Ultrasound-guided peripheral trunk block technique: A new approach gradually stepping onto the stage of clinical anesthesia
Abstract
In recent years, with the continuous development and validation of new visualization, the ultrasound-guided peripheral trunk block becomes more mature and has a more extensive and broader implementation scope in clinical anesthesia. Based on this, we reviewed and summarized the literature on peripheral trunk nerve block include: paraspinal block, retrolaminar block, plane block of erect spinal muscle, transverse convex to pleural midpoint block, block of the trapezius muscle and anterior serratus muscle, anterior serratus muscle block, thoracic nerve block, abdominal transverse fascia block, type-I block of quadratus lumborum, type-II block of quadratus lumborum, type-III block of quadratus lumborum, block of the sheath of rectus abdominis. This paper reviews the ultrasound-guided peripheral trunk block technique, including development history, anatomic basis, implementation methods, advantages and disadvantages of nerve block technique, and describes the bottleneck and difficulties of nerve block technique at present.
Introduction
Nerve block technique in modern anesthesiology history can be traced back to Vienna more than 130 years ago, later than the ether anesthesia used in 1846. Karl Kohler, an ophthalmologist, discovered the anesthetic properties of cocaine, prepared it as a local anesthetic and used it as a topical anesthetic in ophthalmology (Goerig, 2015). In recent decades, nerve block technique has been developed, mainly due to ultrasound in clinical anesthesia. Because ultrasound has the advantage of visualization and can significantly improve the safety and effectiveness of nerve block, it has become the optimal peripheral nerve block choice.
Peripheral nerve block has the potential benefit of reducing acute pain and mortality, pulmonary complications, and hospital stay after perioperative implementation (Memtsoudis, et al., 2013; Perlas, et al., 2016). Its application scope extends from the initial regional block of the nerve trunk to the trunk region and gradually derives the concept of interfascial plane blocks. With the help of ultrasound guidance, local anesthetic drugs are injected into the nerve surroundings or the nerve's interfacial plane and produce an anesthetic effect via permeation into the adjacent nerves. One of the outstanding advantages is that the postoperative analgesia of thoracic and abdominal trunk surgery except upper and lower extremities can utilize nerve block.
It is undeniable that this new anesthesia method updates clinical anesthesia management and acute postoperative pain. First of all, ultrasound-guided nerve block solves the scope of the block that cannot be completed in the past, such as providing a variety of analgesic options for thoracic and abdominal surgery in addition to intravenous analgesia and intraspinal anesthesia. Secondly, because peripheral nerve block changes the local anesthetic injection site, making it possible to observe the drug “permeation path” in a visual state, the probability of vascular injury and the side effects of local anesthetics are significantly reduced. Although there is no direct evidence that ultrasound-guided nerve block can effectively reduce nerve injury(Barrington, et al., 2018), the current development trend of technique makes the injection site of local anesthesia farther away from the main body of the nerve trunk, in order to reduce the possibility of puncture adverse events and nerve injury(Palhais, et al., 2016). Thirdly, with the continuous development of nerve block, the inherent concept that opioids are necessary for postoperative analgesia has been gradually broken, and “de-opioid” postoperative analgesia can also achieve satisfactory results (Frauenknecht, et al., 2019), which makes the multi-mode analgesia with the involvement of nerve block become a leading role of contemporary clinical anesthesia management (Brown, et al., 2018; Richebe, et al., 2018).
With the continuous development and validation of new visualization, the ultrasound-guided peripheral trunk block becomes more mature and has a more extensive and broader implementation scope in clinical anesthesia. Based on this, we reviewed and summarized the literature on peripheral trunk nerve block from the aspects of its development history, anatomical basis, implementation methods, technical advantages, and disadvantages.
Part I: Anatomical basis and technical classification of trunk nerve block
With the popularization and application of ultrasound in clinical anesthesia, the anatomical knowledge needed for regional block anesthesia extends from related structures such as spinal canal and nerve trunk to paravertebral structure, thoracic and abdominal wall muscle, muscle fascia plane. The traditional nerve block relies on the body surface localization and the “sense of breakthrough” when the puncture needle breaks through the target structure. This unsafe process limits the application of nerve block in trunk analgesia. With the maturity of visualization, the theoretical knowledge of anesthesiologists has been effectively released. Modern trunk nerve block no longer emphasizes the injection of local anesthetics around the nerve trunk; instead, any anatomical interval and any muscle fascia plane may be an effective block site in the clinic, which however is often difficult to be completed by anatomical positioning and “sense of breakthrough”.
Paravertebral block
A brief introduction to PVB
PVB is characterized as injecting local anesthetics into space on both sides of the spine. Hugo Sellheim, a professor of obstetrics and gynecology at the Leipzig University in Germany in 1905, was first described this method and was used for analgesia in abdominal surgery (Župčić, 2019). After entering the 21st century, with the ultrasound development, this “ancient” technique has regained its rebirth and has a significant trend to replace epidural analgesia, especially in thoracic postoperative analgesia.Paravertebral space (PVS) is a wedge-shaped region bounded by the vertebral body, intervertebral disc, and intervertebral foramen. The pleural parietal layer in front and the superior transverse costal ligament, ribs, and transverse process behind it (Costache, et al., 2018). In this space, there are essential structures such as the intercostal branch, dorsal branch, communicating branch, and sympathetic chain of the spinal nerve, so anesthetics injection in PVS can have a similar effect to the unilateral epidural block (Figure 1). Block can be carried out in cervical vertebrae, thoracic vertebrae, and lumbar vertebrae, respectively, to provide analgesia for upper limb, breast, abdominal and lower limb surgery (Akinci, et al., 2019) (Pelaez, et al., 2010) (Xie, et al., 2019).
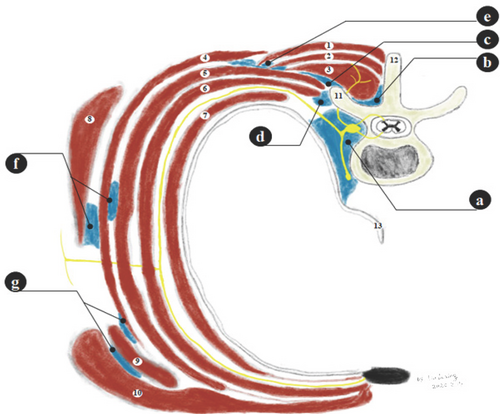
Thoracic nerve block. (1) Trapezius muscle; (2) Rhomboid muscle; (3) Erect spinal muscle; (4) Anterior serratus muscle; (5) External intercostal muscle; (6) Intercostal medial muscle; (7) Intercostal outermost muscle; (8) Latissimus dorsi; (9) Pectoralis minor; (10) Pectoralis major; (11) Transverse protuberance; (12) Spinous process; (13) Pleura. (a) Paraspinal block; (b) Retrolaminar block; (c) Plane block of erect spinal muscle; (d) Transverse convex to pleural midpoint block; (e) Block of trapezius muscle and anterior serratus muscle; (f) Anterior serratus muscle block; (g) Thoracic nerve block
Implementation methods of PVB
The classic PVB based on body surface localization is to insert the needle vertically at 2.5 cm beside the spinous process, and when in contact with the transverse process, the needle passes out from above or under the bone until negative pressure on the syringe with fluid is observed (MJ.,R, 1979). The process of PVB changes after introducing ultrasound. The “visual state” of ultrasound facilitates clarifying the anatomy of PVS and completing the operation by injecting anesthetic after the needle tip reaches PVS to avoid essential structures injury such as pleura during puncture.
