Investigation of the causal relationship between cholelithiasis and Parkinson's disease: A bidirectional Mendelian randomization study
Abstract
Background
Parkinson's disease (PD) and cholelithiasis are a huge public health burden. Although observational studies have suggested a potential link between PD and cholelithiasis, the causal relationship between the two remains uncertain. To address this gap, we performed a two-sample bidirectional Mendelian randomization analysis using genetic tools.
Method
Genome-wide association study summary statistics for all traits were obtained from publicly available databases. We used strict control steps in instrumental variable selection to screen for single nucleotide polymorphisms (SNPs) from summary-level genome-wide association studies. In addition, all F-statistics were >10, indicating no weak instrumental bias. The inverse variance weighting (IVW) method was the primary method used to assess causal associations. Four other MR methods (MR-Egger, Weighted Median, Simple mode, and Weighted mode) were also used to complement IVW. Various sensitivity tests were also performed to assess reliability: (1) Cochrane's Q test for assessing heterogeneity, (2) MR-Egger intercept test and MR-PRESSO global test for assessing horizontal multiplicity, and (3) leave-one-out sensitivity test for determining stability.
Results
We selected a total of 30 SNPs as instrumental variables. It was demonstrated that cholelithiasis had a causal effect on the risk of PD (OR = 1.146, 95% CI: 1.062–1.236, p < 0.001) in IVW method.
Conclusion
The results of our analysis revealed an increased risk effect of cholelithiasis against PD, which may give light on new approaches to PD prevention and therapy.
1 INTRODUCTION
Parkinson's disease (PD) is the most common type of degenerative motor disease of the central nervous system and the most common symptom of dyskinesia, estimated 6.1 million patients affected worldwide in 2016, characterized by a broad spectrum of both motor and nonmotor symptoms (NMS).1, 2 PD has experienced exponential growth as one of the world's fastest-growing neurological disorders for unclear reasons, with a global burden that has more than doubled in the last generation.2 Rapid attention is required to a significant medical issue that involves comprehending the etiology of PD and developing efficient preventive and therapeutic strategies.3
Cholelithiasis, known as gallstones, is a widespread and crucial public health issue with a pooled prevalence of 6.1% and an incidence of 0.47 per 100 person-years, and gallstone frequency rises with age.4 In industrialized nations, cholelithiasis affects roughly 10%–15% of individuals and has become increasingly prevalent in recent decades.5 It is characterized by a solid clot in the gallbladder or biliary tract6 and has traditionally been classed as cholesterol, pigmented, or mixed depending on their constitution. Approximately 10%–20% of adults suffer from cholelithiasis and 20% of patients tolerate complications6-8 include sepsis, pancreatitis, cholecystitis, cholangitis, and gallbladder rupture. The impacts of cholelithiasis raise the expense of healthcare, burden society financially, and potentially endanger lives. Gallstone disease is one of the most costly digestive disorders from a social perspective.9
A clinical study conducted by the Patricia Modaine team in 1995 has performed gallbladder ultrasound in 91 patients with PD and 80 controls. The prevalence of cholelithiasis was found to be 38.5% in the PD group and 30% in the control group, with a significant age-adjusted correlation between PD and the frequency of cholelithiasis. Autonomic dysfunction in patients with PD may lead to dysfunction of gastrointestinal peristalsis, which may affect gallbladder emptying and promote gallstone formation.10 Recently, the gastrointestinal microbiome in cholelithiasis and the nervous system were suggested similar functions because they have similar advantages.11
Furthermore, it was found that intestines of patients in PD contained higher amounts of secondary bile acids which might be a contributing factor to gallstone development.12 Recent evidence suggest fasting gallbladder volume was increased in PD patients. A series of observational clinical studies provides light on biliary dysfunction in PD and advocates for more investigation into the impact of cholelithiasis.13 Interestingly, a nationwide cohort study recently found that individuals who underwent cholecystectomy had a considerably increased risk of PD, a tendency that was more prevalent in males than in women.14 Therefore, it is currently unclear whether there is causality between cholelithiasis and PD.
Nowadays Mendelian randomization (MR) analyses have emerged as a powerful implement to calculate the causal influence of certain risk variables on an outcome of interest (such as illness) by employing genetic variation as an instrumental variable (IV).15 MR has several advantages compared with randomized controlled trials, in terms of cost and time savings, the ability to analyze massive amounts of data, and the lack of ethical restrictions.16
To our knowledge, this is the first study to investigate the causal connection between PD and cholelithiasis using MR techniques. Our investigation attempts to add novel perspectives and factual data to the body of knowledge regarding the risk of PD.
