Recurrence of seminoma 48 years after orchiectomy: Longest late recurrence and treatment
Abstract
Introduction
Although not frequent, the recurrence of seminoma later than 5–10 years after orchiectomy has been reported. We report a case of recurrence of seminoma 48 years after orchiectomy, with metastasis to the para-aorta that was treated with chemotherapy.
Case presentation
An 83-year-old man had an incidentally enlarged para-aortic lymph node noted on computed tomography. Needle biopsy revealed metastasis from a seminoma that had been treated with orchiectomy at age 35. Chemotherapy was introduced but discontinued after the first course due to side effects. However, a decrease in fluorodeoxyglucose accumulation on positron emission tomography was observed, with no subsequent re-enlargement of the tumor.
Conclusion
Chemotherapy was introduced for an elderly patient with the longest known late relapse. Dose reduction should be considered in cases with good prognosis, considering factors such as age.
Keynote message
Stage I seminomas rarely recur 5–10 years after orchiectomy. This study showed the longest late recurrence in the literature, treated with chemotherapy. Considering the side effects of chemotherapy, a dose reduction should be discussed for the treatment of elderly patients with a good prognosis.
Abbreviations & Acronyms
-
- CT
-
- computed tomography
-
- FDG
-
- fluorodeoxyglucose
-
- IGCCC
-
- International Germ Cell Consensus Classification
-
- PET
-
- positron emission tomography
-
- TGCT
-
- testicular germ cell tumors
Introduction
TGCT predominantly affect young men, with U.S. statistics showing that more than 50% of new cases are between the ages of 20–34.1 Most of the patients are young, but there is no specific indication of follow-up after the 5th year.2 The report showed that 6.6% of stage I seminomas relapsed 6 years after diagnosis.3 The longest recurrence reported was 43 years postoperatively.4
In this report, we describe a case of metastasis to a para-aortic lymph node 48 years after orchiectomy, the longest recurrence case reported to date. We treated the elderly patient in the good prognosis group with chemotherapy. A literature review of individualized chemotherapy dose reductions is also presented.
Case presentation
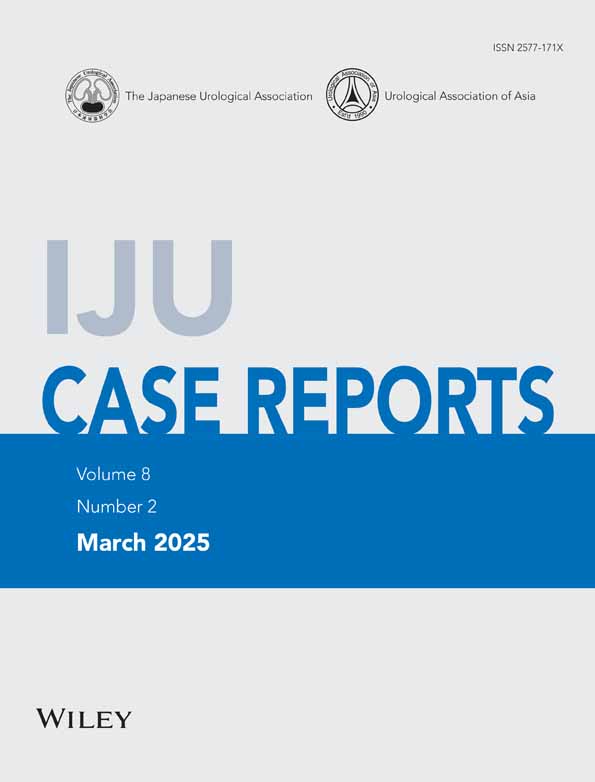
At the age of 35, the patient underwent radical inguinal orchiectomy for a left testicular tumor. The histological result was pure seminoma, and periodic imaging examinations were completed, showing no recurrence. It was unclear how long the patient had been followed up, as no medical records were kept. According to the patient, he had undergone radiotherapy to the abdomen after the surgery. Forty-eight years later, at the age of 83 years, an incidental 17 mm para-aortic lymphadenopathy was discovered on a CT scan. Six months later, the lymph node was enlarged to 45 mm in size (Fig. 1a,b). PET was performed for suspected recurrence of the seminoma, and a CT-guided biopsy was performed because of FDG accumulation in the enlarged para-aortic lymph node (Fig. 1c).