It is worth mentioning that, due to the ample operating space in this area, there are no special requirements for patient’s posture, who can be placed in sitting position, prone position, lateral recumbent position, or even standing position to complete the operation. Ultrasonic probe (with a high-frequency linear array or low-frequency convex array) according to the equipment conditions. The probe can also be placed according to the operator’s experience or habit; either the long axis (sagittal position) or the short axis (transverse position) of the spine is appropriate. Clinical practice has proved that the selection of in-plane or out-of-plane needles can be completed under the condition of all kinds of probe placement.
Drug injection of PVB can use single point or multi-segment, unilateral or bilateral, or catheterization after puncture for long-term administration. The required concentration and volume of local anesthesia should be individualized according to the needs of surgical analgesia. However, the literature shows that the analgesic range of single-point injection of 0.5% ropivacaine is the same as that of 5 multi-segmental injection of ropivacaine of the same concentration volume (Uppal, et al., 2017), which is related to the effective diffusion of anesthetics in the cranial-caudal side of PVS, suggesting that single-point block is well qualified in operations without the need for large-scale analgesia and can decrease the probability of complications due to multiple punctures.
Technical advantages and disadvantages of PVB
PVB is expected to replace intraspinal anesthesia. Especially in the thoracic puncture, it is significantly easier than an epidural puncture. Because of the unilateral block's targeted completion, PVB can effectively reduce the incidence of perioperative hypotension and postoperative pulmonary complications compared with epidural analgesia and significantly reduce the occurrence of mild adverse events thoracic block (Yeung, et al., 2016).
However, PVB shows no breakthrough advantages than traditional epidural analgesia (El Shora, et al., 2018). PVB also has the possibility of serious complications such as pneumothorax, which limits its clinical application. Although PVB has been improved after introducing ultrasound, based on which most scholars speculate that serious complications will be reduced to some extent, the literature evidence shows that the improvement of ultrasound on PVB is below expectation. Ultrasound may reduce the occurrence of complications only in the short-axis plane puncture (Pace, et al., 2016). Therefore, it is still necessary to explore new puncture block sites to optimize the shortcomings of PVB.
Retrolaminar block
A brief introduction to RLB
As a new puncture technique for improving PVB, A brief introduction to RLB was first reported by Pfeiffer in 2006 (Pfeiffer, et al., 2006), and the related ultrasound-guided technique was developed several years later in 2013 (Voscopoulos, et al., 2013).
RLB is located on the surface of each vertebral lamina. Unlike the interspace injection of PVB, the target area of RLB is the bony structure (Figure 1). The purpose of the improvement is to reduce the puncture depth of PVB and prevent the needle tip from crossing the transverse process to avoid nerve root injury and pneumothorax at the physical level. RLB and PVB share the same indication in theory, but there are no sufficient randomized controlled studies. The only reports describe the application of RLB in postoperative analgesia in thoracic and lumbar surgery (Murouchi, et al., 2016; Onishi, et al., 2018; Onishi, et al., 2019).
The implementation method of RLB
Based on the improvement of PVB, the classic RLB based on body surface localization is to insert the needle vertically at 1.5 cm beside the spinous process, and when in contact with the lamina, the needle tip is withdrawn appropriately, and the injection is completed (Pfeiffer et al., 2006). Implementing the body surface localization method is relatively simple, but it is not clear whether the needle tip is located in the lamina or transverse process. Under the development of ultrasonic visualization, the needle can be injected into the spinal long-axis plane. After the relationship between the tip and the lamina is clearly observed, the puncture needle arrives at the lamina's bony components, and the local anesthetic is injected into the surface of the lamina. The operation is completed after a slight withdrawal of the needle.
Very similar to PVB, the implementation of RLB has no special requirements for the patient’s posture except for the supine position. Because the puncture depth of RLB is shallower than that of PVB, the high-frequency linear array probe can be selected to obtain more explicit ultrasound images. Each probe placement method can complete the in-plane puncture technique on both the spinal long and short axis, but among the limited foreign reports, inserting the needle in the sagittal plane of the spinal long-axis is the primary operation method.
Slightly different from PVB, RLB in the existing literature may require the multi-segmental block to achieve satisfactory results (Onishi et al., 2018), resulting from the dense surrounding structure in the posterior lamina and the limitation of drug diffusion. In the autopsy study, after injecting 0.5% bupivacaine of 20ml containing stain into the posterior lamina of the T4 segment, only upward average diffusion of 3.5cm, downward average diffusion of 10.7 cm, and lateral diffusion of 2.5cm were observed (Sabouri, et al., 2018), and the diffusion ability was weak. It has also been proved in animal studies that the implementation of RLB requires an enormous capacity to increase the diffusivity and the success rate of the block (Damjanovska, et al., 2018). However, there is still a lack of literature to show the optimal concentration and volume in the specific implementation.
Technical advantages and disadvantages of RLB
As an alternative to PBV, RLB can effectively reduce pleural, vascular, and nerve injury caused by the puncture. As far as the current literature is concerned, adverse events have not been reported, but this may be related to the small existing literature. In cadaveric studies, anesthetic drugs have been shown to be effective in paravertebral and even epidural space (Sabouri et al., 2018). Although this view was questioned at an early stage, the latest human imaging studies have found direct evidence that drugs extend to the epidural space after RLB (Adhikary, et al., 2018). The result indicates that RLB can have the effect of incision analgesia but may even produce visceral analgesia and reduce neuroinflammation, and thus is the best alternative to epidural block.
However, the mechanism of drug action of RLB is not precise presently. Some literature speculates that the superior costal transverse ligament may play a role by helping the drug penetrate the paravertebral or even epidural space after RLB injection (Yoshida, 2016), but follow-up research is absent. The plane block of erector spinae muscle developed at the same time has a very similar blocking effect and exhibits a much more extensive spread range than RLB, attracting a large number of scientific research forces in a short time, so the research related to RLB is almost at a standstill in recent years. Due to the lack of relatively high-quality clinical studies, the actual value of RLB may not have been fully developed.
Erector spinae plane block
A brief introduction to ESPB
As a new member of the trunk block family, ESPB was first described by Canadian scholar Forero in 2016 (Forero, et al., 2016). Because it has the advantages of both PBV and RLB, ESPB does improve the disadvantage that RLB blocks the limited spreading scope and develops by leaps and bounds in just a few years.ESPB is a plane block technique, and puncture injection itself does not rely on the direct effect on the nerve. Instead, the local anesthetic injected into a specific fascia plane diffuses and blocks the nerves running in the plane. Similar to PVB, ESPB can be operated at the neck, chest, and waist. Except for analgesia for chronic chest pain in the first case report, several clinical randomized controlled trials which appeared in a short time used ESPB for postoperative analgesia in cardiopulmonary bypass (Krishna, et al., 2019), breast surgery (Gürkan, et al., 2018), cholecystectomy (Tulgar, et al., 2019), hernia surgery (Abu Elyazed, et al., 2019) and renal surgery (Ibrahim, et al., 2019), and these surgeries all achieve satisfactory results. Later cases reports realized ESPB (Kilicaslan, et al., 2020) in lower limb surgery and pediatric surgery (Aksu, et al., 2019), continuing to expand the indications of ESPB.
