Disease patterns and clinical outcomes of medical admissions at a tertiary hospital in Northern Tanzania: A retrospective observational study
Abstract
Background and Aims
The burden of noncommunicable diseases is increasing in developing countries and in settings with an existing communicable burden. The study aim was to identify the disease pattern, length of stay, and clinical outcome of medical admissions.
Methods
A retrospective observational study of patients admitted to medical wards between 1st July 2019 and 30th June 2020, excluding those admitted for chemotherapy. The outcome measures were the pattern of disease, length of stay, and clinical outcome.
Results
A total of 3930 patients were analyzed. A total of 53.5% were males, and 42.9% were aged 51–75 years, with a median age of 57 years (IQR 41–71). A total of 41.3% had health insurance, 21.7% died, and the median length of stay was 6 days (IQR 4–9). Cardiovascular diseases were the most common diagnosis (26.8%) on admission and cause of death (27.9%). The common causes of death were stroke (15.1%), chronic kidney disease (11.1%), and heart failure (9.0%). Noninsured patients had a high mortality risk (odds ratios [OR] 1.67, 95% confidence interval [CI] 1.42–1.96), which was also seen among patients aged more than 75 years (OR 1.3, 95% CI 1.08–1.57), patients with communicable diseases (OR 1.44, 95% CI 1.23–1.68), and weekend admissions (OR 1.29, 95% CI 1.08–1.55). The 72-h admission window is critical due to a very high mortality risk (OR 3.03, 95% CI 2.58–3.56).
Conclusion
Cardiovascular diseases are the leading cause of hospital admissions and deaths in a tertiary hospital in Northern Tanzania. Lifestyle modification, health education, and community resources are needed to combat the growing burden of cardiovascular and renal disease.
1 INTRODUCTION
The pattern of medical diseases has been changing in different regions. In developing countries, communicable diseases were the main reason for medical admissions. There is a shifting pattern of diseases in developing countries, especially in the tropics, where the trends are toward noncommunicable diseases (NCDs).1 Increased urbanization has led to a rise in NCDs in developed countries, leading to increased mortality due to increased exposure to risk factors and expensive healthcare.2, 3
The rise of NCDs and the underlying burden of infectious diseases has caused an increased burden in developing countries. The increase in the number of diabetes cases has also increased the number of tuberculosis cases, with an underlying burden of human immunodeficiency virus (HIV). As HIV causes a rise in malignant cases, this results in a double burden on developing countries.3
Population-based studies help identify the burden of different diseases compared to hospital-based studies. However, these studies are not available because of a lack of reliable data and expertise, especially in developing countries.4, 5 Population-based studies in our setting will not detail the cause or diagnosis of these diseases. Diseases may determine the pattern of hospital admissions and summarize the health status and disease patterns in the community.4
The study aimed to identify the patterns of disease, length of stay, and outcomes of patients who were admitted to the medical department at Kilimanjaro Christian Medical Centre (KCMC).
2 METHODS
2.1 Study setting and design
The study was undertaken at KCMC in Northern Tanzania between 1st July 2019 and 30th June 2020. KCMC is a teaching hospital serving a population of approximately 15 million people in Northern Tanzania, and its catchment area extends to the central and eastern zones.6 In the medical inpatient department, the bed capacity is 90, but admissions frequently exceed the bed capacity. This hospital-based retrospective observational study included patients aged over 13 years admitted to the medical wards at KCMC. Patients aged 13 years and below were admitted to the pediatric wards, and therefore excluded from the study. Patients admitted for chemotherapy were excluded from the study. Ethical approval for this study was obtained from the Kilimanjaro Christian Medical University College Research and Ethics Committee (no. 2479).
2.2 Definitions
Disease was defined as having an illness requiring medical attention and subsequent admission to the medical ward.
Comorbidities were defined as having one or more diseases accompanying a primary or admitting disease.
Admission was defined as a patient's hospitalization in the medical inpatient department. All admissions were treated as index hospitalizations regardless of the previous hospitalization, whether for the same disease or a different disease.
Clinical outcome was defined as the end point of the patient's stay in the medical ward, whether the patient was discharged home, referred to another hospital, discharged against medical advice, or died in the medical ward.
Cardiovascular diseases were defined as diseases involving the heart and blood vessels.
Noncardiovascular diseases were defined as diseases, including infectious diseases, that did not involve the heart and blood vessels.