2 MATERIALS AND METHODS
To evaluate the bidirectional relationship between gallstones and PD using MR analysis, we applied three fundamental assumptions to the genetic variants17: (1) association assumption, indicating that SNPs are strongly correlated with exposure; (2) independence assumption, implying that SNPs are not influenced by other factors in the exposure-outcome pathway; and (3) exclusivity assumption, indicating that SNPs influence outcomes exclusively through exposure and not via other pathways.
2.1 Data sources
Our exposure variable of interest was cholelithiasis, and our outcome variable was PD. The IEU OpenGWAS platform (GWAS ID: finn-b-K11_CHOLELITH) was used to extract SNPs strongly linked with gallstones as IVs from the FinnGen data set comprising 19023 European-origin cases and 195144 controls. Besides, we used the IEU OpenGWAS platform (GWAS ID: ebi-a-GCST90018894) for PD as our outcome variable which consists of 2638 European-origin cases and 477,380 controls.
2.2 Selection of SNPs
By filtering the GWAS data, we included SNPs with correlations fulfilling p < 5 × 10–8 as instrumental factors, in line with the fundamental assumptions of MR investigations. We imposed the requirements of r2 < 0.001 and window size = 10,000 kb to lessen the influence of linkage disequilibrium (LD) on study outcomes.18 We calculated the F statistic [F = R2 × (N − 2)/(1 − R2)] to evaluate the strength of instrumental variables, for each SNP separately to ensure robust associations between instrumental and endogenous variables and prevent weak instrumental variable bias.19, 20
2.3 MR analysis
All of our analyses were carried out using RStudio (version 4.3.3), with a significance threshold of p < 0.05. The TwoSampleMR software tool, which retrieves data automatically from the IEU GWAS database, was utilized for all MR correlation studies. The principal analytical technique for MR was the inverse variance weighting (IVW) approach, which adopts a meta-analytical approach to combine Wald ratio estimates of the causal effect of SNPs, providing a consistent estimate for evaluating exposure's influence on outcomes. This technique presents a customized and effective analysis based on the number of IVs available.21 For MR analysis, we further employed four additional techniques: weighted median, MR-Egger, simple mode, and weighted mode22 as additional complementary methods for assessing causal effects. Odds ratios (OR) was used to measure the strength of association.
Furthermore, sensitivity tests were executed to evaluate the robustness of the results, and people with missing data were eliminated to reduce the possibility of confounding effects. To ascertain whether the findings indicated interstudy heterogeneity, a heterogeneity test was applied. When there was no discernible heterogeneity (p > 0.1 in Cochran's Q analysis), the fixed-effects IVW approach was employed in conjunction with the conventional IVW approach. The instances of genetic pleiotropy were investigated using MR-Egger regression and the Mendelian randomization pleiotropy residual sum and outlier (MR-PRESSO test).23, 24 To determine whether reverse causation was present, we also conducted an inverse Mendelian analysis of favorable outcomes.
2.4 Institutional review board statement
No additional ethical approval was required because all of the data used in this investigation came from publicly accessible databases.
3 RESULTS
3.1 Single nucleotide polymorphism (SNP) screening
Using quality control approaches, SNPs from summary-level genome-wide association studies were screened. We selected a total of 30 SNPs as instrumental variables. The exposure of these genes satisfied established thresholds for genome-wide significance (p < 5 × 10–8, r2 < 0.001, kb = 10,000). Additionally, all F-statistic had a value greater than 10, suggesting that there was no mild instrumental bias(Table 1).