The implementation method of ESPB
Because ESPB has specific risks and difficulty using body surface localization, it is not recommended by the empirical judgment of surface localization, and ultrasound-guided visualization is often used for puncture. The trapezius muscle, rhomboid muscle, and erector spinae muscle are identified from the surface and depth under ultrasound. The needle's injection target is the vertex of the transverse process; that is, the puncture needle's target is slightly shifted from the lamina of RLB to the lateral 1cm of the transverse process. The drug is injected into the fascial plane between the erector spine muscle and the intercostal muscle. It takes effect by blocking the ventral and dorsal branches of the spinal nerve. However, when injecting the drug, it needs to be observed that the drug spreads in the cranial and/or caudal direction in the erector spine muscle plane (Figure 1).
From the human body's anatomical structure, ESPB can be regarded as a slight improvement of RLB. The posture, selection, and placement of the ultrasound probe of ESPB during clinical operation are very similar to RLB so that ESPB puncture can be completed in both the spine's long and short-axis by in-plane technique. The slight difference between ESPB and RLB is that it may be more beneficial for ESPB to inject the drug into the spinal long axis plane to improve the success rate of blocking, as the drug diffusion on cranial and/or caudal sides needs to be observed.
ESPB can achieve a wide range of block at a single point of the block, which is put forward in the experience of clinical studies and confirmed by cadaveric studies and imaging studies (Adhikary et al., 2018; Schwartzmann, et al., 2018; Yang, et al., 2018). Therefore, the single-point block is often used in the clinic, but whether to implement bilateral block is decided according to surgical analgesia's demand. In the literature related to dose selection, single-point injection of 10ml via ESPB did not involve paravertebral or epidural space. However, there was no increase in paravertebral diffusion beyond 30ml, and when it came to 40m, the possibility of local anesthetic poisoning was significantly increased (Choi, et al., 2019; Luftig, et al., 2018), indicating that the best clinical single-point drug volume is 20-30ml.
Technical advantages and disadvantages of ESPB
As an improvement of PVB and RLB, ESPB has the late-mover advantage, and hundreds of articles have emerged within four years after the technique was made public. First of all, the puncture site of ESPB is superficial, which is very easy to master with the assistance of ultrasound. Secondly, its good cranial-caudal diffusion range makes single-point injection immediately meets the needs of extensive area analgesia. Meanwhile, potential paravertebral and epidural infiltration can also play a role in visceral analgesia.
Similar to RLB, the mechanism of ESPB remains unclear at present. It may be similar to the RLB pathway to penetrate deep through the costal transverse process ligament, but it may also be completely different from RLB, although the two's injection sites are only a few centimeters apart. Some literature speculates that RLB may be more inclined to take effect through the PVB pathway, that is, “deep” penetration, while ESPB mainly produces analgesic effect by affecting lateral cutaneous branches and some small branches of the intercostal nerve through “transverse” penetration. Therefore, in the back's analgesia, RLB may show a better effect than ESPB (Onishi et al., 2019). At the same time, due to the lack of significant muscles (such as rhomboids muscles) in the lower thoracic or lumbar vertebrae, ESPB may not provide adequate analgesia in a wide range of lower thoracic and lumbar vertebrae, where RLB may be more effective (Ueshima, et al., 2017).
Isolated chest wall block technique
In addition to the above methods, several block techniques for chest wall analgesia have been reported in the recent literature. According to the anatomical relationship from proximal to distal, these block techniques can be divided into mid-point transverse process to pleura (MTP), rhomboid intercostal and subserratus plane block (RISS), serratus anterior plane block (SAPB), pectoral blocks (PECB), which are targeted to block the branches of the thoracic spinal nerve, to achieve analgesia in thoracic surgery.
Mid-point transverse process to pleura (MTP)
Canadian scholar Costache first reported MTP in 2017 in breast surgery (Costache, et al., 2017). Then it was reported again in 2019 for postoperative analgesia of rib fractures (Syal, et al., 2019),. The idea of MTP is very similar to that of PVB. Due to the need for drug injection between the transverse process and the pleura, the goal is to make the drug permeate into the paravertebral region to produce an analgesic effect. Therefore, this method is limited to analgesia for lateral and frontal surgery of the chest wall, such as breast surgery and rib surgery (Costache et al., 2017; Syal et al., 2019). Unfortunately, the expansion of its indications has not been reported in the literature recently.
In clinical practice, MTP can be regarded as thoracic PVB far away from the vertebral body, and the posture requirement is similar to that of PVB. The thoracic vertebra segment to be blocked is selected and scanned by the spinal midline long axis under ultrasound guidance. Then the probe is horizontally moved until the ultrasound image clearly shows the transverse process, ribs, trapezius muscle, rhomboid muscle, erector spinae muscles, and pleura in the same section. The needle is injected into the transverse process level, and the midpoint from the erector spine muscle's deep surface to the pleura, but not beyond the superior transverse process ligament, and then the operation is completed after injecting anesthetic (Figure 1). The unilateral or bilateral block is performed according to the operation requirement, and it is usually necessary to complete a multi-point injection to expand the scope of the block to meet the requirement. Due to the lack of good literature, it is only recorded that each injection site can be injected with a local anesthetic of 5 or 15ml (Costache et al., 2017; Syal et al., 2019), and catheterization for continuous analgesia is also permitted.
Rhomboid intercostal and subserratus plane block (RISS)
American scholar Hesham Elsharkawy first reported RISS in 2018 in the form of a cadaver study (Elsharkawy, et al., 2018), and then sporadic reports on its surgical utilization appeared.
RISS is an in-plane fascial block technique performed between the erector spine muscle and the anterior serratus muscle. It is aimed to infiltrate the anesthetic into the lateral cutaneous branch of the thoracic intercostal nerve to achieve the blocking effect. At present, it has been used in video-assisted thoracoscopic surgery (Longo, et al., 2020), open thoracotomy (Kozanhan, et al., 2019), radical mastectomy (Kozanhan, et al., 2019), and cardiac surgery (Ueshima, 2019), but no large sample of clinical randomized controlled trials have been reported.
RISS is similar to ESP farthest block, but the localization method is different. In the literature initially reported, the prone position was used, and a high-frequency linear probe was selected and placed on the medial side of the scapula at the T5-T6 level of the spinal long-axis. Then, the probe's cranial side is slowly rotated inward, and the caudal side is rotated outward about 1-2cm to obtain the RISS operation plane. The trapezius muscle, rhomboid muscle, intercostal muscle, and costal pleural tissue can be identified from shallow to deep in the ultrasound plane, and the anesthetic is injected into the space between the rhomboid muscle and the intercostal muscle, that is, the fascia plane of the lateral edge of erector spinae muscles (Elsharkawy et al., 2018). The inward infiltration of the anesthetic along the plane of the erector spinae muscle can block the dorsal branch of the spinal nerve, spread outward along the fascial plane between the serratus anterior muscle and the external intercostal muscle to the lateral chest wall, and infiltrate the cutaneous branch of the intercostal nerve (Figure 1). Lacking sufficient literature support, the specific block scope and appropriate dosage of RISS need further exploration.