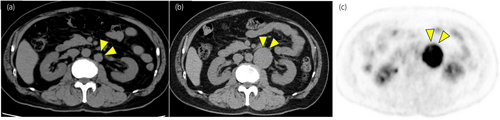
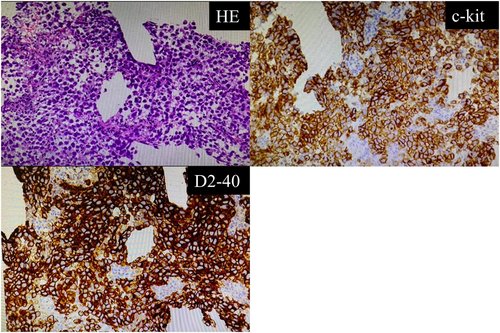
The biopsy specimen showed a proliferation of cells with pale, well-defined nucleoli forming irregularly fused nests. The stroma was infiltrated with lymphocytes and showed a two-cell pattern. Immunostaining was positive for c-kit and D2-40 (Fig. 2). Human chorionic gonadotropin and alpha-fetoprotein blood levels were within normal limits. Based on these findings, we diagnosed recurrent metastatic seminoma, Stage II B, with a good prognosis according to the IGCCC.5 The patient's treatment was planned with four cycles of etoposide and cisplatin (EP), but the treatment was interrupted during the first course at full dose due to grade 4 febrile neutropenia and grade 4 paralytic ileus. A CT scan was performed after the first course, and the mass had shrunk to 22 mm (Fig. 3).
PET after one cycle of EP therapy showed a decrease in FDG accumulation. Although the tumor remained, decreased tumor viability was suggested (Fig. 4). Currently, 1 year and 6 months have passed since the completion of the first course of EP therapy, and the lymph nodes have shrunk from 22 mm to 14 mm, with no apparent recurrence on CT.

Discussion
We reported a case of seminoma that recurred in a para-aortic lymph node 48 years after orchiectomy. In addition, EP therapy was successfully performed to control the disease in an 83-year-old patient with recurrence.
To our knowledge, this is the longest late relapse reported to date. Cummins et al.6 reported a median time to relapse of 15.5 months for stage I seminomas. Conversely, 6.6% of recurrences have been reported to occur after the 6th year,3 and there are scattered reports of recurrence after 10 years.7 For stage I seminomas, the risk factors for recurrence when postoperative no-treatment follow-up is chosen are a testicular tumor diameter of 4 cm or greater and invasion of the rete testis.3 The 5-year recurrence rate was previously reported to be 32% when both factors were present, 16% when one of the factors was present, and 12% when neither factor was present. In this case, medical records dating back more than 40 years were not available, and the presence or absence of both factors was unknown. The cause of the rapid growth in metastatic lymph nodes during follow-up after a long time after orchiectomy is unknown. The accumulation of genetic mutations over time may be involved.
As for the treatment, chemotherapy was introduced with EP therapy for recurrent seminoma in the 80s, and only one course of chemotherapy was sufficient to achieve a therapeutic effect. However, the patient could not complete the planned number of courses due to side effects during the treatment. Feldman et al.8 reported that 30 of 50 GCT patients aged 50 years or older who had received platinum-based chemotherapy as first-line treatment had side effects that delayed treatment for more than 7 days or forced a regimen change. Recently, Loriot et al.9 reported the de-escalation of chemotherapy to reduce the toxicity of seminomas in a group with good prognosis. In a previous study, advanced seminomas of stage IIB or higher were evaluated with PET-CT after two courses of EP therapy, and if positive, two additional courses of EP therapy were performed. If negative, only one additional course of carboplatin was administered at area under the curve 7. The 3-year progression-free survival was 90.8%, comparable to the 5-year survival rate of 89% in the 2021 IGCCCG update.10 As for treatment toxicity, a significant reduction in peripheral neuropathy and other toxicities was reported in the group that received the reduced dose of EP therapy.
As a treatment for stage II seminomas, meta-analyses have shown that radiation therapy has a similar therapeutic effect to chemotherapy.11 In the present case, chemotherapy was chosen because of a history of radiation therapy with unknown details. Nevertheless, radiation therapy should also be considered, especially in elderly patients in terms of treatment burden.
In this case, a needle biopsy specimen could be performed to make the diagnosis. If the patient has an enlarged para-aortic lymph node with an unknown primary site or metastatic tumor to other organs, a history of TGCT more than 10 years ago may help to make the diagnosis.
In the present case, we reported a TGCT that recurred in a para-aortic lymph node at the age of 83 years, 48 years after orchiectomy. Although the planned EP treatment could not be completed, sufficient therapeutic effect was obtained. A reduction of chemotherapy for seminoma, in cases with good prognosis, should be considered, considering PET-CT findings, age, and the general condition of the patient.
Author contributions
Shinya Miyazaki: Writing – original draft; writing – review and editing; data curation. Ryota Ogura: Writing – review and editing; data curation. Munehiro Ohashi: Data curation. Teruki Shimizu: Data curation. Hideto Taga: Data curation. Takashi Ueda: Writing – review and editing. Masayoshi Okumi: Supervision. Fumiya Hongo: Supervision. Osamu Ukimura: Supervision.
Conflict of interest
Osamu UKIMURA, Editor-in-Chief, and Fumiya Hongo, Managing Editor of the International Journal of Urology, are co-authors of this article. They were excluded from all editorial decisions regarding the acceptance and publication of this manuscript.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Informed consent was obtained from the patient for the publication of this case report.
Registry and the Registration No. of the study/trial
Not applicable.