| SNP | OA | EA | Beta | SE exposure | EAF exposure | p Value | F statistics |
|---|---|---|---|---|---|---|---|
| rs28473566 | G | A | −0.247 | 0.016 | 0.173 | 4.272e-52 | 232.092 |
| rs114041253 | G | T | 0.290 | 0.032 | 0.038 | 3.585e-19 | 79.948 |
| rs114350689 | T | C | 0.358 | 0.045 | 0.020 | 1.305e-15 | 63.857 |
| rs6742078 | G | T | 0.087 | 0.012 | 0.392 | 1.629e-12 | 49.780 |
| rs1260326 | T | C | 0.079 | 0.013 | 0.649 | 3.464e-10 | 39.610 |
| rs72613899 | G | A | −0.115 | 0.016 | 0.167 | 1.308e-12 | 50.568 |
| rs11887534 | G | C | 0.840 | 0.022 | 0.084 | 1.000e-200 | 1369.000 |
| rs191092790 | A | G | 0.328 | 0.042 | 0.021 | 8.074e-15 | 60.412 |
| rs11124977 | G | C | 0.199 | 0.024 | 0.067 | 1.39e-16 | 68.460 |
| rs4681502 | T | C | 0.081 | 0.012 | 0.458 | 1.409e-11 | 45.367 |
| rs12633863 | G | A | −0.130 | 0.012 | 0.492 | 1.882e-27 | 117.903 |
| rs2290846 | G | A | 0.124 | 0.014 | 0.221 | 6.312e-18 | 74.630 |
| rs2228375 | T | C | 0.068 | 0.012 | 0.395 | 3.537e-08 | 30.205 |
| rs12538707 | T | C | −0.206 | 0.018 | 0.135 | 1.067e-30 | 133.415 |
| rs17154498 | C | A | −0.108 | 0.013 | 0.286 | 4.966e-16 | 66.184 |
| rs2326077 | C | T | −0.134 | 0.012 | 0.615 | 1.996e-27 | 118.509 |
| rs686030 | C | A | 0.148 | 0.019 | 0.881 | 1.706e-15 | 63.656 |
| rs635634 | C | T | 0.092 | 0.015 | 0.200 | 1.024e-09 | 37.210 |
| rs12775076 | C | T | 0.294 | 0.051 | 0.015 | 6.858e-09 | 33.562 |
| rs55665473 | G | A | 0.092 | 0.013 | 0.281 | 4.177e-12 | 48.266 |
| rs174565 | C | G | 0.0890 | 0.014 | 0.232 | 4.580e-10 | 39.106 |
| rs7979473 | A | G | 0.076 | 0.012 | 0.581 | 5.727e-10 | 38.501 |
| rs16961277 | A | G | −0.126 | 0.017 | 0.138 | 4.312e-13 | 52.604 |
| rs28929474 | C | T | 0.368 | 0.043 | 0.020 | 4.394e-17 | 70.722 |
| rs62128824 | T | C | −0.159 | 0.017 | 0.151 | 7.089e-21 | 88.293 |
| rs8108864 | G | A | 0.083 | 0.013 | 0.299 | 2.014e-10 | 40.531 |
| rs2972623 | G | T | −0.145 | 0.017 | 0.155 | 1.841e-17 | 72.651 |
| rs708686 | C | T | 0.102 | 0.013 | 0.334 | 9.743e-16 | 64.758 |
| rs1800961 | C | T | 0.385 | 0.030 | 0.045 | 8.580e-39 | 170.148 |
| rs2618566 | G | T | 0.0750 | 0.013 | 0.677 | 8.313e-09 | 33.018 |
- Abbreviations: Beta, SD change in urate per effect allele; EA, effect allele; EAF, effect allele frequency; OA, other allele; SE, standard error; SNPs, single-nucleotide polymorphisms.
3.2 MR analysis
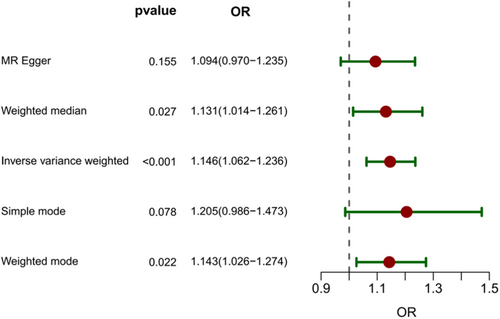
Fixed-effects IVW was employed because there was no substantial heterogeneity among SNPs (p > 0.1). The MR findings (Figure 1) indicated a substantial correlation between a genetically determined gallstone risk and an increased chance of PD (OR = 1.146, 95% CI: 1.062–1.236,p < 0.001). These results are consistent with the weighted median approach (OR = 1.131, 95% CI: 1.014–1.261, p = 0.027) and the weighted mode method (OR = 1.143, 95% CI: 1.026–1.274, p = 0.022), suggesting a causal relationship between cholelithiasis and the risk of PD, and a positive association was found. MR-Egger regression (OR = 1.094, 95% CI: 0.970–1.235, p = 0.155) and simple mode means (OR = 1.205, 95% CI: 0.986–1.473, p = 0.078) shows no significant. As shown in the forest plot in Figure 2A, the results of the IVW method indicated that the prevalence of PD gradually increased with the onset of cholelithiasis.