Serratus anterior plane block (SAPB)
SAPB appeared relatively early and was first reported by British scholar Blanco in 2013 (Blanco, et al., 2013), followed by postoperative analgesia reports different parts of the chest and by clinical randomized controlled trials to verify its clinical significance.
SAPB is also an in-plane fascial block technique. Two fascial planes are composed of outer latissimus dorsi, middle serratus anterior, and inner intercostal muscles on the chest wall's lateral side (Figure 1). SAPB aims at injecting the drug into the surface or deep fascia plane to block the lateral cutaneous branch of the intercostal nerve for analgesia. Because SAPB is approximately the improvement of traditional intercostal nerve, its indications also focus on minimally invasive thoracic surgery (Wang, et al., 2019), open thoracotomy (Saad, et al., 2018), breast surgery (Rahimzadeh, et al., 2018) and cardiac surgery (Berthoud, et al., 2018). Recent studies have shown that SAPB can provide a good analgesic effect for upper abdominal surgery, and the scope of effect is T2-T9 level (Fernandez Martin, et al., 2019; Tiwari, et al., 2019).
The puncture point of SAPB is strictly between RISS and PECB, at the level of the axillary midline of the lateral chest wall, so it may be better to perform this operation in the lateral recumbent position. The high-frequency linear array probe's spinal short-axis is placed at the level of the 4th-5th ribs in the midaxillary line. Ultrasonic scanning can identify latissimus dorsi, serratus anterior, intercostal muscle, ribs, and pleural tissue from superficial to deep. The anesthetic is injected into the fascia plane of the serratus anterior muscle's surface or deep surface to complete the operation. The latest literature reported that the idea of SAPB, underbody surface localization, is similar to that of RLB, that is, the target is the bony locating point, and the needle tip reaches the ribs, and then the drug can be injected into the plane of the anterior serratus muscle (Vadera, et al., 2020). However, whether its effect is consistent with the ultrasound-guided SAPB still needs to be verified in the follow-up study. Cadaveric studies have shown that the large volume 40ml double-point injection spreads wider than 20ml single-point infusion, and the analgesia scope may involve a more expansive chest wall and armpit (Biswas, et al., 2018). A clinical randomized controlled study confirmed that 0.5% ropivacaine was better than 0.375% and 0.75% ropivacaine in the same volume state of 20ml and was the most suitable for clinical promotion (Huang, et al., 2020).
Pectoral blocks (PECB)
PECB was first reported in 2011 when a Spanish scholar described a new chest block technique for postoperative analgesia in breast surgery (Blanco., 2011), followed by a randomized controlled study that slightly improved it to classify the technique as type I or II block (Kulhari, et al., 2016).
PECB is also an in-plane fascial block technique. Two fascial planes are composed of pectoralis major muscle, pectoralis minor muscle, and serratus anterior muscle directly in front of the chest wall, and the pectoralis minor muscle is located in the middle of the three layers of muscle (Figure 1). PECB aims at injecting drugs into the surface of the pectoralis minor muscle (PECB type I) or a second injection on its deep surface (PECB type II) to block the intrathoracic, external, and long thoracic nerves originating from the brachial plexus to achieve the analgesic effect. Since PECB type I has been confirmed in follow-up reports that it cannot block the chest wall's skin sensation (Desroches, et al., 2018), it may only have a particular clinical significance for chest muscle strain muscle injury caused by surgery. PCEB type II has an excellent blocking effect on the armpit and has become a prevalent breast surgery technique. Solid evidence has proven the important value of this breast surgery technique (Lovett-Carter, et al., 2019). It has recently been reported that this method has been independently used in non-intubated general anesthesia breast surgery rather than postoperative analgesia (Debbag, et al., 2019). During the implementation of PECB, the patient is placed in the supine position or lateral position. A high-frequency linear probe is selected and placed at the short axis of the pectoralis major muscle at the T3 level in the anterior axillary line.
The pectoralis major, pectoralis minor, ribs, intercostal muscle, and pleural tissue can be identified by ultrasound scanning from superficial to deep. It is worth mentioning that the vascular branches originating from the acromial artery can usually be found in the fascia plane of the pectoralis major and pectoralis minor muscle, often accompanied by the branches of the thoracic nerve. PECB type II refers to puncture to the fascia plane of the pectoralis minor muscle and intercostal muscle to complete the first injection and then back to the fascia between the pectoralis major muscle and the pectoralis minor muscle to complete second injection. In contrast, PECB type II refers to the only fascia plane injection between the pectoralis major muscle and the pectoralis minor muscle. Because of the similar diffusion nature, SAPB is also classified as PECB type III (Ueshima, et al., 2019). Therefore, the drug use of PECB is similar to that of SAPB. For example, 0.5% ropivacaine of 25ml can achieve adequate analgesia and reduce the amount of opioid in radical mastectomy (Kulhari et al., 2016). There are also short reports declare that ultrasound combined with a nerve stimulator can reduce the effective capacity of PECB to 10ml (Ueshima, et al., 2018).
Advantages and disadvantages of Isolated chest wall block technique
These improvements for paravertebral blocks make the clinical puncture farther and farther away from the center part of the body, eliminating the possibility of mechanical injury of nerve roots at the physical level. With the introduction and continuous progress of ultrasound technology, fascia in-plane block has made rapid progress. Depending on various improvements, various block methods can be implemented in different areas of the chest wall according to specific needs, which helps formulate the optimal plan for different patients or types of surgery.
However, these block methods which act on thoracic analgesia alone still have some shortcomings. First of all, the methods mentioned above need puncture in structural attachments such as ribs and pleura, and there is still a potential risk of pneumothorax in pleural injury. Although there are few reports of related adverse events, with the continuous promotion of technique and the expansion of application scenarios, complications should not be ignored. Meanwhile, although the advantages of the new techniques have been confirmed by relevant studies in the iterative process, due to the emergence of many technical means in a short time, the parallel comparison among the new techniques in the same period is relatively absent at present. This is also related to the fact that different isolated chest wall block methods may have their best surgical methods, so it is urgent to make parallel comparative studies.
Isolated abdominal wall block technique
Thanks to the introduction of ultrasound, abdominal block, which often lacks body surface and bony localization, has been extensively developed. Like the isolated chest wall block, in addition to the original techniques of intraspinal analgesia, paravertebral, retrolaminar, and erector muscles and a variety of peripheral trunk block techniques for abdominal wall analgesia have been developed in recent years, among which the more mature ones include transversus abdominis plane block (TAPB), rectus sheath blocks (RSB), quadratus lumborum block (QLB), and the ilioinguinal/iliohypogastric nerve block (II/IHNB)
Transversus abdominis plane block (TAPB)
In 2001, Rafi, an Irish scholar, performed a new abdominal nerve block on 200 patients by body surface localization and puncture loss. Rafi first defined it as a “lumbar triangular approach” nerve block because of the ideal results and reported it (Rafi, 2001). In 2007, McDonnell verified the stability and reliability of the “lumbar triangle” approach through a randomized clinical study, formally named this method as TAPB (McDonnell, et al., 2007), and used it clinically in the same year (Hebbard, et al., 2007). In 2009, Zhang Hong et al. verified the existence of this “plane” in an autopsy study (Tran, et al., 2009). As a result, TAPB has undergone speedy development in the following ten years.
