STAT3 inhibition sensitizes colorectal cancer to chemoradiotherapy in vitro and in vivo
Melanie Spitzner
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorBirte Roesler
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorChristian Bielfeld
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorGeorg Emons
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJochen Gaedcke
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorHendrik A. Wolff
Department of Radiotherapy and Radiooncology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorMargret Rave-Fränk
Department of Radiotherapy and Radiooncology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorFrank Kramer
Department of Medical Statistics, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorTim Beissbarth
Department of Medical Statistics, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJulia Kitz
Department of Pathology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJürgen Wienands
Department of Cellular and Molecular Immunology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorB. Michael Ghadimi
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorReinhard Ebner
Genetics Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
Search for more papers by this authorThomas Ried
Genetics Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
Search for more papers by this authorCorresponding Author
Marian Grade
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Correspondence to: Marian Grade, Department of General and Visceral Surgery, University Medicine Göttingen, Robert-Koch-Str. 40, 37075 Göttingen, Germany. Tel.: +49-551-39-6944; Fax: +49-551-39-12550; E-mail: [email protected]Search for more papers by this authorMelanie Spitzner
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorBirte Roesler
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorChristian Bielfeld
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorGeorg Emons
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJochen Gaedcke
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorHendrik A. Wolff
Department of Radiotherapy and Radiooncology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorMargret Rave-Fränk
Department of Radiotherapy and Radiooncology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorFrank Kramer
Department of Medical Statistics, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorTim Beissbarth
Department of Medical Statistics, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJulia Kitz
Department of Pathology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorJürgen Wienands
Department of Cellular and Molecular Immunology, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorB. Michael Ghadimi
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Search for more papers by this authorReinhard Ebner
Genetics Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
Search for more papers by this authorThomas Ried
Genetics Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
Search for more papers by this authorCorresponding Author
