63 (−1.06, 4.32) | 2.62* (0.12, 5.13) |
| SRMH: Excellent (Ref) | Ref | Ref | Ref |
| SRMH: Poor | 2.92 (−1.59, 7.43) | 1.15 (−1.44, 3.74) | 1.77 (−0.65, 4.18) |
| Weight status: Underweight, overweight, and/or obese (Ref) | Ref | Ref | Ref |
| Weight status: Healthy | 0.58 (−2.86, 4.03) | −0.11 (−2.09, 1.87) | 0.69 (−1.15, 2.54) |
| Part time job: No (Ref) | Ref | Ref | Ref |
| Part time job: Yes | −2.15 (−5.95, 1.65) | −0.80 (−2.98, 1.38) | −1.35 (−3.39, 0.68) |
| Last time depressed: Never (Ref) | Ref | Ref | Ref |
| Last time depressed: Past month | 6.36* (0.39, 12.33) | 3.61* (0.18, 7.04) | 2.75 (−0.44, 5.95) |
| Last time depressed: Past 3 months or more | 6.52* (0.67, 12.37)κ | 3.95* (0.59, 7.30)κ | 2.57 (−0.56, 5.70) |
| Consumed alcohol at least once in their lifetime: Yes (Ref) | Ref | Ref | Ref |
| Consumed alcohol at least once in their lifetime: No | 1.19 (−2.78, 5.17) | 0.86 (−1.42, 3.14) | 0.34 (−1.79, 2.46) |
| Stressed during most days: No (Ref) | Ref | Ref | Ref |
| Stressed during most days: Yes | 0.69 (−4.69, 6.06) | 0.39 (−2.69, 3.47) | 0.30 (−2.58, 3.17) |
| Constant | 24.58 (−4.80, 53.96) | 10.93 (−5.93, 27.78) | 13.66 (−2.07, 29.37) |
| Observations | 132 | 132 | 132 |
- * p < 0.05.
- a These models controlled for gender, age, parental education, school, and ethnic background.
- κ p-values significant after adjusting for the BH correction.
In the sleep (hours/day) model (Table 7), youth who reported experiencing stress during most days were found to be associated with less overall (β = −2.04, 95% [CI] = −3.50, −0.58, p-value = 0.008) and weekend (β = −1.36, 95% [CI] = −2.47, −0.24, p-value = 0.019) sleep in comparison to youth who did not report experiencing stress during most days. Moreover, youth who reported healthy weight status also reported higher overall (β = 1.31, 95% [CI] = 0.37, 2.244, p-value = 0.008) and weekend (β = 0.93, 95% [CI] = 0.21, 1.64, p-value = 0.013) sleep compared to youth who were either underweight, overweight, or obese.
| Hours/day Sleep Overall (Model 1) a | Hours/day Sleep Weekday (Model 2) a | Hours/day Sleep Weekend (Model 3) a | |
|---|---|---|---|
| Cannabis use: Not Using Cannabis (Ref) | Ref | Ref | Ref |
| Cannabis use: Using Cannabis | −0.64 (−1.91, 0.63) | −0.24 (−0.87, 0.39) | −0.40 (−1.37, 0.57) |
| SRMH: Excellent (Ref) | Ref | Ref | Ref |
| SRMH: Poor | −0.96 (−2.18, 0.27) | −0.33 (−0.93, 0.28) | −0.63 (−1.57, 0.31) |
| Weight status: Underweight, overweight, and/or obese (Ref) | Ref | Ref | Ref |
| Weight status: Healthy | 1.31* (0.37, 2.24)b | 0.38 (−0.08, 0.85) | 0.93* (0.21, 1.64)b |
| Part time job: No (Ref) | Ref | Ref | Ref |
| Part time job: Yes | 0.02 (−1.01, 1.05) | 0.25 (−0.26, 0.77) | −0.24 (−1.02, 0.55) |
| Last time depressed: Never (Ref) | Ref | Ref | Ref |
| Last time depressed: Past month | −0.03 (−1.65, 1.59) | −0.67 (−1.48, 0.14) | 0.64 (−0.60, 1.88) |
| Last time depressed: Past 3 months or more | 0.25 (−1.34, 1.84) | −0.47 (−1.26, 0.32) | 0.72 (−0.50, 1.93) |
| Consumed alcohol at least once in their lifetime: Yes (Ref) | Ref | Ref | Ref |
| Consumed alcohol at least once in their lifetime: No | 0.19 (−0.89, 1.26) | 0.13 (−0.41, 0.66) | 0.06 (−0.76, 0.89) |
| Stressed during most days: No (Ref) | Ref | Ref | Ref |
| Stressed during most days: Yes | −2.04* (−3.50, -0.58)b | −0.69 (−1.41, 0.04) | −1.36* (−2.47, −0.24)b |
| Constant | 16.93* (8.95, 24.90)b | 9.74* (5.78, 13.70)b | 7.19* (1.09, 13.28)b |
| Observations | 132 | 132 | 132 |
- * p < 0.05.
- a These models controlled for gender, age, parental education, school, and ethnic background.
