Epidemiology and predictors of multimorbidity in Kharameh cohort study: A population-based cross-sectional study in southern Iran
[Correction added on 20 December 2022, after first online publication: The fourth author's name was corrected in this version.]
Abstract
Background and Aim
Multimorbidity is one of the problems and concerns of public health. The aim of this study was to estimate the prevalence and identify the risk factors associated with multimorbidity based on the data of the Kherameh cohort study.
Methods
This cross-sectional study was performed on 10,663 individuals aged 40–70 years in the south of Iran in 2015 to 2017. Demographic and behavioral characteristics were investigated. Multimorbidity was defined as the coexistence of two or more of two chronic diseases in a person. In this study, the prevalence of multimorbidity was calculated. Logistic regression was used to identify the predictors of multimorbidity.
Results
The prevalence of multimorbidity was 24.4%. The age-standardized prevalence rate was 18.01% in males and 29.6% in females. The most common underlying diseases were gastroesophageal reflux disease with hypertension (33.5%). Multiple logistic regression results showed that the age of 45–55 years (adjusted odds ratio [ORadj]] = 1.22, 95% confidence interval [CI], 1.07–1.38), age of over 55 years (ORadj = 1.21, 95% CI, 1.06–1.37), obesity (ORadj = 3.65, 95% CI, 2.55–5.24), and overweight (ORadj = 2.92, 95% CI, 2.05–4.14) were the risk factors of multimorbidity. Also, subjects with high socioeconomic status (ORadj = 1.27, 95% CI, 1.1–1.45) and very high level of socioeconomic status (ORadj = 1.53, 95% CI, 1.31–1.79) had a higher chance of having multimorbidity. The high level of education, alcohol consumption, having job, and high physical activity had a protective role against it.
Conclusion
The prevalence of multimorbidity was relatively high in the study area. According to the results of our study, age, obesity, and overweight had an important effect on multimorbidity. Therefore, determining interventional strategies for weight loss and control and treatment of chronic diseases, especially in the elderly, is very useful.
1 INTRODUCTION
Multimorbidity is a condition in which a person suffers from two or more chronic diseases at the same time.1-3 Multimorbidity leads to increased mortality, decreased quality of life, overuse of medical drugs, frequent hospitalizations, and increased use of care services.,4-6 thus imposing a heavy financial burden on the individual, the community, and the health care system.7 For this reason, multimorbidity has become an important public health concern8 which has led to challenges in the public health field.9, 10 In various studies, older age, sex, smoking and alcohol consumption, opium use, low income, obesity, overweight, and lack of physical activity have been introduced as risk factors for multimorbidity.7, 11
In recent years, progress in the medical situation in Iran as well as increasing life expectancy has led to the transformation of acute and deadly diseases into chronic diseases,12 which are the main cause of multimorbidity.9 In this regard, World Health Organization (WHO) reported that chronic diseases kill 38 million people annually.1
Although the prevalence of multimorbidity increases with age,2 it can be seen at all ages.13 In various studies, the prevalence of multimorbidity is reported between 13.1% and 71.8%.9 A cross-sectional study revealed a 60% prevalence of multimorbidity.14 One meta-analysis of 70 studies reported an overall multimorbidity prevalence of 31%.15 In the Netherlands, the prevalence of multimorbidity in men and women was 33.6% and 35.9%, respectively.16 Also, in Switzerland, the overall prevalence of multimorbidity was estimated to be between 20% and 30% in all age groups.17 Also, the prevalence of multimorbidity in Golestan, Iran, was reported to be 19.4%,12 and in another study in the northwest of Iran, it was reported 15.75%.7 Despite recent studies showing an increase in the prevalence of multimorbidity in the world, especially in developing countries, so far only few studies have been conducted in developing countries5; therefore, still many questions remain in this regard.11 Due to the complexity of treatment management of multimorbidity, we need to increase knowledge and awareness about the underlying factors of multimorbidity, its trend in society, and the costs that it imposes on society and individuals. In this way, health policymakers can take measures to allocate financial and medical resources, as well as develop prevention and treatment guidelines for the treatment of these people. For this purpose, this study was conducted to investigate the prevalence and risk factors for multimorbidity in adults in the city of Kharameh in the south of Iran.