Marian Grade
Department of General and Visceral Surgery, University Medicine Göttingen, Göttingen, Germany
Correspondence to: Marian Grade, Department of General and Visceral Surgery, University Medicine Göttingen, Robert-Koch-Str. 40, 37075 Göttingen, Germany. Tel.: +49-551-39-6944; Fax: +49-551-39-12550; E-mail: [email protected]Search for more papers by this authorAbstract
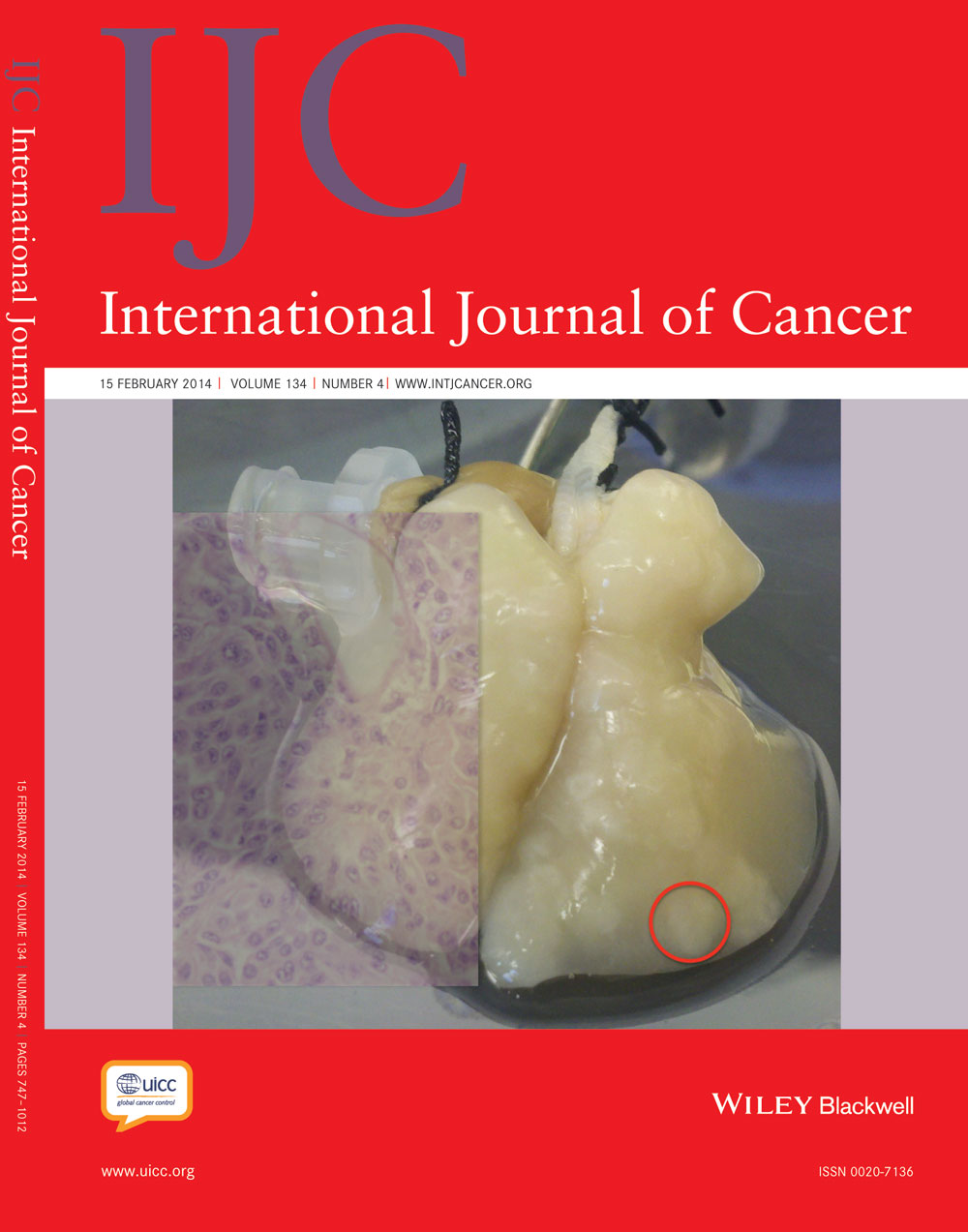
Increased activity of signal transducer and activator of transcription 3 (STAT3) is common in human malignancies, including colorectal cancers (CRCs). We have recently reported that STAT3 gene expression correlates with resistance of CRC cell lines to 5-fluorouracil (5-FU)-based chemoradiotherapy (CT/RT). This is of considerable clinical importance, because a large proportion of rectal cancers are resistant to preoperative multimodal treatment. To test whether STAT3 contributes to CT/RT-resistance, we first confirmed that STAT3 protein expression correlated positively with increasing resistance. While STAT3 was not constitutively active, stimulation with interleukin-6 (IL-6) resulted in remarkably higher expression levels of phosphorylated STAT3 in CT/RT-resistant cell lines. A similar result was observed when we determined IL-6-induced expression levels of phosphorylated STAT3 following irradiation. Next, STAT3 was inhibited in SW480 and SW837 using siRNA, shRNA and the small-molecule inhibitor STATTIC. Successful silencing and inhibition of phosphorylation was confirmed using Western blot analysis and a luciferase reporter assay. RNAi-mediated silencing as well as STATTIC treatment resulted in significantly decreased clonogenic survival following exposure to 3 µM of 5-FU and irradiation in a dose-dependent manner, with dose-modifying factors of 1.3–2.5 at a surviving fraction of 0.37. Finally, STAT3 inhibition led to a profound CT/RT-sensitization in a subcutaneous xenograft model, with a significantly delayed tumor regrowth in STATTIC-treated mice compared with control animals. These results highlight a potential role of STAT3 in mediating treatment resistance and provide first proof of concept that STAT3 represents a promising novel molecular target for sensitizing resistant rectal cancers to CT/RT.
Abstract
What's new?
A considerable percentage of rectal cancers are resistant to preoperative chemoradiotherapy, which exposes patients to the potential side effects of both irradiation and chemotherapy without clear benefits. In this study, IL-6-stimulated expression levels of phosphorylated STAT3 were remarkably higher in chemoradiotherapy-resistant colorectal cancer cell lines. RNAi- and small molecule-mediated STAT3 inhibition sensitized to chemoradiotherapy in vitro in a dose-dependent manner, which led to a profound chemoradiotherapy-sensitization in a subcutaneous xenograft model. These results highlight a potential role of STAT3 in treatment resistance, and provide first proof of concept that STAT3 represents a promising novel molecular target for sensitizing resistant rectal cancers to chemoradiotherapy.