2.3 Study variables and analysis
Medical information was retrieved from the computerized databases at KCMC, which included age, sex, insurance status, duration of hospital stay, diagnosis, and admission outcome. The data were collected and entered into a spreadsheet. The data set was cleaned and entered into the Statistical Package for Social Science (SPSS) v26 (IBM; https://www.ibm.com/analytics/spss-statistics-software). The outcomes were the pattern of disease, length of stay, and clinical outcomes of all patients admitted to the medical ward in the defined period. Categorical variables were expressed as numbers and percentages, including median and interquartile range (IQR). For the study variables, their relationship with mortality was analyzed in a univariate analysis model using the odds ratio (OR), with 95% confidence intervals (CI). To analyze mortality with the admission characteristics and disease, we calculated the odds with the chi-square test. A significant trend existed when the odds of each outcome varied significantly with mortality.
3 RESULTS
Between 1st July 2019 and 30th June 2020, 4226 patients were admitted to the medical wards at KCMC. A total of 3930 patients were analyzed after 296 patients admitted for chemotherapy were excluded.
Table 1 shows that out of the 3930 patients, 2105 (53.5%) were males, 1685 (42.9%) were between 51 and 75 years old, with a median age of 57 years (IQR 41–71), 1623 (41.3%) had health insurance, 2762 (70.3%) were discharged home, 854 (21.7%) died, and the median length of stay (LOS) was 6 days (IQR 4–9). There were more males than females across all age groups. Females had more health insurance, with 792 (43.4%) out of 1825 females, compared to males, with 852 (40.5%) out of 2105 males. The common comorbidities were hypertension (19.5%) and type 2 diabetes mellitus (10.1%). However, 3.8% of the patients had HIV. Death was more common in males (23.2%) than in females (20.0%). Among the 854 deaths, those that occurred after the first 3 days of admission accounted for 490 (57.4%) patients, while deaths that occurred within the first 3 days of admission accounted for 364 (42.6%). The mortality rate among 100 admissions admitted within the first 3 days was 9.3%. Deaths that occurred from patients being admitted over the weekend were 23.7%.
| Male | Female | Total | ||||
|---|---|---|---|---|---|---|
| Variables | N | % | N | % | N | % |
| Age | ||||||
| <25 | 192 | 9.1 | 160 | 8.8 | 352 | 9.0 |
| 25–50 | 604 | 28.7 | 574 | 31.5 | 1178 | 30.0 |
| 51–75 | 933 | 44.3 | 752 | 41.2 | 1685 | 42.9 |
| >75 | 376 | 17.9 | 339 | 18.6 | 715 | 18.1 |
| Median (IQR) | 58 | 41–71 | 57 | 41–71 | 57 | 41–71 |
| Insured | ||||||
| No | 1253 | 59.5 | 1033 | 56.6 | 2307 | 58.7 |
| Yes | 852 | 40.5 | 792 | 43.4 | 1623 | 41.3 |
| NHIF | 804 | 95.1 | 733 | 94.2 | 1537 | 94.7 |
| Other | 41 | 4.9 | 45 | 5.8 | 86 | 5.3 |
| Common Comorbidities | ||||||
| Hypertension | 773 | 18.5 | 765 | 20.7 | 1538 | 19.5 |
| Type 2 diabetes mellitus | 408 | 9.7 | 385 | 10.4 | 793 | 10.1 |
| Chronic kidney disease | 291 | 6.9 | 201 | 5.4 | 492 | 6.2 |
| Heart failure | 182 | 4.3 | 236 | 6.4 | 418 | 5.3 |
| HIV | 127 | 3.0 | 174 | 4.7 | 301 | 3.8 |
| Outcome | ||||||
| Discharge home | 1425 | 67.7 | 1337 | 73.3 | 2762 | 70.3 |
| Referral | 95 | 4.5 | 70 | 3.8 | 165 | 4.2 |
| DAMA | 96 | 4.6 | 53 | 2.9 | 149 | 3.8 |
| Death | 489 | 23.2 | 365 | 20.0 | 854 | 21.7 |
| ≤72 h | 209 | 42.7 | 155 | 42.5 | 364 | 42.6 |
| >72 h | 280 | 57.3 | 210 | 57.5 | 490 | 57.4 |
| Weekday admission | 376 | 76.9 | 276 | 75.6 | 652 | 76.3 |
| Weekend admission | 113 | 23.1 | 89 | 24.4 | 202 | 23.7 |
| Length of stay | ||||||
| Median (IQR) | 5 | 3–9 | 6 | 4–9 | 6 | 4–9 |
| Discharge home | 6 | 4–9 | 6 | 4–9 | 6 | 4–9 |
| Referral | 5 | 4–9 | 6 | 3–10 | 5 | 4–10 |
| DAMA | 6 | 3–9 | 6 | 3–8 | 5 | 3–8 |
| Death | 4 | 2–8 | 4 | 2–8 | 4 | 2–8 |
| Total | 2105 | 53.6 | 1825 | 46.4 | 3930 | 100 |
- Abbreviations: DAMA, discharge against medical advice; HIV, human immunodeficiency virus; NHIF, national health insurance fund.