2 METHODS
2.1 Study design and population
The present cross-sectional, analytical study was conducted using baseline data from the Kharameh cohort study, with 10,663 adult individuals aged from 40 to 70 years old. Kharameh cohort study is part of the Prospective Epidemiological Studies in Iran (PERSIAN). The Persian Cohort Study was launched in 2014 in 18 geographical areas in Iran to determine the prevalence and risk factors of noncommunicable diseases. Kharameh is one of the southern cities in Fars province with a population of 61,580 people. Other details related to the PERSIAN cohort study design have been previously published.18
Initially, all people aged 40–70 years were invited to participate in the study, and then those who signed the informed consent forms were enrolled in the study (the response rate for participation in the study was 97. 3%).
2.1.1 Inclusion and exclusion criteria
Inclusion criteria were age between 40 and 70 years, residents of Kharameh city for at least 9 months and Iranian nationality. Exclusion criteria also included mental disorders such as mental retardation and any illness in the acute phase that is not treated. Another exclusion criterion was unwillingness to participate in the study.
2.1.2 Data collection
For this study, variables related to demographic characteristics and the chronic disease status of the participants were examined. All information of the participants to this study was collected using standard questionnaires of the Persian cohort study that had previously been validated. Data were collected through face-to-face interviews by trained staff. Clinical information of individuals was also reviewed by trained physicians. Further information regarding the Persian cohort study has been presented in other studies.18
Variables related to demographic characteristics in this study included age, sex, marital status, education level, employment, living place, socioeconomic status (SES), physical activity, body mass index (BMI), smoking, alcohol consumption, and hookah use. Hookah is a traditional method of smoking tobacco, especially in the Eastern Mediterranean Region (EMR). The hookah is also known as gouza, waterpipe, narghile, shisha, or hubble-bubble. It is usually referred to as Ghalyan in Iran.19, 20 The SES index was also calculated using principal component analysis; using variables related to the individuals' financial assets, we classified the SES into four categories: low, moderate, high, and very high. Also, the Metabolic Equivalent of Task (MET) index was calculated to the physical activity. In this way, we converted physical activity into the amount of energy consumption. One MET is equal to one kilocalorie of energy consumed per kilogram of body weight at rest.
Individuals' weight was measured with light clothing without shoes using the SECA scale (made in Germany), and height was measured using a standard measuring tape. BMI was calculated by dividing weight (kg) by height (m2), and individuals were divided into four categories: underweight (BMI < 18.5 kg/m2), normal weight (BMI: 18.5–24.9 kg/m2), overweight (BMI: 25–29.9 kg/m2), and obese (BMI ≥ 30 kg/m2). Blood pressure was measured from the individual's right arm after a 5-min rest in sitting position using a standard calibrated sphygmomanometer (Reister Model). Blood pressure was measured twice from each person with a minimum interval of 10 min and their mean was recorded.21
2.2 Multimorbidity definition
In our study, multimorbidity refers to the coexistence of two or more chronic diseases in a person at the same time. Chronic diseases considered in this study were cardiovascular disease (CVD), diabetes mellitus, hypertension, chronic obstructive pulmonary diseases (COPD), chronic kidney disease (CKD), liver disease, neurologic diseases, cancer, and chronic gastroesophageal reflux disease (GERD). GERD is a chronic condition that occurs when the reflux of the contents of the stomach causes troublesome symptoms.21 The history of chronic diseases (such as diabetes, blood pressure, CVDs, etc.) was recorded based on their personal self-report and review of their medical records by a physician. In the absence of sufficient medical documents or lack of confidence in people's reporting, diagnostic measures such as laboratory tests, radiology, ultrasound, and so on, were performed for people with the doctor's recommendation. Finally, all medical documents were checked by two specialist doctors to confirm the disease.
2.3 Statistical analysis
Frequency and percentage were used to describe qualitative variables. χ2 and Fischer's exact test were performed to evaluate the difference between the levels of qualitative variables in the two groups with and without multimorbid. Moreover, the age-standardized prevalence rate (ASPR) of multimorbidity was determined using the standard Asian population.22 Dependent variable in this study was multimorbidity. Based on the definition of multimorbidity, people are divided into two categories. People with and without multimorbidity. Simple logistic regression was used to identify the predictors of multimorbidity and calculate the odds ratio with a 95% confidence interval (CI). To control the confounding factors and calculate the adjusted odds ratio, multiple logistic regression was used. The significance level was considered less than 0.05 for all tests and all analyses were performed using Stata crop Inc version 13 (College Station).