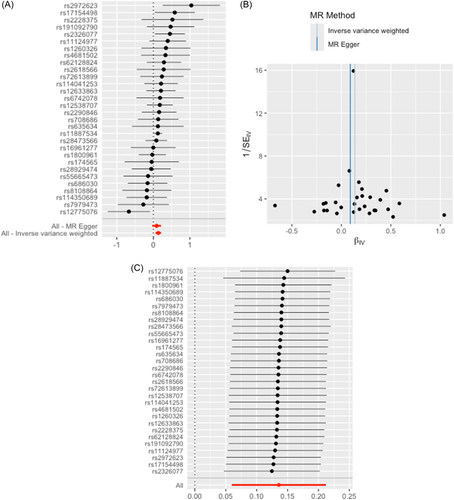
All of the SNPs' F-values were larger than 10, the Cochran Q test, the Funnel plot (Figure 2B), the leave-one-out approach, and other measures demonstrated the validity of our findings. No heterogeneity was detected by Cochran's Q test among the IVs (Q = 28.982, p = 0.466) (Table 2). Moreover, no horizontal pleiotropy was detected using the MR-Egger intercept (p = 0.350) (Table 2). The MR-PRESSO analysis did not perceive any instrumental outlier at the significance level of 0.05 (Table 2). To evaluate the conformance of the included SNPs, a leave-one-out analysis was performed; the findings showed that no single SNP significantly altered the overall MR results (Figure 2C).
| Heterogeneity horizontal pleiotropy MR-PRESSO | |||||||
|---|---|---|---|---|---|---|---|
| Q | df | p Value | Egger_intercept | SE | p Value | p Value | |
| 28.982 | 29 | 0.466 | 0.010 | 0.010 | 0.350 | 0.480 | |
For the purpose of investigating the impact of PD on the risk of cholelithiasis, we conducted a reverse Mendelian randomization analysis to minimize reverse causality (Individual SNP test,Wald ratio: OR = 1.166 (1.036–1.314), p = 0.011).
3.3 External validation of another cholelithiasis data set
To improve the generalizability of the results to other populations, we were also interested in discovering if the causal relationship between gallstones and an increased risk of PD continued in ethnic groups other than Fins. For MR analysis that required external validation, a supplementary European cholelithiasis database (GWSID: ukb-b-18700) inside the IEU OpenGWAS platform was implemented, which consists of 7682 cases of European ancestry and 455,251 control subjects.
The findings of the MR analysis were reaffirmed and demonstrated a strongly positive causal impact when investigating the relationship between gallstones and the risk of PD (Inverse variance weighted: OR = 5442.711, 95% CI: 54.928–5.933e+05, p < 0.001). These findings are in line with the weighted median method (OR = 737.997, 95% CI: 3.601–1.599e+05, p = 0.017). The Cochran Q test (Q = 12.790, p = 0.46), MR-Egger intercept (SE = 0.011, p = 0.097), and MR-PRESSO analysis (p = 0.442) demonstrated the validity of our validation. However, it shows no significance in a reverse Mendelian randomization analysis (Individual SNP test, Wald ratio: OR = 0.999, 95% CI: 0.998–1.002, p = 0.973).
3.4 Confounding analysis
To confirm that IVs are not connected to the other common risk factors for Parkinson's disease (diabetes, alcohol intake, smoking, and coffee consumption),25, 26 we examined each of the cholelithiasis-associated SNPs using LDlink platform (https://ldlink.nih.gov/). A total of nine SNPs linked to confounding variables were investigated (details are in Table S1). Even after discarding the promiscuous SNPs, genetically predicted gallstones still had a significant causal effect on the increasing risk of PD (Inverse variance weighted: OR = 1.140, 95% CI: 1.049–1.240, p = 0.002). The weighted median method and the weighted mode method also supported this association with an OR of 1.133 (95% CI: 1.012–1.270, p = 0.030) and 1.143 (95% CI: 1.023–1.277, p = 0.028) respectively. These causal relationships were ascertained by sensitivity analyses of the leave-one-out approach (p > 0.05). The detailed results of the MR analyses are shown in Figures S1 and S2 and Table S2.
4 DISCUSSION
In this study, we investigated the causal relationship between cholelithiasis and risk of PD, using two-sample bidirectional MR which helps to reduce residual confounders and various biases, thus enhancing our causal inference ability by employing exposure-related genetic variations as proxies for exposure. Genetic variance is inherited from the parents and remains unchanged from birth, and the relationship with outcome is chronologically rational. Gametes are formed according to the Mendelian law of inheritance, in which parental alleles are randomly assigned to offspring. Therefore, inherited variants are not affected by potential confounders such as environmental exposure, socioeconomic status, and behavioral factors.27
To the best of our understanding, this is the first study to investigate the causal connection between PD and cholelithiasis. The results of our analysis revealed an increased risk effect of cholelithiasis against PD, which provides significant implications for clinical and public health. Meanwhile, we made sure that these correlations had been assessed in two independent populations, and a series of sensitivity tests were executed to evaluate the robustness of the results, which improves the validity of the results. There was no horizontal pleiotropy (p = 0.35) in the selected IVs, according to the MR-Egger regression intercept term results, and there were no outliers (p = 0.48) in the MR-PRESSO global test. The Cochran's Q test results showed that these IVs did not significantly differ from one another (p = 0.466). No single SNP was shown to have a significant impact on the overall calculations by the leave-one-out study. Even after removing the confounding SNPs, the calculated MR values remained significant, and the conclusion's direction aligned with the original study. Moreover, there was no consistent result whether PD causally contributes to the development cholelithiasis in external validation of another cholelithiasis data set. Even though, the casual association found in our study shed new evidence of therapeutic ideas for PD. There is still much to discover about the potential link between cholelithiasis and PD.