Supporting Information
Additional Supporting Information may be found in the online version of this article.
| Filename | Description |
|---|---|
| ijc28429-sup-0001-suppfig1.tif30.5 MB | Supplementary Figure S1: Total STAT3 and pSTAT3Tyr705 expression in 12 colorectal cancer (CRC) cell lines after irradiation. A-L, Cell lines were irradiated with 6 Gy of X-rays, and whole-cell lysates were obtained at the indicated time points (0.5, 1, 3, 6, 24 hours) after irradiation (without stimulation with IL-6) for Western blot analysis. None of the cell lines showed increasing protein levels of either pSTAT3Tyr705 or total STAT3. |
| ijc28429-sup-0002-suppfig2.tif9.2 MB | Supplementary Figure S2: Cellular viability of SW480 and SW837 cells following RNAi against STAT3. A and B, 3,000 SW480 (left panel) or 6,000 cells SW837 (right panel) were transfected with two different siRNAs targeting STAT3, or a negative-control siRNA (siNEG). Ninety-six hours of transfection, cellular viability was determined using the CellTiter-Blue® reagent (without stimulation with IL-6). Cellular viability was not significantly affected following siRNA-mediated silencing of STAT3. |
| ijc28429-sup-0003-suppfig3.tif12.7 MB | Supplementary Figure S3: Dose-response experiments to identify optimal concentrations of the STAT3 inhibitor STATTIC. A and B, Serum starved SW480 or SW837 cells were treated with DMSO or the indicated concentrations of STATTIC (SW480: 1, 2.5, 5, and 10µM; SW837: 1, 5, 10, and 20µM) for 30 minutes. Next, STATTIC was washed out, and cells were stimulated with 100ng/ml IL-6 for 30 minutes, followed by whole protein harvest for Western blot analysis. Increasing inhibitor concentrations led to a dose-dependent decrease of pSTAT3Tyr705 levels. Based on these results, further experiments were performed with 2.5µM and 10µM of STATTIC in SW480, and with 5µM and 20µM in SW837. Each experiment was independently repeated three times, and one representative blot is shown. |
| ijc28429-sup-0004-suppfig4.tif32.6 MB | Supplementary Figure S4: Establishment of doxycycline-inducible stable single-cell clone (scc) populations in SW480. A-C, A negative-control population (shNEG) and six single-cell clones, three from each of the two vectors, expressing an shRNA plasmid targeting STAT3, were established. Using FACS analysis, unstimulated shNEG and single-cell clone populations showed only faint signals of red fluorescence (left panel), while TurboRFP expression was strong 120 hours after incubation with 1 µg/ml doxycycline (right panel). All experiments were independently performed three times and showed similar results. |
| ijc28429-sup-0005-suppfig5.tif25.7 MB | Supplementary Figure S5: In the absence of chemoradiotherapy, STATTIC-treatment of SW837 xenografts in nude mice showed no differences in tumor growth and survival compared to DMSO-treatment. A, Mice were treated as indicated. Two million SW837 cells were subcutaneously injected in 100µl sterile cell culture medium into the right flank, and tumors were grown until they reached a volume of 400 – 500 mm3. Two groups of mice were treated once daily by intra-tumoral injections of either 23% DMSO (n=8) or 10mg/kg STATTIC (n=11) at the indicated time points (black arrows). Tumor volume and body weight were measured thrice weekly, and mice were sacrificed when the tumor volume exceeded 900 mm3 (start volume ×2). B, In both groups, tumor volume increased steadily over the whole time of injection, and STATTIC-treated mice showed no significant differences in tumor volume increase compared with DMSO-treated mice. C, In both groups, body weight was stable during the injections, and no significant differences could be detected. D, For tumor growth, documentation pictures were taken once a week. In both groups, tumor volumes increased at the same rate, and no differences were detected between DMSO-treated mice (left panel) and STATTIC-treated mice (right panel). E, Kaplan-Meier curves showed no significant survival differences between both groups. |
| ijc28429-sup-0006-supptable1.doc36.5 KB | Supplementary Table S1: Sequences for RT-PCR primers, siRNAs and shRNAs. |
| ijc28429-sup-0007-supptable2.doc38.5 KB | Supplementary Table S2: Antibodies and application specifications. |
| ijc28429-sup-0008-supptable3.doc40 KB | Supplementary Table S3: Survival variables α and β, and dose-modifying factors (DMF) at 37% survival. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1Yu H, Jove R. The STATs of cancer—new molecular targets come of age. Nat Rev Cancer 2004; 4: 97–105.
- 2Haura EB, Turkson J, Jove R. Mechanisms of disease: insights into the emerging role of signal transducers and activators of transcription in cancer. Nat Clin Pract Oncol 2005; 2: 315–24.
- 3Bromberg JF, Wrzeszczynska MH, Devgan G, et al. Stat3 as an oncogene. Cell 1999; 98: 295–303.