3 RESULTS
The present study was performed on 10,663 adults aged 40–70 years. Mean age of the participants was calculated to be 52.15 ± 8.5 years, and the majority of them were female (55.7%), married (89%), illiterate (52.4%), dwellers of rural areas (64.1%), and overweight (41.7%). Other descriptive characteristics of the participants are shown by in Table 1.
| Variable | Class | Total | Multimorbidity in female | p Value | Multimorbidity in male | |||
|---|---|---|---|---|---|---|---|---|
| No (N = 4182) | Yes (N = 1762) | No (N = 3869) | Yes (N = 850) | p Value | ||||
| Age (years) | ≤45 | 2566 (24.06) | 910 (21.76) | 347 (19.69) | 0.204 | 1138 (29.41) | 171 (20.12) | 0.0001 |
| 45–55 | 4177 (39.17) | 1484 (35.49) | 643 (36.49) | 1667 (43.09) | 383 (45.06) | |||
| ≥55 | 3920 (36.76) | 1788 (42.75) | 772 (43.81) | 1064 (27.5) | 296 (34.82) | |||
| Living place | Rural | 6831 (64.1) | 2805 (67) | 1105 (62.7) | 0.001 | 2402 (62.1) | 519 (61.06) | 0.578 |
| Urban | 3832 (35.9) | 1377 (33) | 657 (37.3) | 1467 (37.9) | 331 (38.94) | |||
| Marital status | Unmarried | 176 (1.65) | 134 (3.2) | 18 (1.02) | 0.0001 | 19 (0.49) | 5 (0.59) | 0.762a |
| Married | 9492 (89) | 3499 (83.67) | 1334 (75.71) | 3819 (98.71) | 840 (98.8) | |||
| Widow | 995 (9.33) | 549 (13.13) | 410 (23.27.02) | 31 (0.8) | 5 (0.59) | |||
| Education level | Illiterate | 5587 (52.4) | 2469 (59.04) | 1286 (72.99) | 0.0001 | 1458 (37.68) | 374 (44) | 0.0001 |
| Primary school | 2676 (25.1) | 1087 (25.99) | 339 (19.24) | 1069 (27.63) | 181 (21.29) | |||
| Middle school | 1136 (10.65) | 328 (7.84) | 73 (4.14) | 630 (16.28) | 105 (12.35) | |||
| High school | 702 (6.58) | 160 (3.83) | 39 (2.21) | 394 (10.18) | 109 (12.82) | |||
| University | 562 (5.27) | 138 (3.3) | 25 (1.42) | 318 (8.22) | 81 (9.53) | |||
| Employment | No | 5147 (48.3) | 2977 (71.19) | 1464 (83.1) | 0.0001 | 470 (12.15) | 236 (27.76) | 0.0001 |
| Yes | 5516 (51.7) | 1205 (28.81) | 298 (16.9) | 3399 (87.85) | 614 (72.24) | |||
| Socioeconomic status | Low | 2667 (25.01) | 1249 (29.87) | 452 (25.65) | 0.001 | 823 (21.27) | 143 (16.82) | 0.0001 |
| Moderate | 2977 (27.92) | 1342 (32.09) | 603 (34.22) | 849 (21.94) | 183 (21.53) | |||
| High | 2539 (23.81) | 1095 (26.18) | 452 (25.65) | 804 (20.78) | 188 (22.12) | |||
| Very high | 2480 (23.26) | 496 (11.86) | 255 (14.47) | 1393 (36) | 336 (39.53) | |||
| Physical activity | Light | 2670 (25.04) | 732 (17.5) | 533 (30.25) | 0.0001 | 1048 (27.09) | 357 (42) | 0.0001 |
| Moderate | 2666 (25.0) | 1359 (32.5) | 533 (30.25) | 637 (16.46) | 137 (16.12) | |||
| High | 2664 (24.98) | 1455 (34.8) | 522 (29.63) | 576 (14.89) | 111 (13.06) | |||
| Sever | 2663 (24.97) | 636 (15.2) | 174 (9.88) | 1608 (41.56) | 245 (28.82) | |||