- b p-values significant after adjusting for the BH correction.
4 Discussion
This study uses data from a digital epidemiological and citizen science platform that engaged youth as citizen scientists via their own smartphones for a period of 8 days (Brodersen et al. 2023a). As there has been a call for conducting more holistic research on the combination of movement behaviours (Tremblay et al. 2016), the objective of this study was to utilize a digital citizen science approach to examine if recreational cannabis use was associated with the 24-h movement behaviours (i.e., physical activity, SB, and sleep) among youth aged 13 to 21 years. The study also aimed to examine the sociodemographic and contextual factors that are associated with 24-h movement behaviours.
Given that MVPA is a key protective factor for non-communicable diseases (Lee et al. 2012; Biswas et al. 2022; Santos et al. 2023; Warburton 2006), one of our aims was to explore whether cannabis use was associated with MVPA among youth. However, we did not find an association between cannabis use and MVPA. This contrasts with previous studies, such as Ashdown-Franks et al. (2019), which found that cannabis use was associated with lower physical activity levels among adolescents from 21 low- and middle-income countries around the world (Ashdown-Franks et al. 2019). The lack of a significant association in our study could be due to differences in study design, population characteristics, or contextual factors. For instance, unlike many other countries, cannabis is legal across all Canadian provinces, yet despite restrictions on sales to those under 18, youth appear to have easy access to it (Nguyen and Mital 2022; Wadsworth et al. 2022). Additionally, our study focused specifically on Canadian youth, whereas other studies have examined youth in different geographical and socioeconomic settings, such as low- and middle-income countries (Ashdown-Franks et al. 2019).
In addition to cannabis use, this study found nuanced individual differences, including weight status and employment status, that were associated with MVPA. These findings align with a previous study, which found that youth with overweight or obese weight status had lower levels of MVPA compared to the entire sample (Carson et al. 2016). Moreover, our study found that during weekdays, youth with a healthy weight status reported higher levels of MVPA compared to those who reported being underweight, overweight, or obese. This finding was not significant during weekends, perhaps due to the large proportion of MVPA that occurs through physical activity incorporated into daily school routines on weekdays (Aubert et al. 2022; Brazendale et al. 2021). However, as youth's weight status plays a role in their participation in physical activity during school (Pope et al. 2020), youth who are underweight, overweight, and/or obese may not engage in school-based physical activity as much as their counterparts who have a healthy weight status. Schools must design structured and customized physical activity sessions in a way that includes all youth, regardless of their weight.
The association between working a part-time job and MVPA was also examined in this study. In particular, our study found that youth who reported working a part-time job reported higher levels of MVPA than youth who did not have a part-time job; however, this association was only significant in the overall and weekday models. Similarly, a study previously found that working part-time was associated with higher physical activity levels among male high school students (Van Domelen 2015). As youth working part-time jobs on weekdays may also be engaging in structured physical activity during school (Aubert et al. 2022; Brazendale et al. 2021), the combined effect of both forms of physical activity could be a potential contributor to the observed increase in MVPA. Future research should explore the mechanisms that contribute to the specific variations in MVPA during weekdays and weekends for youth working part-time jobs.
This study also examined the relationship between cannabis use and SB. Our study's results indicate that youth who reported using cannabis also reported higher levels of SB compared to youth who did not use cannabis. This finding aligns with previous studies, which also found cannabis use to be associated with higher odds of SB in adolescence (Vancampfort et al. 2019b; de la Haye et al. 2014). This may be attributable to youth perceiving cannabis use as a potential tool to manage stress and anxiety (Porath-Waller et al. 2013); thus, when using cannabis, youth may engage in indoor activities that are not as physically demanding, such as watching television or playing video-games. Given that SB is associated with a range of negative health outcomes among youth, including reduced physical and psychosocial health (Tremblay et al. 2011; LeBlanc et al. 2015), it is imperative for policymakers to not only enhance education and awareness regarding the potential risks of cannabis use on SB but also the importance of promoting alternative strategies for managing stress and anxiety – potential motivators for cannabis use among youth.
Our study also revealed nuanced variations in SB. For instance, during weekends but not weekdays, youth who reported using cannabis also reported higher levels of SB than their counterparts not using cannabis. These findings could be due to youth having fewer school obligations during weekends when they are not attending school. Additionally, our study found that youth who reported being depressed in the past 3 months or more had higher SB on weekdays compared to individuals who were not previously depressed. This finding may be attributable to recreational ST, a key component of SB, serving as a means of coping with mechanism for psychological distress (Kim et al. 2015), which tends to be more prevalent among youth on weekdays compared to weekends (Reardon et al. 2023). To better understand recreational ST, our study stratified overall SB into recreational ST and other SB and conducted separate analyses. Similar to our findings with overall SB, cannabis use was associated with higher recreational ST and other SB on weekends but not weekdays, reinforcing that the relationship between cannabis use and SB may be more pronounced on weekends. However, these associations were not significant after adjusting for false discovery rate, suggesting that they may be due to multiple hypothesis testing and should be interpreted with caution. Future studies should conduct focused analyses on weekday-weekend differences to better capture these nuances while minimizing the risk of false discoveries associated with multiple comparisons. There is also a need for studies to take into consideration not only the different types of ST behaviours, but specifically smartphone use due to it's implication on their mental and physical health (Katapally, Thorisdottir, et al. 2018; Brodersen et al. 2022; Brodersen et al. 2023b).