- 4Darnell JE, Jr. STATs and gene regulation. Science 1997; 277: 1630–5.
- 5Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat Rev Immunol 2007; 7: 41–51.
- 6Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer 2009; 9: 798–809.
- 7Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 2010; 140: 883–99.
- 8Sansone P, Bromberg J. Targeting the interleukin-6/Jak/stat pathway in human malignancies. J Clin Oncol 2012; 30: 1005–14.
- 9Spitzner M, Emons G, Kramer F, et al. A gene expression signature for chemoradiosensitivity of colorectal cancer cells. Int J Radiat Oncol Biol Phys 2010; 78: 1184–92.
- 10Cunningham D, Atkin W, Lenz HJ, et al. Colorectal cancer. Lancet 2010; 375: 1030–47.
- 11Rodel C, Hofheinz R, Liersch T. Rectal cancer: state of the art in 2012. Curr Opin Oncol 2012; 24: 441–7.
- 12Grade M, Hummon AB, Camps J, et al. A genomic strategy for the functional validation of colorectal cancer genes identifies potential therapeutic targets. Int J Cancer 2011; 128: 1069–79.
- 13Schust J, Sperl B, Hollis A, et al. Stattic: a small-molecule inhibitor of STAT3 activation and dimerization. Chem Biol 2006; 13: 1235–42.
- 14Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001; 25: 402–8.
- 15Kendziorra E, Ahlborn K, Spitzner M, et al. Silencing of the Wnt transcription factor TCF4 sensitizes colorectal cancer cells to (chemo-) radiotherapy. Carcinogenesis 2011; 32: 1824–31.
- 16Scuto A, Kujawski M, Kowolik C, et al. STAT3 inhibition is a therapeutic strategy for ABC-like diffuse large B-cell lymphoma. Cancer Res 2011; 71: 3182–8.
- 17Lin Q, Lai R, Chirieac LR, et al. Constitutive activation of JAK3/STAT3 in colon carcinoma tumors and cell lines: inhibition of JAK3/STAT3 signaling induces apoptosis and cell cycle arrest of colon carcinoma cells. Am J Pathol 2005; 167: 969–80.
- 18Kusaba T, Nakayama T, Yamazumi K, et al. Expression of p-STAT3 in human colorectal adenocarcinoma and adenoma; correlation with clinicopathological factors. J Clin Pathol 2005; 58: 833–8.
- 19Corvinus FM, Orth C, Moriggl R, et al. Persistent STAT3 activation in colon cancer is associated with enhanced cell proliferation and tumor growth. Neoplasia 2005; 7: 545–55.
- 20Morikawa T, Baba Y, Yamauchi M, et al. STAT3 expression, molecular features, inflammation patterns, and prognosis in a database of 724 colorectal cancers. Clin Cancer Res 2011; 17: 1452–62.
- 21Monnien F, Zaki H, Borg C, et al. Prognostic value of phosphorylated STAT3 in advanced rectal cancer: a study from 104 French patients included in the EORTC 22921 trial. J Clin Pathol 2010; 63: 873–8.
- 22Klampfer L. The role of signal transducers and activators of transcription in colon cancer. Front Biosci 2008; 13: 2888–99.
- 23Waldner MJ, Foersch S, Neurath MF. Interleukin-6—a key regulator of colorectal cancer development. Int J Biol Sci 2012; 8: 1248–53.
- 24Atreya R, Neurath MF. Signaling molecules: the pathogenic role of the IL-6/STAT-3 trans signaling pathway in intestinal inflammation and in colonic cancer. Curr Drug Targets 2008; 9: 369–74.
- 25Rose-John S, Mitsuyama K, Matsumoto S, et al. Interleukin-6 trans-signaling and colonic cancer associated with inflammatory bowel disease. Curr Pharm Des 2009; 15: 2095–103.
- 26Grade M, Hormann P, Becker S, et al. Gene expression profiling reveals a massive, aneuploidy-dependent transcriptional deregulation and distinct differences between lymph node-negative and lymph node-positive colon carcinomas. Cancer Res 2007; 67: 41–56.
- 27Camps J, Nguyen QT, Padilla-Nash HM, et al. Integrative genomics reveals mechanisms of copy number alterations responsible for transcriptional deregulation in colorectal cancer. Genes Chromosomes Cancer 2009; 48: 1002–17.