| BMIb | Underweight | 413 (3.87) | 85 (2.03) | 16 (0.91) | 0.0001 | 290 (7.5) | 22 (2.59) | 0.0001 |
| Normal | 3883 (36.42) | 1217 (29.1) | 388 (22.02) | 1957 (50.58) | 321 (37.76) | |||
| Overweight | 4450 (41.73) | 1889 (45.17) | 796 (45.18) | 1360 (35.15) | 405 (47.65) | |||
| Obese | 1917 (17.98) | 991 (23.7) | 562 (31.9) | 262 (6.77) | 102 (12) | |||
| Smoking | No | 7960 (74.6) | 4052 (96.9) | 1689 (95.8) | 0.045 | 1786 (46.1) | 433 (50.9) | 0.011 |
| Yes | 2703 (25.4) | 130 (3.1) | 73 (4.2) | 2083 (53.9) | 417 (49.1) | |||
| Use hookah | No | 10,115 (94.9) | 4125 (98.64) | 1736 (98.52) | 0.735 | 3489 (90.15) | 765 (90) | 0.874 |
| Yes | 548 (5.1) | 57 (1.36) | 26 (1.48) | 380 (9.82) | 85 (10) | |||
| Alcohol consumption | No | 10,095 (94.7) | 4178 (99.9) | 1760 (99.9) | 0.999a | 3372 (87.15) | 785 (92.4) | 0.0001 |
| Yes | 568 (5.3) | 4 (0.1) | 2 (0.1) | 497 (12.85) | 65 (7.6) | |||
- Abbreviation: BMI, body mass index.
- a Fischer's exact test.
- b Underweight (BMI < 18.5 kg/m2), normal (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI > 30 kg/m2).
The crude prevalence and ASPR of multimorbidity were 24.4% (95% CI: 23.6–25.3) and 24.4% (95% CI: 24.1–24.9), respectively. Besides, the ASPR was 18.01% in males (95% CI: 17.8%–18.2%) and 29.6% in females (95% CI: 29.3%–29.9%) (Table 2).
| 95% CI | 95% CI | |||||
|---|---|---|---|---|---|---|
| Crude | Lower | Upper | ASPR | Lower | Upper | |
| Both sexes | 24.4 | 23.6 | 25.3 | 24.4 | 24.1 | 24.9 |
| Male | 18 | 16.92 | 19.1 | 18.01 | 17.8 | 18.2 |
| Female | 29.6 | 28.4 | 30.8 | 29.6 | 29.3 | 29.9 |
- Abbreviations: ASPR, age-standardized prevalence rate; CI, confidence interval.
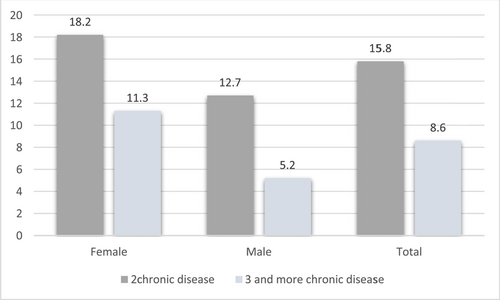
Also, we calculated the prevalence of multiple diseases based on the number of simultaneous chronic diseases by gender and the results showed that approximately 16% of the participants had two simultaneous chronic diseases and 8.6% had three or more. 12.7% of men and 18.25% of women had two chronic diseases simultaneously. In addition, 5.2% of men and 11.35% of women had three or more chronic diseases (Figure 1).
The most common cases of multimorbidity were the simultaneous presence of GERD with hypertension (33.5%) and GERD with diabetes mellitus (29.3%).
The result of the χ2 test showed that there was a statistically significant difference between the status of multimorbidity in different age groups, education levels, job statuses, SES levels, physical activity levels, smoking, alcohol consumption, and BMI in men (p < 0.0001). Also, there was a statistically significant difference between the status of multimorbidity in the place of residence, education level, marital status, job status, BMI, smoking, and physical activity level in women (p < 0.05). Other cases are reported in Table 1.