In recent decades, an enormous amount of pharmacologic studies have shown the naturally occurring bile acid ursodeoxycholic acid (UDCA), also as a traditional treatment of chronic cholecystitis,28 is demonstrated a promising mitochondrial rescue compound for PD in both clinical and experimental.29-31 Cholelithiasis can lead to abnormalities in the components of bile as well as poor bile excretion. These modifications may have an indirect impact on the development and course of PD by influencing the intestinal absorption of nutrients, particularly those essential for the synthesis and metabolism of dopamine.32, 33 On the other hand, changes in the PD gut microbiome are linked with increase in the bile acid pool.12 Interestingly, it was demonstrated an increase in bile acid production in patients with cholesterol gallstones by Metabolite Set Enrichment Analysis (MSEA)34 In rats with PD symptoms overexpressing α-synuclein, gut microbial diversity is altered and levels of the associated bile acids are significantly increased, thereby affecting motor symptoms.35 The brain-gut-microbiota axis is crucial to the etiology of PD.36 Changes in the composition and activity of the gut microbiota due to cholelithiasis37 may have an effect on neuroinflammation, oxidative stress, and neurotransmitter homeostasis, all of which have been connected to the pathophysiological mechanisms behind PD.11, 38 Cholelithiasis may trigger an inflammatory response with the release of inflammatory mediators, which enter the central nervous system through the circulation, leading to neuroinflammation and neuronal damage, increasing the risk of PD. To date, it was found that cholecystectomy did not raise the risk of colorectal cancer or metabolic disorders.39 In a nationwide retrospective cohort study, it is found that the cholecystectomy group has a higher incidence of PD, which is more significant in males but not in females. Potential processes linked to a higher risk of PD following cholecystectomy could involve dysbiosis of the gut microbiota and metabolic inefficiency stemming from elevated levels of secondary bile acids.14 It is important to note that these mechanisms are still in the research phase and more studies are needed to confirm their specific role in the relationship between cholelithiasis disease and PD.
Nevertheless, it is important to recognize the limitations of our MR investigation. First of all, the GWAS databases used in our study are only available for European populations begs the question of whether this causal relationship is still substantial in other groups, calling for further study. Second, the MR-Egger and simple mode means method demonstrated no significant association between cholelithiasis and PD in both major study databases and external validation databases. Indeed, the MR-Egger technique may be used to examine horizontal pleiotropy of genetic variation, yielding causal impact estimates consistent with IVW when pleiotropic SNPs linked with the outcome are excluded.23, 40 In the presence of multivalence, MR-Egger estimations are favored. In our analysis, the MR-Egger regression intercept term revealed that the selected IVs did not exhibit horizontal multicollinearity. The simple model approach is an unweighted model of causal impact estimate that is less biased than other models but less accurate due to bias reduction.41, 42 Third, both cholelithiasis and PD are heterogenic conditions, however the absence of pertinent stratification data prohibits us from analyzing disease subtypes in more detail. Future attentions on the association between PD and cholelithiasis should be implemented in the future.
In conclusion our MR analysis provide tentative initial evidence to support roles of genetic liability to cholelithiasis and risk of PD and offer novel perspectives on preventing PD. In the future, more investigation is required to confirm the existence of cholelithiasis and investigate the possible involvement of bile acid metabolism and its relationship with gut microbiota in the etiology of PD.
AUTHOR CONTRIBUTIONS
Zijiao Yang: Writing—original draft; writing—review and editing; investigation; formal analysis; validation; methodology; software; data curation; conceptualization; visualization. Chengfu Song: Supervision. Chong Lu: Visualization; validation; supervision; software.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The original contributions presented in the study are included in the article/Supporting Information, further inquiries can be directed to the corresponding author.
The lead author Chengfu Song, Chong Lu affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.