- 28Camps J, Pitt JJ, Emons G, et al. Genetic amplication of the NOTCH modulator LNX2 upregulates the WNT/beta-catenin pathway in colorectal cancer. Cancer Res 2013; 73: 2003–13.
- 29Network CGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature 2012; 487: 330–7.
- 30Tsareva SA, Moriggl R, Corvinus FM, et al. Signal transducer and activator of transcription 3 activation promotes invasive growth of colon carcinomas through matrix metalloproteinase induction. Neoplasia 2007; 9: 279–91.
- 31Zugowski C, Lieder F, Muller A, et al. STAT3 controls matrix metalloproteinase-1 expression in colon carcinoma cells by both direct and AP-1-mediated interaction with the MMP-1 promoter. Biol Chem 2011; 392: 449–59.
- 32Suzuki A, Hanada T, Mitsuyama K, et al. CIS3/SOCS3/SSI3 plays a negative regulatory role in STAT3 activation and intestinal inflammation. J Exp Med 2001; 193: 471–81.
- 33Bollrath J, Phesse TJ, von Burstin VA, et al. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell 2009; 15: 91–102.
- 34Grivennikov S, Karin E, Terzic J, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 2009; 15: 103–13.
- 35Lin L, Liu Y, Li H, et al. Targeting colon cancer stem cells using a new curcumin analogue, GO-Y030. Br J Cancer 2011; 105: 212–20.
- 36Lin L, Liu A, Peng Z, et al. STAT3 is necessary for proliferation and survival in colon cancer-initiating cells. Cancer Res 2011; 71: 7226–37.
- 37Grade M, Wolff HA, Gaedcke J, et al. The molecular basis of chemoradiosensitivity in rectal cancer: implications for personalized therapies. Langenbecks Arch Surg 2012; 397: 543–55.
- 38Kim KW, Mutter RW, Cao C, et al. Inhibition of signal transducer and activator of transcription 3 activity results in down-regulation of Survivin following irradiation. Mol Cancer Ther 2006; 5: 2659–65.
- 39Bonner JA, Trummell HQ, Willey CD, et al. Inhibition of STAT-3 results in radiosensitization of human squamous cell carcinoma. Radiother Oncol 2009; 92: 339–44.
- 40Gao L, Li F, Dong B, et al. Inhibition of STAT3 and ErbB2 suppresses tumor growth, enhances radiosensitivity, and induces mitochondria-dependent apoptosis in glioma cells. Int J Radiat Oncol Biol Phys 2010; 77: 1223–31.
- 41Chen YW, Chen KH, Huang PI, et al. Cucurbitacin I suppressed stem-like property and enhanced radiation-induced apoptosis in head and neck squamous carcinoma—derived CD44(+)ALDH1(+) cells. Mol Cancer Ther 2010; 9: 2879–92.
- 42Yang YP, Chang YL, Huang PI, et al. Resveratrol suppresses tumorigenicity and enhances radiosensitivity in primary glioblastoma tumor initiating cells by inhibiting the STAT3 axis. J Cell Physiol 2012; 227: 976–93.
- 43Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell 2012; 21: 309–22.
- 44Swartz MA, Iida N, Roberts EW, et al. Tumor microenvironment complexity: emerging roles in cancer therapy. Cancer Res 2012; 72: 2473–80.
- 45Mankan AK, Greten FR. Inhibiting signal transducer and activator of transcription 3: rationality and rationale design of inhibitors. Expert Opin Investig Drugs 2011; 20: 1263–75.
- 46Wang T, Niu G, Kortylewski M, et al. Regulation of the innate and adaptive immune responses by Stat-3 signaling in tumor cells. Nat Med 2004; 10: 48–54.
- 47Kortylewski M, Kujawski M, Wang T, et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat Med 2005; 11: 1314–21.
- 48Herrmann A, Kortylewski M, Kujawski M, et al. Targeting Stat3 in the myeloid compartment drastically improves the in vivo antitumor functions of adoptively transferred T cells. Cancer Res 2010; 70: 7455–64.
- 49Ishihara S, Watanabe T, Kiyomatsu T, et al. Prognostic significance of response to preoperative radiotherapy, lymph node metastasis, and CEA level in patients undergoing total mesorectal excision of rectal cancer. Int J Colorectal Dis 2010; 25: 1417–25.
- 50Chang GJ, Rodriguez-Bigas MA, Eng C, et al. Lymph node status after neoadjuvant radiotherapy for rectal cancer is a biologic predictor of outcome. Cancer 2009; 115: 5432–40.