The results of simple logistic regression to identify multimorbidity predictor variables showed that age, female sex, obesity and overweight, urbanization, marital status, and high level of SES had a statistically significant relationship with the increase in chances of multimorbidity. Moreover, having a job, high levels of physical activity, cigarette smoking, consumption of alcohol, and hookah reduced the chances of multimorbidity (Table 3).
| Variable | Simple logistic regression | Multiple logistic regression | |||
|---|---|---|---|---|---|
| OR (95% CI) | p Value | ORadj (95% CI) | p Value | ||
| Age (year) | ≤45 | 1 | 1 | ||
| 45–55 | 1.28 (1.14–1.45) | 0.0001 | 1.22 (1.07–1.38) | 0.002 | |
| ≥55 | 1.48 (1.31–1.66) | 0.0001 | 1.21 (1.06–1.37) | 0.003 | |
| Sex | Male | 1 | 1 | ||
| Female | 1.91 (1.74–2.14) | 0.0001 | 1.01 (0.87–1.18) | 0.836 | |
| Marital status | Unmarried | 1 | 1 | ||
| Married | 1.97 (1.27–3.07) | 0.002 | 1.94 (1.23–3.06) | 0.004 | |
| Widow | 4.75 (3.01–7.51) | 0.0003 | 3.1 (1.98–5.06) | 0.0001 | |
| Education level | Illiterate | 1 | 1 | ||
| Primary school | 0.57 (0.51–0.63) | 0.0001 | 0.57 (0.51–0.65) | 0.0001 | |
| Secondary school | 0.43 (0.37–0.52) | 0.0001 | 0.48 (0.4–0.58) | 0.0001 | |
| High school | 0.63 (0.52–0.76) | 0.0001 | 0.69 (0.56–0.85) | 0.0001 | |
| University | 0.54 (0.44–0.68) | 0.0001 | 0.56 (0.44–0.72) | 0.0001 | |
| Employment | No | 1 | 1 | ||
| Yes | 0.4 (0.36–0.44) | 0.0001 | 0.57 (0.5–0.65) | 0.0001 | |
| Socioeconomic status | Low | 1 | 1 | ||
| Moderate | 1.2 (1.1–1.4) | 0.0001 | 1.26 (1.11–1.44) | 0.0001 | |
| High | 1.17 (1.03–1.33) | 0.014 | 1.27 (1.1–1.45) | 0.001 | |
| Very high | 1.08 (0.95–1.24) | 0.195 | 1.53 (1.3–1.79) | 0.0001 | |
| Physical activity | Light | 1 | 1 | ||
| Moderate | 0.67 (0.59–0.75) | 0.0001 | 0.67 (0.59–0.77) | 0.0001 | |
| High | 0.62 (0.55–0.7) | 0.0001 | 0.66 (0.58–0.76) | 0.0001 | |
| Sever | 0.37 (0.32–0.42) | 0.0001 | 0.59 (0.51–0.69) | 0.0001 | |
| BMIa | Underweight | 1 | 1 | ||
| Normal | 2.2 (1.56–3.1) | 0.0001 | 1.96 (1.38–2.79) | 0.0001 | |
| Overweight | 3.64 (2.59–5.12) | 0.0001 | 2.92 (2.05–4.14) | 0.0001 | |
| Obese | 5.22 (3.69–7.39) | 0.0001 | 3.65 (2.55–5.24) | 0.0001 | |
| Living place | Rural | 1 | 1 | 0.113 | |
| Urban | 1.11 (1.01–1.22) | 0.021 | 1.08 (0.98–1.2) | ||
| Alcohol consumption | No | 1 | 1 | 0.001 | |
| Yes | 0.39 (0.3–0.5) | 0.0001 | 0.62 (0.47–0.83) | ||
| Smoking | No | 1 | 1 | 0.999 | |
| Yes | 0.6(0.54–0.67) | 0.0001 | 1.006 (0.87–1.16) | ||
| Use hookah | No | 1 | 1 | 0.162 | |
| Yes | 0.77 (0.62–0.95) | 0.018 | 1.18 (0.93–1.49) | ||
- Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio.
- a Underweight (BMI < 18.5 kg/m2), normal (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI > 30 kg/m2).