Table 2 shows the insurance status and clinical outcome of patients across different age groups. As stated, patients aged 51–75 years were more common compared to the other age groups, and they also had higher average insurance coverage (53.4%). Those aged 51–75 years had a higher mortality rate (42.4%) than those aged 25–50 years (28.6%). NCDs were the more common admission diagnoses in those aged 51–75 years (44.4%), while communicable diseases were more common in those aged 25–50 years (35.8%).
| Insured | CD | NCD | Discharge | Referral | DAMA | Died | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age categories | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| <25 | 94 | 5.7 | 65 | 11.6 | 287 | 8.5 | 256 | 9.3 | 8 | 4.8 | 21 | 14.1 | 67 | 7.8 |
| 25–50 | 309 | 18.8 | 201 | 35.8 | 977 | 29.0 | 824 | 29.8 | 60 | 36.4 | 50 | 33.6 | 244 | 28.6 |
| 51–75 | 878 | 53.4 | 190 | 33.8 | 1495 | 44.4 | 1188 | 43.0 | 81 | 49.1 | 56 | 37.6 | 360 | 42.2 |
| >75 | 363 | 22.1 | 108 | 18.9 | 609 | 18.1 | 494 | 17.9 | 16 | 9.7 | 22 | 14.8 | 183 | 21.4 |
- Abbreviations: CD, communicable diseases; DAMA, discharge against medical advice; LOS, length of stay; NCD, noncommunicable disease.
Table 3 shows that most of the admission diagnoses were for NCDs (85.7%), which caused 78.8% of the deaths, but there was a higher proportion of deaths observed among patients with communicable diseases (21.2%). Cardiovascular diseases (CVDs) were the most common admission diagnoses, comprising 26.8% of all admissions and 27.9% of all deaths.
| Male | Female | Insured | Discharge | Referral | DAMA | Died | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diseases | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| CD | 297 | 14.1 | 265 | 14.5 | 229 | 13.9 | 357 | 12.9 | 9 | 5.5 | 15 | 10.1 | 181 | 21.2 | 562 | 14.3 |
| NCD | 1808 | 85.9 | 1560 | 85.5 | 1415 | 86.1 | 2405 | 87.1 | 156 | 94.5 | 134 | 89.9 | 673 | 78.8 | 3368 | 85.7 |
| CVD | 504 | 23.9 | 551 | 30.2 | 463 | 28.2 | 746 | 27.0 | 50 | 30.3 | 21 | 14.1 | 238 | 27.9 | 1055 | 26.8 |
| NCVD | 1601 | 76.1 | 1274 | 69.8 | 1181 | 71.8 | 2016 | 73.0 | 115 | 69.7 | 128 | 85.9 | 616 | 72.1 | 2875 | 73.2 |
- Abbreviations: CD, communicable diseases; CVD, cardiovascular disease; DAMA, discharge against medical advice; LOS, length of stay; NCD, noncommunicable disease; NCVD, noncardiovascular disease.