The abdominal wall comprises the skin and subcutaneous tissue, obliquus externus abdominis, obliquus internus abdominis, transversus abdominis muscle, and peritoneum from superficial to deep. The target operation of TAPB is to choose an appropriate approach and inject anesthetic into the fascia plane on the surface of the transversus abdominis muscle to block the thoracic and abdominal nerves for analgesic effect (Figure 2). Because the abdominal wall muscle is “loose” than the chest wall muscle, TAPB has a larger diffusion area after implementation, so enough drugs can be injected at a single point to meet the analgesic needs of most abdominal surgeries. At present, many kinds of literature have reported ultrasound-guided gallbladder surgery, gastrointestinal surgery, obstetrics and gynecology surgery, urology surgery, and the indications of TAPB include almost all abdominal surgeries. Although TAPB can be operated by body surface localization, there is a potential risk of abdominal organ injury based on the sense of loss (O’Donnell, 2009). Therefore, ultrasound guidance is used chiefly in the clinic at present. Ultrasound-guided TAPB may choose the supine position (subcostal margin approach and lateral approach) or lateral supine position (lateral and posterior approach). A High-frequency linear array probe is usually used to obtain high-quality images, but if the patient is obese, there are also cases of using a convex array probe to complete the operation.
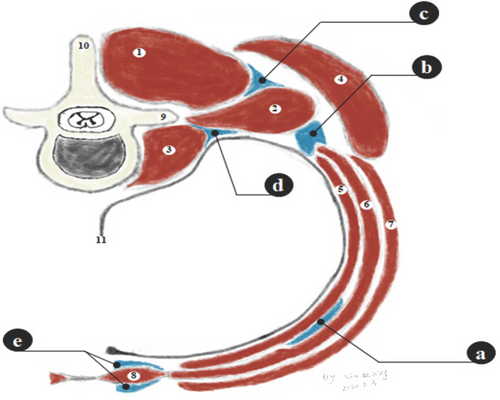
Abdominal nerve block. (1) Erect spinal muscle; (2) Quadratus lumborum; (3) Psoas major muscle; (4) Latissimus dorsi muscle; (5) Transversus abdominis muscle; (6) Obliquus internus abdominis; (7) Obliquus externus abdominis; (8) Rectus abdominis muscle; (9) Transverse process; (10) Spinous process; (11) Pleura. (a) Abdominal transverse fascia block; (b) Type I block of quadratus lumborum; (c) Type II block of quadratus lumborum; (d) Type III block of quadratus lumborum; (e) Block of sheath of rectus abdominis
Ultrasound-guided lateral TAPB is a visual improvement of the classical body surface localization method of “lumbar triangle”. During operation, the probe is placed horizontally at the axillary midline level with the spinal short-axis and the midpoint from the arch's inferior edge and the anterior superior iliac spine. After obtaining the three-layer muscle section by ultrasound, the needle is inserted into the ventral or dorsal medial plane. After reaching the fascia plane, anesthetics are injected to block the anterior branch of the T10-T12 cutaneous nerve to relieve abdominal pain below the umbilical cord. Because the lateral approach cannot provide epigastric analgesia, Hebbard, an Australian scholar who first reported ultrasound-guided TAPB in 2008, once again improved the classical lateral approach and proposed the “oblique subcostal” method, which is the subcostal approach used today (Hebbard, 2008). In ultrasound-guided subcostal approach, the probe is horizontally placed under the xiphoid process, rectus abdominis is identified, and then the probe is rotated counterclockwise until parallel to the costal margin and then slid to the outside until the obliquus externus abdominis, obliquus internus abdominis, and transversus abdominis muscle appear on the lateral edge of rectus abdominis muscle.
Moreover, the drug is injected into the fascia plane of the deep surface of obliquus internus abdominis and rectus abdominis muscle and the surface of transversus abdominis muscle to block the anterior branch of the T6-T9 cutaneous nerve to complete abdominal analgesia above the umbilical cord. Based on the lateral approach, the posterior approach uses the probe to moves to the posterior axillary line. When the aponeurosis of quadratus lumborum, obliquus externus abdominis, obliquus internus abdominis, and transversus abdominis muscle are identified by ultrasound, the anesthetic is injected into the fascia plane to block the collateral branches of the cutaneous nerve in order to expand the analgesic coverage area and prolong block time, which may be caused by the local anesthetic penetrating into the paravertebral and sympathetic chain of T4-L1 through the posterior approach (Finnerty, et al., 2012).
According to the type of operation and the demand for analgesia, TAPB can choose a unilateral block, bilateral block, or catheterization for analgesia. Bilateral TAPB is necessary for abdominal surgery whose incision crosses the midline. Consequently, local anesthetic drugs with large volumes and high concentrations may increase local anesthetic poisoning risk. Some studies used 100mg ropivacaine to inject into one side of TAP, with the volume of 20ml (0.5%), 30ml (0.33%), and 40ml (0.25%), respectively and repeated the postoperative analgesia of bilateral block in gynecological surgery. The results showed that high volume had no advantage of expanding the block scope but had a longer block time (Forero, et al., 2015), suggesting that TAPB of 20ml satisfy the diffusion demand. Another study observed gastrointestinal surgery and showed that TAPB with 0.5% ropivacaine was more beneficial for elderly patients to undergo radical resection of rectal cancer (Ping, et al., 2018).
Quadratus lumborum block (QLB)
QLB was first proposed by the British scholar Blanco in 2007 and was described as a “variant” approach of TAPB (Blanco, 2007). In 2013, Danish scholar Børglum proposed the famous ultrasonic waist “clover” structure, that is, the lumbar transverse process referred to the stem, psoas major muscle and erector spinae muscles referred to the left and right lobe, respectively, and quadratus lumborum was located in the parietal lobe of this structure (Børglum, et al., 2013). All the above is effectively different from the TAPB. At this point, QLB as an independent method of nerve block began to develop gradually.