We used multiple logistic regression to control the confounders and calculate the adjusted odds ratio. All variables with p-value less than 0.2 were included in multiple regression. The results showed that the chance of developing multimorbidity in people over 55 years was 1.21 (95% CI: 1.06–1.37) times and in people aged 45–55, 1.22 (95% CI: 1.07–1.38) times higher than the participants under 45 years old. People with obesity were 3.65 times (95% CI: 2.55–5.24) and overweight people 2.92 (5% CI: 2.05–4.14) times more likely to develop multimorbidity in comparison to normal-weight people, respectively. Married people were 1.94 (95% CI: 1.23–3.06) times more likely than unmarried ones to have multimorbidity; also, those with a high SES were 1.27, times (95% CI: 11–1.45) and those with very high SES 1.53 times (95% CI: 1.31–1.79) more likely to developed multimorbidity than those with a low SES group. It is also worth noting that variables such as high school and university education, employment, alcohol consumption, and high- and medium-level physical activity had a protective role against multimorbidity. After control of the confounders, we observed no significant relationship between gender, smoking, and hookah with multimorbidity (Table 3).
4 DISCUSSION
Multimorbidity is one of the most important public health issues that has become a public health concern due to the increasing incidence of noncommunicable diseases. However, not many studies have been conducted in this regard in Iran so far. This study was performed on 10,663 people aged 40–70 years old. The prevalence of multimorbidity in the population under our study was 24.4%, which was higher than that of multimorbidity(19.4%) in the Golestan study,12 and lower than that reported (36.6%) in the Kurdish ethnic study in Iran.9 It was also similar to the prevalence in China (24.7%),11 and Burkina-Faso (22.8%).5 Other studies have reported a prevalence of multimorbidity between 14.4% and 67.3%.3, 16, 23-25 The reason for these differences can be such factors as age and sex composition of the population under study, lack of a definitive definition for multimorbidity, and, finally, how multimorbidity is calculated in different studies.
According to the results of this study, GERD along with hypertension (33.5%) followed by GERD along with diabetes (29.3%) were the chronic diseases most commonly seen together. However, the prevalence of GERD has been increasing in recent years in Iran,26 and hypertension is the main cause of mortality in more than 30% of the adult population.27 In the study conducted in Golestan, Iran, GERD along with CVDs (52%) was identified as the most common multimorbidity.12 Furthermore, in other studies, hypertension along with hyperlipidemia,12, 23, 28 and in southern Argentina, hypertension along with diabetes were the most common multimorbidities. This difference can be due to the cultural factors of their region and lifestyle.
Our study showed that the prevalence of multimorbidity increased with age, which is consistent with the findings of other studies.3, 10, 25, 29 Given the growing trend of aging around the world, especially in developing countries, this issue can be very worrying. Studies conducted in Iran to examine the aging trend of the population have shown that the rate of fertility in Iran has had a sharp decline compared to previous decades. They also predict that in 2050, 31% of the population of Iran, equivalent to 29 million people, would have over 60 years of age and 22% will be 65 years old,30 this is a striking alarm for health policymakers in Iran because as the population ages, the prevalence of chronic diseases will increase due to biological changes in the body, imposing a heavy burden on the individual and the society.
According to the results of our study, overweight and obesity were the risk factor of multimorbidity, which was consistent with the results of many other studies,11, 16, 17 while another study has not shown an association between obesity and multimorbidity.9 In a study carried out in New Zealand, obesity was introduced as a protective factor.7 The reason for these differences can be the people under study. However, it should be noted that obesity has long been recognized as an important risk factor for chronic diseases.31-33 A meta-analysis study in 2018 found the prevalence of obesity in Iranian adults to be 21.4%,34 and another study reported an overall prevalence of obesity in Iran to be 26.5%.35 In our study, about 50% of people were overweight or obese. Due to the increase in inactive lifestyles in society, the rise in the prevalence of obesity will continue.
It should be noted that the results of this study, similar to some other studies12, 17 have shown that increasing the level of physical activity is a protective factor against multimorbidity. Contrary to our study, Hudon et al.36 stated that there was no relationship between the level of physical activity and multimorbidity. In another study conducted in Iran on 30,541 adults, the prevalence of insufficient physical activity was 54.7%.37 This in itself indicates the risk for people; hence, the necessary arrangements should be made to educate the culture and increase awareness about the benefits of physical activity and obesity prevention.
Our study, similar to some other studies, has shown that a high level of education reduces the risk of multimorbidity.10, 12, 38 This can be due to the higher awareness of these people as well as their greater sensitivity to follow-up and health care.