The common causes of admission and death listed in Table 4 showed that chronic kidney disease was the main cause of admission in 492 patients (6.2%), followed by heart failure and stroke in 418 (5.3%) and 406 (5.2%) patients, respectively. Of the 854 deaths, stroke was the leading cause with 129 (15.1%), followed by chronic kidney disease with 95 (11.1%), heart failure with 77 (9%), septicemia with 62 (7.3%), and respiratory tract infections with 57 (6.7%). Stroke has an in-hospital mortality rate of 31.8 deaths per 100 admissions. However, nearly half of all septicemic patients died, with an in-hospital mortality rate of 49.6 deaths per 100 admissions.
| Diagnosis | Death | Admission | Mortality (Deaths/100 admissions) | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Stroke (ischemic/hemorrhagic) | 129 | 15.1 | 406 | 5.2 | 31.8 |
| Chronic kidney disease | 95 | 11.1 | 492 | 6.2 | 19.3 |
| Heart failure | 77 | 9.0 | 418 | 5.3 | 18.4 |
| Septicemia | 62 | 7.3 | 125 | 1.6 | 49.6 |
| Respiratory tract infections | 57 | 6.7 | 218 | 2.8 | 26.1 |
| Human immunodeficiency virus | 30 | 3.5 | 301 | 3.8 | 10.0 |
| Liver disease | 29 | 3.4 | 157 | 2.0 | 18.5 |
| Acute kidney injury | 24 | 2.8 | 117 | 1.5 | 20.5 |
| Tuberculosis | 23 | 2.7 | 103 | 1.3 | 22.3 |
| Malignant neoplasm of liver | 19 | 2.2 | 54 | 0.7 | 35.2 |
| Acute myeloid leukemia | 15 | 1.8 | 22 | 0.3 | 68.2 |
| Unknown gastrointestinal bleeding | 15 | 1.8 | 78 | 1.0 | 19.2 |
| Malignant neoplasm of lung | 13 | 1.5 | 37 | 0.5 | 35.1 |
| Esophageal varices | 11 | 1.3 | 183 | 2.3 | 6.0 |
| Organophosphate poisoning | 11 | 1.3 | 15 | 0.2 | 73.3 |
The logistic regression analysis in Table 5 showed an overall increased risk of mortality associated with male sex (OR 1.21, 95% CI 1.03–1.41), noninsured patients (OR 1.67, 95% CI 1.42–1.96), patients aged >75 years (OR 1.30, 95% CI 1.08–1.57), communicable diseases (OR 1.44, 95% CI 1.23–1.68), and weekend admissions (OR 1.29, 95% CI 1.08–1.55). A greater association was seen among patients who had a clinical outcome within the first 72 h of admission (OR 3.03, 95% CI 2.58–3.56).
| Odds ratios | 95% confidence interval | |
|---|---|---|
| Male | 1.21 | 1.03–1.41 |
| Not Insured | 1.67 | 1.42–1.96 |
| <25 | 0.83 | 0.63–1.10 |
| 25–50 | 0.91 | 0.77–1.08 |
| 51–75 | 0.96 | 0.82–1.12 |
| >75 | 1.30 | 1.08–1.57 |
| Communicable disease | 1.44 | 1.23–1.68 |
| Cardiovascular disease | 0.92 | 0.83–1.03 |
| ≤72 h | 3.03 | 2.58–3.56 |
| Weekend admission | 1.29 | 1.08–1.55 |
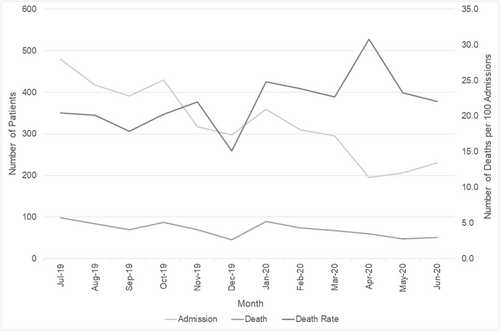
Observing the admissions and deaths all year round, the number of deaths per 100 admissions is higher from January 2020 onward, with the highest recorded in April 2020 compared to 2019 (Figure 1).
4 DISCUSSION
In the mid-nineteenth century, most medical admissions in Africa were for infectious diseases such as malaria, bacterial pneumonia, tetanus, tuberculosis, and meningitis.7, 8 In a few African studies in the past 50 years, some trends have become obvious: the proportion of CVD admissions has increased significantly, and the proportion of infectious disease admissions has decreased.7 Our study showed that CVDs, including heart failure and stroke, were the most common causes of hospital admission, followed by chronic kidney disease and respiratory tract infections. Heart failure is prevalent in this setting, with frequent readmissions and poor outcomes.9, 10 Hypertension and type 2 diabetes mellitus were the most common comorbidities. This study emphasizes a shift in disease burden toward cardiovascular diseases as the leading cause of hospital admission and death.