Another objective of this study was to assess sleep behaviours in youth given the increasing prevalence of sleep-related issues among youth (Madan Jha 2023). Sleep is important for maintaining optimal physical health, cognitive function, and mental health (Chaput et al. 2016), particularly among youth who are in a critical developmental period (Larsen and Luna 2018). The study found that cannabis use was not associated with hours of sleep among youth, which aligns with previous research, which also found that cannabis neither harms nor benefits sleep among adolescents over 1 year (Goodhines et al. 2022). However, other studies have found cannabis use to be associated with lower hours of sleep among youth (Madan Jha 2023; Chaput et al. 2016; Larsen and Luna 2018; Goodhines et al. 2022). This discrepancy highlights the complexity of the relationship between cannabis use and sleep among youth as sleep is likely influenced by other contextual factors. For instance, this study found that stress was associated with fewer hours of sleep among youth on weekends but not on weekdays. This finding may be explained by previous evidence indicating that adolescents use technology at bedtime more on weekends than weekdays, which may be contributing to the association between sleep levels and mental health (Reardon et al. 2023). It is important for future research to explore the mechanisms through which these and other contextual factors influence sleep to better promote youth well-being.
4.1 Strengths and Limitations
This study's primary strength is its examination of the associations between cannabis use and movement behaviours (i.e., sleep, MVPA, and SB) from a citizen scientist perspective, using citizen-owned devices (Katapally 2022; Hammami and Katapally 2022). This approach enhances ecological validity, though a key limitation is the reliance on self-reported data, which may introduce recall biases in reporting movement behaviours. Moreover, some measures such as the SBQ have been primarily validated in adults rather than youth (Rosenberg et al. 2010), while others such as the sleep questions lack established psychometric properties altogether (Mallinson et al. 2019). Nevertheless, self-reported use of cannabis is relatively accurate (79.9% sensitivity and 80.0% specificity) (Zielinski et al. 2017), and the anonymous smartphone engagement through our digital citizen science approach may have minimized social desirability biases. The crude nature of the measurement tools for activity behaviours in this study limits the generalizability of our findings. Future research should use objective measures, such as accelerometers for MVPA and sleep trackers for sleep quality, to improve accuracy (Katapally and Chu 2019; Katapally et al. 2016). Researchers should also prioritize validating these measures in youth populations to enhance their reliability and applicability.
Selection bias is another limitation, as participants in citizen science studies may differ in technology access and digital literacy (Buchan et al. 2024). There is a need to explore how these factors influence participation and address barriers for underrepresented groups. Additionally, while other behaviours or environmental factors may further explain variance in the outcomes, we chose to limit the number of predictors to avoid overfitting (López et al. 2022). Another limitation of this study is that it involved a cross-sectional design, which limits the understanding of the directionality of the association between cannabis use and 24-h movement behaviours. Longitudinal cohort studies are needed to assess causal pathways between cannabis use and 24-h movement behaviours (Solvang and Subbey 2019), while taking into consideration seasonality effects (Muhajarine et al. 2015, Katapally et al. 2015, Katapally et al. 2016).
5 Conclusion
This is the first study to examine the impact of cannabis use on the 24-h movement behaviours of youth. The results of the study indicated that self-reported cannabis use was associated with higher levels of SB, particularly recreational ST, but not MVPA and sleep. As youth are in a critical period of development with movement behaviours tracking into adulthood, these study findings indicate the need for policymakers, health professionals, and parents to consider the potential long-term implications of cannabis use on youth health.
Author Contributions
This study was conceptualized by TRK. TRK led project administration, data collection, survey design, and implementation. Funding was acquired by TRK. SI and JP led data analysis, and findings were interpreted by TRK. SI and JP prepared the first manuscript draft with support from TRK. The final manuscript was reviewed by all authors. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
We acknowledge the youth and educator citizen scientists who were critical to the implementation of the Smart Youth study. We acknowledge the support of Regina Public and Catholic schools in implementing the Smart Youth study. This study was funded by the Saskatchewan Health Research Foundation's Establishment Grant (#3779). This funding body had no role in the design of the study, the collection, analysis, and interpretation of data, and in writing the manuscript. The study is also supported by the Canada Research Chairs Program, which supports Dr. Tarun Katapally's research program.
Ethical Statement
Ethics approval was obtained from the universities of Regina and Saskatchewan through a synchronized review protocol (EB # 2017-29).
Conflicts of Interest
We have no conflicts of interest to declare.
Open Research
Data Availability Statement
The data that support the findings of this study are openly available in Figshare at Smart Youth Cannabis-24-h Movement Data: https://doi.org/10.6084/m9.figshare.25033673.v1.