In our study, being married also increased the chances of developing multimorbidity. This was consistent with the results of Kurdish studies in Iran,9 but no correlation was found with the Golestan study12 though in the Burkina Faso study, single people were at higher risk.5 These differences can be due to cultural conditions, stress levels in society, and people's lives and social conditions.
Although in many studies around the world, multimorbidity was higher among women,1, 23, 38 in our study, similar to other studies, no difference between men and women was observed.39, 40 This may be because the male-to-female ratio in our studies was somewhat similar; also, due to the different prevalence of diseases in men and women, the type of diseases evaluated in different studies can affect these differences. However, we must keep in mind that women are always more likely to seek health care than men; therefore, their diseases are diagnosed earlier.
Based on the results of our study, multimorbidity has increased along with the increase in the level of SES, while in many other studies, unlike our study, the low level of SES was identified as a risk factor for multimorbidity41-44; these differences are due to social factors and different ways of classifying the SES in different studies. However, our study was conducted in a developing country that is facing lifestyle changes, including sedentary lifestyle and obesity. Also, people with high level of SES have better access to care services and are informed of their illness sooner.
Although alcohol consumption has been identified as a risk factor for chronic diseases,45-47 in our study as well as other studies a protective role has been shown.6, 7, 25 Sarkar and colleagues48 also observed that alcohol consumption played a protective role for multimorbidity, which was not statistically significant. In the study carried out by Mohammadian, alcohol consumption was introduced as a risk factor for multimorbidity in men49; however, some studies found no association between alcohol consumption and multimorbidity.10, 41 The reason for these differences is that the amount and duration of alcohol consumption have not been studied in the same way in all studies; also, due to religious and social factors in different countries, people may not respond honestly to this issue, and this will cause errors in the study estimates. Also, some people may have stopped taking it after suffering from a chronic disease. These contradictions indicate the need for more detailed studies, especially in relation to alcohol consumption and multimorbidity.
In our study, no significant relationship was observed between smoking cigarettes and hookah with multimorbidity. In a study conducted in Golestan, light smoking had a protective role,12 and in another study in Canada, this protective role was seen.6 However, some other studies have identified smoking as a risk factor for multimorbidity.11, 50 Quitting smoking to prevent the progression of the disease after the diagnosis in people can be the reason for this protective effect. Our study was cross-sectional research and did not examine smoking before the study.
5 LIMITATIONS
The prevalence of multimorbidity in this study is based on self-reports of individuals; as a result, some of the clinical information may not have been properly reported to interviewers. Therefore, we may witness under-reporting on some cases. In addition, we must keep in mind that this was a cross-sectional study and we could not correctly estimate the cause-and-effect relationship. In addition, we must keep in mind that there might be unknown confounding factors that affect the results of our study.
6 CONCLUSION
The prevalence of multimorbidity in the population under study was relatively high. Obesity, overweight, and high SES were the risk factors and physical activity reduced the risk of multimorbidity. Therefore, having a healthy lifestyle can reduce the risk of multimorbidity. These results indicate the need to prepare and implement basic strategies to prevent multimorbidity. It is also a warning to health policymakers to provide the necessary guidance to reduce the risk factors, especially in the young population.
AUTHOR CONTRIBUTIONS
Leila Moftakhar: Formal analysis; investigation; writing – review and editing. Ramin Rezaeianzadeh: Writing – original draft. Masoumeh Ghoddusi Johari: Supervision; writing – original draft. Seyed Vahid Hosseini: Writing – original draft. Abbas Rezaianzadeh: Methodology; writing – original draft.
ACKNOWLEDGMENTS
The authors are grateful to the officers and data management staff of kherameh cohort. Also, the authors would like to thank all the study participants who patiently cooperated with us. This research received no external funding.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The Kherameh cohort is part of the large Persian cohort study in Iran. PERSIAN Cohort Study is being performed in 18 geographical regions of Iran. PERSIAN Cohort Study was approved by the Ethics Committee of the Ministry of Health and Medical Education. The code of ethics and approval of the Kharamah cohort 7421. Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors. Also, informed consent was obtained from all participants in the study.
TRANSPARENCY STATEMENT
The lead author Masoumeh Ghoddusi Johari affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The datasets generated and analyzed during the current study are not publicly available due to data are not public, but are available from the corresponding author on reasonable request.