Trends in sub-Saharan Africa are becoming similar to those in other countries, such as Saudi Arabia, where CVDs were 34.4%, followed by infections at 16%.5 Although there are regions in Africa that present more infections than NCDs, a study in Ethiopia showed pneumonia (22.8%) is the most common cause of admission, followed by other infections (16.4%) and chronic meningitis (13.1%).2 In Nigeria, malaria (38.9%) was the most common cause of admission.11 Our study shows that CVDs were 26.8%, followed by infections at 11.1%, as parts of Africa have not yet succumbed to the double burden.
The shift toward NCDs in the medical admission patterns observed in this study could be because urbanization has affected most of these patients. Increasing urbanization may change the diet, reduce physical activity and lead to an increased rate of obesity.12 Overall, CVDs and chronic kidney diseases were the most common causes of medical admission in this study, which could be explained by the increased prevalence of cardiovascular risk factors such as hypertension and type 2 diabetes mellitus. The rise in chronic kidney diseases may also reflect increased use of over-the-counter medications such as nonsteroidal anti-inflammatory drugs.
At KCMC in 2012, they found NCDs to be the main cause of admission compared to infectious causes, at 79.9% and 20.1%, respectively.13 The trend has been growing toward NCDs as their number has increased to 88% while infections have decreased to 12%. Parts of Africa still have a high prevalence of HIV, as shown in this study, where only 3.8% of all admissions had an HIV infection and it was the sixth leading cause of death. In Uganda, 30.4% of admissions were HIV-infected and were the leading cause of infectious deaths,14 and similarly, there was a higher number of deaths in Cameroon because of HIV.15 Patients may have benefited from ongoing HIV sensitization and subsidized medical care, which may explain the decrease in HIV-related mortality.
LOS is used to assess the efficacy of hospital management, quality of care, and functional evaluation. The LOS is determined by the type of disease and the cause of admission, as the LOS differs between diagnoses. Reduced LOS is associated with fewer hospital-acquired infections and medication side effects, including a reduced burden of medical fees and increased bed turnover time.16 Hospitals with high bed capacities have longer LOS than those with low bed capacities.17 Poor care coordination can be a sign of poor care quality.18 In Italy, the LOS was different for discharged patients and those who died, being 13.1 and 10.7 days, respectively.19 In the United Kingdom, the median LOS was 9 days.13 A study in South Korea stated that the average LOS was 7 days, with a median of 4 days.16 At KCMC in 2012, the median LOS was 5 days from admission to discharge and 3 days from admission to death.13 Our study shows that the median LOS was 6 days, as the median for admission to discharge was 6 days, and the median for admission to death was 4 days. The LOS may be longer in developed countries because it may reflect efforts to minimize the rate of readmission, while in developing countries, it may reflect increased turnaround time to manage hospital bed space.
Sub-Saharan Africa is on the verge of an epidemiological transition, as NCDs account for 35% of all deaths, with CVDs accounting for 13% of all deaths and 37% of all NCD deaths in that region.20 Our study shows that NCDs account for 78.8% of deaths, and CVDs account for 27.9% of all deaths. The burden of elderly patients has increased as life expectancy has improved. Infectious diseases accounted for 17.1% of deaths in Africa over the last half-century, with gastrointestinal diseases and CVDs accounting for 16.2% and 16.0%, respectively.7 A study in Tanzania found that 65% of deaths resulted from NCDs, with pneumonia (20.9%) as the leading infectious cause.21 Our study shows that septicemia and respiratory tract infections are the fourth and fifth leading causes of death, respectively, while NCDs are the top three. Currently, the trend is similar to that of developed countries.
The mortality rate of patients admitted within 72 h of admission was 9.3%. This may be because of patient delays in reaching the hospital or patients not receiving timely treatment at the hospital. Patient delays may occur because patients often seek medical attention elsewhere before going to a hospital, as studies have shown that 56% of Northern Tanzanians visit traditional healers during their illnesses.22 Patients also visit dispensaries and health centers before visiting a tertiary hospital. These delays result in patients developing complications or presenting with advanced disease that makes management difficult, especially in resource-limited settings. At the hospital, the high patient-to-doctor ratio and the high number of patients needing investigations may cause delays in proper treatment, as the long turnaround time may further delay making a diagnosis and subsequent treatment.23
The “weekend effect” suggests that patients admitted on weekends have a worse outcome than those admitted on weekdays. Compared to patients admitted on weekdays, those admitted on weekends had a 10%–12% higher risk of death.24, 25 In this study, 23.7% of patients who died were admitted over the weekend. The rates are lower in developed countries, as the United States of America was 2.7% 24 and Spain was 11.1%,26 compared to Kenya at 21.1%.27 However, in this study, there was a 4.6% increase in mortality over the weekend admissions compared to the weekday admissions.