QLB involves a set of complex muscle-fascial complexes, including erector spinae muscles and its anterior and posterior layer of the thoracolumbar fascia, quadratus lumborum and its anterior layer of the thoracolumbar fascia and the quadratus lumborum fascia, obliquus internus abdominis and transversus abdominis muscle, and the transversal fascia between them (Ueshima, et al., 2017). When performing QLB, an appropriate approach is chosen, and anesthetic is injected into the thoracolumbar fascia or quadratus lumborum fascia to infiltrate the T12 subcostal nerve, iliohypogastric ilioinguinal nerve, genitocrural nerve, and thoracoabdominal nerve to achieve the analgesic effect (Adhikary, et al., 2017; Elsharkawy, et al., 2017). QLB can be used for analgesia in intraperitoneal and retroperitoneal operations, such as hepatobiliary surgery (Okmen, et al., 2018), gastrointestinal surgery (Cardoso, et al., 2018), renal surgery (Aditianingsih, et al., 2019), gynecological surgery (Krohg, et al., 2018). Because the thoracolumbar fascia has thoracolumbar continuity, the lower extension can provide analgesia for hip surgery (Bak, et al., 2019). In cadaveric studies, it is suggested that QLB infiltrates upward to T5 level (Elsharkawy et al., 2017), so its indication is wider than that of TAPB. QLB can take a lateral position or take a height seat in the operative side of the horizontal position to expose the waist and abdomen. QLB, which started with ultrasound-guided technique, has a deep operation site, and the puncture location is close to several important anatomical structures, so there are no reports about the operation completed by body surface positioning. Ultrasound guidance often requires a low-frequency convex array probe to identify the anatomical structure of deep tissue better. After more than ten years of development, the operation approach of QLB has been developed rapidly. At present, the literature reports mainly focus on three different injection locations: QLB type 1 (Figure 2), QLB type 2 (Figure 2), and QLB type 3 (Figure 2). The ultrasound-guided probe is placed along the spinal short-axis on the anterior superior iliac spine. Furthermore, the probe is slid to the head to obtain the cross-sectional image of the waist. The probe's corresponding height is selected according to the blocking demand, and the “clover” structure of the waist and the three-layer muscles of obliquus internus abdominis, obliquus externus abdominis, and transversus abdominis muscle is selected to obtain the necessary sections for QLB implementation. QLB type 1 is located at the contact point between the lateral edge of quadratus lumborum and TAP, can be regarded as the continuation of TAPB in the waist. The local anesthetic is injected into the fascia plane by in-plane injection to complete the operation. Since this point lives the posterior edge of the transversalis fascia, drugs can infiltrate forward to TAP and inward to the anterior part of the thoracolumbar fascia and quadratus lumborum fascia after injection. This is the main reason why QLB is considered as a “variant” of TAPB when it came out. On the other hand, QLB type 2 makes a slight change to the injection target. It punctures into the outer edge of the obliquus internus abdominis and the anterior layer of the thoracolumbar fascia between erector spinae muscles and quadratus lumborum, which was very similar to the RISS in chest block.On the other hand, QLB type 3 is an excellent improvement on the above two approaches. It has a similar anatomical site of the puncture point with MTP in the thoracic block. The target point is located in the transverse process's deep surface and the quadratus lumborum fascia between quadratus lumborum and psoas major muscle. Drugs then infiltrate quadratus lumborum fascia and psoas primary muscle space after injection. QLB type 4 also exists, which injects drugs directly insides the quadratus lumborum. At the same time, it is not discussed in this paper due to little related literature.
According to the demand for analgesia, QLB can perform the unilateral or bilateral block. Because QLB involves multiple fascia planes, large-capacity local anesthetics are often required to consider the needs of each plane, such as at least 30ml at a single point. Ropivacaine with 100ml (0.1%) was even reported in the literature to provide analgesia because of renal surgery (TSUCHIYA, et al., 2018).
Rectus abdominis block (RSB)
RSB was first used in abdominal surgery to relax abdominal muscles, and the literature used to relieve postoperative pain could be traced back to the 1980s. Bilateral rectus abdominis sheath block was used in diagnostic laparoscopy for postoperative analgesia and obtained satisfactory results (BE, et al., 1988). As a result, this method gradually came into the field of vision of anesthesiologists. In 1996, British scholars proposed that RSB had a very high value in postoperative analgesia in children’s umbilical hernia repair (S, et al., 1996). In contrast, the report of ultrasound-guided RSB appeared ten years later in 2006, which proved that ultrasound-guided RSB was safer and more effective (Willschke, et al., 2006). RSB involves the structure of fascia sheath composed of multi-layer aponeurosis, including skin and subcutaneous tissue, aponeurosis of obliquus externus abdominis, aponeurosis of obliquus internus abdominis, aponeurosis of transversus abdominis, rectus abdominis, transversalis fascia, and peritoneum. During the operation, anesthetics are injected into the anterior sheath (on the surface) or the posterior sheath (on the deep surface) of the rectus abdominis to infiltrate the terminal cutaneous branches of the 9-11 costal nerve to relieve pain in the median abdominal incision (Figure 2). However, due to its terminal cutaneous branch nerve, whether there is an advantage over local infiltration remains controversial (Rajwani, et al., 2014). RSB can be performed by body surface localization and surgeons under direct vision before closing the abdominal cavity (Crosbie, et al., 2012). The introduction of ultrasound greatly reduces the difficulty of operation. The main point of anesthesiologists to perform RSB is to complete the operation before skin incision, aiming to reduce the use of perioperative opioids and improve anesthesia management quality.
Rectus abdominis muscle should be exposed in a supine position during RSB operation. A High-frequency linear array probe is usually used to meet the need immediately because of the superficial position in ultrasound guidance. By placing the probe horizontally in the abdomen's center, the rectus abdominis and the rectus abdominis sheath on its deep surface can be easily identified. The in-plane needle inserting technique is used to inject anesthetic into the anterior sheath and posterior sheath to complete the operation. When it comes to abdominal median incision analgesia, the bilateral block is often needed, while unilateral surgery often plays an auxiliary role in analgesia. Drug volume selection should include the total dose of all blocks for personalized design and configuration.
Ilioinguinal/iliohypogastric nerve block (II/IHNB)
The iliohypogastric and ilioinguinal nerves originate from the lumbar spinal nerves, but due to the lower abdomen and groin's partial operation in modern surgery, II/IHNB has a unique clinical significance. As early as 1988, there was a concentration analysis of bupivacaine for nerve block at this site (P. J. STOW, 1988). In 2005, it was reported that ultrasound-guided II/IHNB was used in inguinal surgery in children (Willschke, et al., 2005), and then introduced into adults in 2007 (Hu, et al., 2007). However, with the technological progress and the emergence of various new trunk block techniques, II/IHNB has entered a controversial era. Some kinds of literature have confirmed that ESPB is superior to II/IHNB in inguinal surgery analgesia (El-Emam, et al., 2019). Nevertheless, compared with TAPB, II/IHNB alsohas some advantages in inguinal analgesia (Faiz, et al., 2019). QLB and II/IHNB almost have the same effect (Samerchua, et al., 2020). Therefore, recently there are still pieces of literature to explore the value of this operation, but whether new blocking methods eliminate II/IHB or whether it continues to maintain its unique charm still needs to be verified by follow-up research and practice.
The iliohypogastric and ilioinguinal nerve branches from the lumbar spinal nerve walk between the psoas quadratus muscle and the psoas major muscle and migrate to the superficial surface. Although QLB type 3 can effectively infiltrate these two nerves, the general description of II/IHNB refers to the block completed in the anterior superior iliac spine's deep surface. Body surface localization can complete this operation, but because there is often much uncertainty in clinical practice by relying on the sense of fascia breakthrough, even skilled operators of II/IHNB without direct vision may have a 45% chance of block failure (Weintraud, et al., 2008), which greatly reduces the value of this technology. Therefore, at present, it is advocated to complete the operation under the guidance of ultrasound.