The rate and cause of death are different across regions. In Italy, 86.7% of patients were discharged home, 8.3% were transferred to a different ward, and 5.0% died in the hospital.19 A study in Saudi Arabia showed hospital discharge among 83.3% of patients. However, 6.7% were transferred to another health facility, 4.1% left against medical advice, and 5.9% died.5 Our study shows that 70.3% went home, but 21.7% died. The mortality rate is different and higher in developing countries because of the lack of healthcare availability, as seen in Sudan, Ethiopia, Nigeria, Uganda, and Tanzania, with rates of 4.7%, 12.6%, 16.0%, 17.1%, and 25.6%, respectively.2, 4, 14, 21, 28 These differences may be because of the availability of resources for diagnosis and treatment, nursing staff, and specialists to cater to the patients, as well as the difference in comprehensive health services offered at each health center studied. This is evident as the inpatient department continues to have a shortage of nursing staff and specialists as per the country's staffing requirements.6 At KCMC in 2012, there were 25.7% deaths, compared to 6.5% in the United Kingdom.13 Although the death rate dropped from 25.7% to 21.7% at KCMC, there are higher death rates seen in Africa than in developed countries, and this may be due to a delay in seeking medical care, disease severity at presentation, and healthcare-economic barriers.13, 21
A retrospective analysis in Tanzania found that causes of death among adults over 10 years found malaria to be the leading cause (11.2%), followed by HIV (11.1%), CVDs (8.5%), respiratory diseases (8%), and cancer (7.3%).29 In the same study, they looked at deaths according to regions: in the Kilimanjaro region, the mortality trend switched over 10 years and showed that by 2010, the leading causes of death were HIV and tuberculosis, but by 2015, the leading causes were CVDs.29 In our study, malaria, and tuberculosis were not the leading causes of death in our population, although HIV is still present.
There was a drop in the number of admissions in 2020, specifically in April 2020, which was around the time the coronavirus disease 2019 (COVID-19) pandemic arrived in Tanzania. Notably, the number of deaths did not drop even though the number of admissions was reduced, which resulted in an increased death rate from the month of April onward. We postulate a change in health-seeking behavior during the COVID-19 epidemic as a cause of decreased admissions. However, the increase in death rates may be due to the reorganization of hospital operations and medical personnel and delays in the diagnosis and treatment of non-COVID-19 cases.
5 CONCLUSION
Cardiovascular diseases such as heart failure and stroke are considered the leading causes of hospital admission and death in a teaching community hospital in Moshi, Tanzania. Similarly, there has been an increase in the number of NCDs, a decrease in the number of infectious diseases, and a decrease in the death rates over the last 9 years. However, the weekend effect is clear, with a higher number of deaths occurring from patients admitted over the weekend. The increased death rates may have been attributed to the COVID-19 pandemic. Hypertension and type 2 diabetes mellitus are prevalent comorbidities among hospitalized patients. Health-related databases and disease registries are required to estimate the burden of cardiovascular diseases in Tanzania. Lifestyle changes, healthy eating, patient education, aggressive management of hypertension and diabetes mellitus within the community, and the allocation of necessary resources are needed to combat the growing burden of cardiovascular disease.
AUTHOR CONTRIBUTIONS
Abid M. Sadiq: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; supervision; validation; visualization; writing – original draft; writing – review & editing. Rosalia E. Njau: Data curation; investigation; methodology; validation; visualization; writing – review & editing. Kajiru G. Kilonzo: Conceptualization; formal analysis; methodology; project administration; supervision; validation; visualization; writing – review & editing.
ACKNOWLEDGMENT
The authors are grateful to the internal medicine department for their work and support of all the patients they managed.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
Ethical approval for this study was obtained from Kilimanjaro Christian Medical University College Research and Ethics Committee (no. 2479).
TRANSPARENCY STATEMENT
The lead author Abid M. Sadiq affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