During the implementation of II/IHNB, the patient is placed in a supine position, and a high-frequency linear array probe is placed obliquely on the medial side of the anterior superior iliac spine and the long axis of the probe is perpendicular to the long axis of the ilium. The probe is then slid along both sides of the anterior superior iliac spine to show the block's necessary sections. From superficial to deep, skin and subcutaneous tissue, obliquus externus abdominis, obliquus internus abdominis, transversus abdominis muscle, and peritoneum can be identified. The iliohypogastric nerve, ilioinguinal nerve, and its accompanying iliohypogastric vessels can often be observed on the iliac side of the transversalis fascia. The operation is completed by injecting drugs into the transversalis fascia, where the nerve is located by in-plane or out-of-plane techniques. The ultrasound-guided II/IHNB is more similar to the lowest abdominal TAPB. As II/IHNB is often involved in the compound block, its capacity requirement is similar to that of RSB, so the total amount should be adjusted according to the requirement. Literature studies have shown that the 50% effective concentration of ropivacaine for II/IHNB is 0.21% (Yamada, et al., 2016), and this concentration may also be the lowest effective concentration for many fascial blocks aimed at branch nerves.
Technical advantages and disadvantages of isolated abdominal wall block
Unlike isolated thoracic block techniques, some abdomen techniques have been around for decades. Because it is easier to perform intraspinal anesthesia in abdominal surgery than in the chest, abdominal trunk block development is limited to some extent. Likewise, thanks to the introduction of ultrasound, the fascia plane block concept has been developed synchronously in abdominal wall analgesia, which makes some patients who are inconvenient to use intraspinal analgesia can benefit from it. The trunk block techniques almost ending the era of simple intraspinal analgesia, the way of abdominal surgery analgesia has been enriched, and its comfortableness has been dramatically improved.
However, these block methods also have shortcomings. First of all, the above methods need to be punctured in the abdominal wall, and there is still a potential risk of peritoneal injury and even abdominal visceral injury. Simultaneously, consistent with the plight of other emerging technologies, different block methods or the same block methods with different approaches may also be different in fount of the same patients, which requires a lot of research and clinical exploration.
Part II: Ultrasound-guided peripheral trunk block promotes the revolution of clinical anesthesia management strategy
With the modern anesthesia management strategy reform, ultrasound-guided peripheral trunk block techniques have gradually become one of the new protagonists in the clinical anesthesia stage. The fascia plane block's breakthrough enables the perioperative analgesic management of trunk surgery to share the dividend of technological progress.
Although general anesthesia, intraspinal anesthesia, and peripheral nerve block are still the three basic blocks of modern anesthesia techniques, more and more compound, combined anesthesia, and more trunk block techniques have become valuable choices in clinical anesthesia, which together have a profound impact on improving the quality of perioperative anesthesia management after nearly a decade of development.
Dose and the toxic reaction of local anesthetics
The local anesthetic dose required for peripheral nerve block depends on the anesthetic target. The ultrasonic visualization, the needle tip, the structure at the puncture site, and the local anesthetic diffusion are visible, so the local anesthetic dose begins to decrease. Among earlier literature that involved ultrasound-guided nerve block in the upper limbs (P, et al., 2011) or analgesia in the lower extremities (Casati, et al., 2007), dose reduction in local anesthetics always attracts our attention. Therefore, the good news that naturally follows is the probability decrease of local anesthetic poisoning caused by a decrease in the practical dose (Barrington, et al., 2013). A large sample study reported that in 80661 cases of peripheral nerve block between 2009 and 2014, the ultrasound utilization rate increased from 48% in 2009 to 90% in 2014, and there were only 3 cases of local anesthetic poisoning with direct evidence, and the incidence decreased to a staggering 0.04/1000 (Liu, et al., 2016). As a result, a peripheral nerve block is getting rid of the label of a local anesthetic toxic reaction, and the era of getting rid of it ultimately seems to be just around the corner.
The development of peripheral trunk nerve block is inseparable from the fascia plane block, which is different from the traditional upper and lower limb nerve block. The fascia plane block needs to let the local anesthetic spread in the fascia to widely infiltrate the target nerve or nerve plexus (Elsharkawy, et al., 2018). It is not difficult to imagine that in the absence of TAPB, a patient undergoing laparoscopic surgery may rely on local anesthesia infiltration of intravenous anesthesia. While in the era of ultrasound, he may receive high-dose local anesthesia for TAPB. It is not denied that patients can get a variety of beneficial possibilities after TAPB, but the change from zero to one does not rule out local anesthetic poisoning in the clinic.
Moreover, there is evidence that fascial plane block absorbs the drug quickly after injection and advances to the toxic threshold within two hours (Toju, et al., 2014). As mentioned earlier, RLB, ESPB, QLB, and other peripheral trunk block techniques mainly belong to the fascial plane block. With the promotion of existing techniques and the invention of new techniques, whether the incidence of local anesthetic poisoning reaction in clinical practice continues to decline or bottomed out deserves much more attention.
Transition of complications of nerve block
The injury of the puncture site's blood vessels, nerves, and adjacent tissue structures is a common complication in nerve block. With the utilization of ultrasound, a large sample of observational studies have shown that the incidence of vascular injury has been effectively controlled (Barrington, et al., 2009). based on inheriting this advantage, ultrasound angiography behaves well in trunk block: because of the need to block the terminal branch nerve, the smaller nerve is challenging to display clearly, while the blood vessel can be displayed in the ultrasound section. Therefore, the characteristics of accompanying blood vessels and nerves can be used to target blood vessels in the target area and complete block around them, which can not only effectively avoid vascular injury but also improve the success rate of the block, of which the most representative are PECB (type I) and II/IHNB. Although it is also possible to reduce nerve injury under ultrasound guidance, a study involving the data of more than 20,000 people over ten years showed that the total incidence of nerve injury after ultrasound guidance (1-3/1000) was indeed lower than that of body surface localization (5-9/1000). However, there was no significant difference in injury after six months (Melnyk, et al., 2018). It is difficult to conclude that the application of ultrasound directly leads to decreased nerve injury, and this problem is more complicated in trunk blocks. On the one hand, as the trunk nerve block's development trend is more and more “far away from the trunk”, puncture has led to less possibility of direct nerve injury. On the other hand, it is unknown whether the high local tension may lead to terminal nerve branches' injury due to the injection of large volume local anesthetic into the fascia plane block.
From the historical trend of the hot spots in the development of trunk block, we can infer that the site of puncture block is “getting farther and farther away”. Due to many thoracic epidural puncture problems, PVB appears on the stage after ultrasound lowers the threshold of execution. There is the possibility of serious adverse events, the subsequent development of trunk block presents from the paravertebral to the lamina, to the transverse process, to the side of the thoracic and abdominal wall, or even to the front of the thoracic and abdominal wall. In theory, trunk block eliminates malignant adverse events such as intraspinal hematoma and general spinal anesthesia. But to benefit from the advantages of the new techniques, we have to bear the risks because trunk block still has potential risks, that is, being away from the spinal nerve but closer to the body cavity. Even with the latest vertical spinal muscle block, adverse events such as pneumothorax have been reported (Ueshima, 2018), and it is difficult to explain the lack of proficiency in the new techniques, as some scholars have begun to discuss the improvement of the operation of the erector spinae muscles to reduce the possibility of pneumothorax (Piraccini, et al., 2020). According to this analogy, trunk blocks will gradually mature after a new period. In this process, the safety of various methods and approaches tends to focus on academic discussion in recent years.
Trunk block involved multimodal analgesia and enhanced recovery
The patient’s pain was successfully promoted to “fifth vital sign” based on a 1995 acute pain management guide (Committee, 1995). After more than 20 years of great attention to pain management, satisfactory clinical changes have been made, but at the same time, it has also brought trouble, that is, opioid abuse in analgesia management (Becker, et al., 2017). In addition to addiction, nausea, and vomiting, respiratory depression, and other problems make the perioperative opioid analgesia management strategy and multi-mode analgesia plan more and more popular in the industry (Elkassabany, et al., 2019).
In 2016, several medical associations in the United States jointly issued perioperative pain management guidelines that strongly recommended implementing perioperative multimodal analgesia and regarded peripheral nerve block as the main component of multimodal analgesia based on high-quality evidence (Chou, et al., 2016). Moreover, more and more enhanced recovery after surgery (ERAS) subspecialist guidelines are beginning to recommend including trunk nerve block in the management of postoperative analgesia. For example, for lung surgery, ESPB is recommended as one of the main analgesic methods, and SAPB is recommended to specifically deal with severe pain (Gao, et al., 2019). In another clinical guideline on ERAS for colorectal surgery, transversalis fascia block is recommended for postoperative analgesia in minimally invasive colorectal surgery with the most robust evidence (Gustafsson, et al., 2018). After the success of orthopedic limb surgery, the status of nerve block in multimodal analgesia and ERAS has been established. The progress of peripheral trunk nerve block has been gradually recognized in thoracic and abdominal surgery. A peripheral trunk nerve block is no longer the icing on the cake in combined anesthesia, but an indispensable part of anesthesia management and is becoming a new protagonist (Brown et al., 2018).
Challenges of ultrasound-guided peripheral trunk block
The development of peripheral trunk nerve block is facing many challenges, among which the most critical and urgent clinical problem is how to prolong the drug duration after a single block. The duration of peripheral nerve block is affected by drug pharmacology, concentration volume, injection site, and other factors. Significantly, diabetic patients with peripheral neuropathy may also affect the drug duration(Baeriswyl, et al., 2018). The duration of a single nerve block can rarely cover the whole course of operation, but the pain rebounds after the block's gradual failure, and the connection of multi-mode analgesia still challenges clinicians' management ability.
Continuous catheterization for analgesia
A peripheral nerve block with catheterization for continuous analgesia was first reported in 1946 when anesthesiologists performed catheterization for continuous analgesia in 27 patients with brachial plexus block (FP, 1946). After entering the 21st century, with the cooperation of real-time visualization of ultrasound, the indication of continuous analgesia by catheterization continues to expand from limb orthopedic surgery to trunk thoracic and abdominal surgery (Ilfeld, 2017). Its principle is similar to catheterization for continuous epidural analgesia. The catheter is placed in the trunk block target area, and continuous administration is carried out after operation to achieve continuous analgesia.
However, continuous analgesia by catheterization is not the best combination of nerve block techniques. On the one hand, catheter placement as an additional operation not only increases the difficulty of operation, the pressure of nursing, and the cost of hospitalization but also increases the risk of local compression and infection and even the adverse reactions caused by long-term block (Fredrickson, et al., 2016). On the other hand, it is still unclear whether the benefits of continuous analgesia are consistent among all methods or are only effective for specific methods (Ilfeld, et al., 2019).
Increasing the use of adjuvant drugs to prolong the adequate time
The addition of adjuvant drugs to local anesthetics has a long history, but the most well-known epinephrine combination to peripheral nerve block can only prolong the analgesic time of 1 hour (Tschopp, et al., 2018), and must pay the cost of increased blood pressure and heart rate. Dexmedetomidine has an analgesic time of nearly 6 hours and a shorter prolongation time than dexamethasone (Albrecht, et al., 2019), and also need to face the problems of excessive sedation, bradycardia, over-instruction. According to the clinical literature, buprenorphine has the longest prolongation for local anesthetics and can effectively prolong the analgesic time of local anesthetics for more than 8.5 hours, but it will bring more than five times the incidence of nausea and vomiting (Schnabel, et al., 2017). The research on the combination of dexamethasone to prolong local anesthesia's analgesic time has been mature enough. At present, the most appropriate dose and intravenous use of 4mg dexamethasone have been found, which can effectively prolong local anesthesia time up to 8 hours (Albrecht, et al., 2019). Because there is no apparent adverse reaction, dexamethasone seems to be an ideal adjuvant for the clinic's nerve block. Unfortunately, the most clinically used combination of dexamethasone and ropivacaine may produce particle crystallization, and this kind of crystal may have the potential risk of getting into the blood vessels (Watkins, et al., 2015).
Therefore, the addition of various adjuvant drugs can indeed prolong the analgesic time of local anesthesia. What is worrying is that they all have interference factors, and some cases may lead to new problems that make the management of analgesia more and more complex. Therefore, we desperately need a breakthrough in drug research and development. It is conceivable that a safe and long-acting local anesthetic drug that can last for 72 hours or even a week may make complex adjuvant drugs no longer compulsory in peripheral trunk block, whose indications will also be significantly improved.
Improvement of surgical prognosis by peripheral nerve block
Peripheral nerve block is currently used mainly for postoperative analgesia and have a very important place in multimodal analgesia, let along the dominant role in de-opioidized analgesia programs, which may effectively reduce the occurrence of adverse events such as postoperative nausea and vomiting and respiratory depression. In addition, as the peripheral nerve block continues to develop, the technical features of which may break through the category of postoperative analgesia and become another major anesthetic modality in addition to general anesthesia and intralesional anesthesia in torso surgery. Finally, beyond analgesia, the peripheral nerve block is expected to make the same breakthrough in inflammation control and become an important component of rapid surgical recovery.
Conclusion
Peripheral trunk nerve block guided by ultrasound has changed the management ideas and strategies of clinical anesthesia. This technological revolution is no longer icing on the cake but has shown an irreversible trend in the application of modern anesthesia. The pace of development is so rapid that some sort of improvement on the old techniques and some technological development of regional block seems to emerge every day. Facing patients who undergo trunk, thoracic and abdominal surgery, clinical anesthesiologists have unprecedented and multiple choices when planning postoperative analgesia. Almost every inch of the chest and abdomen skin has corresponding nerve block methods for analgesia, and each specific operation of thoracic and abdominal organs has 1-2 most suitable nerve block approaches. In addition to laryngoscope and syringe, ultrasound has become the most common equipment and valuable anesthesiologists' tools. Ultrasound-guided peripheral trunk block is gradually becoming a new protagonist in the clinical anesthesia stage.
It is undeniable that there are still many problems in applying ultrasound in anesthesia practice, and the combination of anesthesiologists and ultrasound is still far from perfect. But fortunately, we have found the right partner and are moving in the right direction to benefit patients. One day, the combination of ultrasound and anesthesia will undoubtedly become more and more perfect.
Ethical statement
Not applicable.
Acknowledgements
Not applicable.
Funding
This work was supported by Joint Fund of Zunyi Science And Technology Bureau [grant numbers ZUNSHIKEHE.HZ (2019)97].
Conflict of interest
There is no conflict of interest in this study.
Transparency statement
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Authors' contribution
De-Xing Liu contributed to conceive the study and collect the literature, write the paper, drawing and modify the article; Zhao-Qiong Zhu contributed to guidance and inspection.