Investigating the effects of systemic thrombolysis on electrocardiography and pulmonary artery blood pressure in patients with pulmonary embolism
Abstract
Background and Aims
We aimed to evaluate the association between electrocardiography (ECG) and echocardiographic findings in patients with pulmonary embolism (PE) before and after systemic thrombolysis.
Methods
We included 38 PE patients admitted to the hospital with approved right ventricular (RV) dysfunction who were indicated for systemic thrombolysis. Indications for systemic thrombolysis were considered as patients who were either hemodynamically unstable on admission or became unstable in the course of hospital admission. Systemic thrombolysis was performed by either Reteplase or Alteplase. ECG and echocardiographic findings were documented at baseline and 12–24 h following systemic thrombolysis.
Results
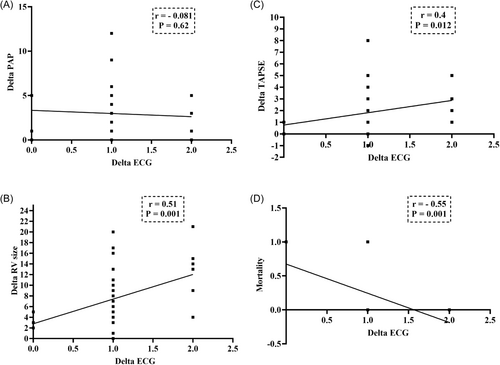
Our results showed that TAPSE significantly increased while RV size and pulmonary artery systolic pressure (PAP) notably decreased after systemic thrombolysis (p < 0.001). The ECG abnormalities markedly diminished after systemic thrombolysis in PE patients (p < 0.001). Additionally, 100% of our patients had more than one ECG abnormality at baseline, while 55.3% had no ECG abnormalities after systemic thrombolysis. Further, the median number of ECG abnormalities remarkably attenuated after systemic thrombolysis (from 2.0 (1.0) to 0.0 (1.0), p < 0.001). Our results also revealed that delta RV size (r = 0.51, p = 0.001) and delta TAPSE (r = 0.4, p = 0.012) were positively correlated while mortality (r = −0.55, p = 0.001) was negatively associated with changes in the number of ECG abnormalities before and after systemic thrombolysis.
Conclusion
We showed that systemic thrombolysis improved echocardiographic and electrocardiographic findings in PE patients. Additionally, a greater decreased number of ECG abnormalities after systemic thrombolysis was accompanied by more improvement in RV size and TAPSE and a lower mortality rate.
1 INTRODUCTION
Pulmonary embolism (PE) is a life-threatening condition and a major cause of global morbidity and mortality.1 American Heart Association has classified PE patients as low-risk, sub-massive (also known as intermediate-risk), and massive (also known as high-risk) based on various clinical and paraclinical features.2 PE management and outcomes majorly vary among patients with massive and non-massive PE,3 which, besides the nonspecific clinical findings, reinforces the importance of risk stratification in these patients using potential clinicopathological tools.
Electrocardiography (ECG) is a simple assessment tool that can be used as an initial test to conduct on individuals presenting with early diagnosis with signs and symptoms of PE.4, 5 In addition, ECG findings were significantly associated with hemodynamic instability and a worse prognosis.6, 7 Therefore, ECG is potentially useful for PE risk stratification and prognosis due to its low cost and broad availability in medical care settings. Echocardiography is also an easily addressed assessment utility that is a valuable tool for assessing RV function and size associated with PE prognosis.4 Multiple RV parameters were found to be correlated with the prognosis of PE, such as RV systolic pressure, tricuspid annular plane systolic excursion (TAPSE), pulmonary artery systolic pressure (PAP), inferior vena cava (IVC) collapsibility, and ratio of RV to left ventricular end-diastolic diameter.8, 9
Thrombolytic therapy is an accepted modality in treating hemodynamically unstable PE patients. Still, there are controversies around its role in stable patients as it is accompanied by a greater risk of malignant hemorrhagic events.10, 11 A recent Cochrane update also emphasized the fact that there is limited data with considerable risk of bias, plus major heterogeneity among studies evaluating the possible benefits or risks of thrombolytic therapy in PE, especially in hemodynamically stable patients.11 However, it was reported that thrombolytic treatment may positively affect survival, hemodynamic state, findings of CTPA and echocardiography, lung perfusion, and pulmonary hypertension.10, 11 Common effective thrombolytic agents used in acute PE include alteplase, reteplase, tenecteplase, urokinase, and streptokinase.12, 13
However, there is limited data on the impacts of systemic thrombolysis with alteplase and reteplase on ECG and echocardiographic changes in acute PE patients. Therefore, the present study aimed to investigate the possible association between multiple ECG and echocardiographic findings in patients with diagnosed PE who were indicated for systemic thrombolysis, as well as the effects of reteplase and alteplase on these entities.
2 METHODS
2.1 Ethical consideration
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences under the approval code of IR. MUMS. MEDICAL. REC.1401.439. Additionally, written informed consent was obtained from all individuals. Furthermore, study procedures were done in accordance with the stipulations of the Declaration of Helsinki.
2.2 Study design and participant selection
The present study is a single-center, prospective, observational study conducted from May 2022 to May 2023 in Ghaem Hospital, affiliated with the Mashhad University of Medical Sciences. The study aimed to evaluate the association between various ECG and echocardiographic findings in patients with systemic thrombolysis-indicated PE, as well as the effects of reperfusion treatment on these findings. Additionally, this study hypothesized that ECG abnormalities is correlated with echocardiographic parameters and mortality in patients with systemic thrombolysis-indicated PE following systemic thrombolysis.
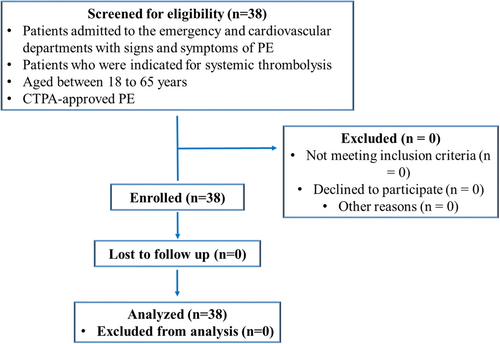
The study participants were selected from individuals admitted to the emergency and cardiovascular departments with signs and symptoms of PE, including hemoptysis, acute chest pain, syncope, and new or worsening dyspnea, who also fulfilled the following inclusion criteria. Inclusion criteria comprised individuals aged between 18 and 65 years with computed tomography pulmonary angiography (CTPA)-approved PE who were indicated for systemic thrombolysis. Additionally, RV dysfunction was confirmed by two-dimensional transthoracic echocardiography (TTE). Exclusion criteria included pregnancy, lactation, history of intracranial hemorrhage, known cerebrovascular lesion, active bleeding, and incomplete patient documentation. We enrolled 38 systemic thrombolysis-indicated PE patients and no patients had the exclusion criteria (Figure 1).
2.3 Systemic thrombolysis indications and modalities
Indications for systemic thrombolysis were considered as patients who were either hemodynamically unstable on admission or became unstable in the course of hospital admission.14 Hemodynamic instability was defined as systolic blood pressure (SBP) < 90 mmHg for more than 15 min or a need for inotrope drugs to maintain the SBP > 90 mmHg.2 Drugs employed for systemic thrombolysis were either reteplase (10 units, two IV bolus doses) or alteplase (100 mg, 2-h slow infusion, IV). In this regard, the choice of the thrombolytic drug was at the discretion of the treating physicians.
2.4 Outcome evaluation
Demographics and past medical history were abstracted from all participants, which included age, gender, and history of diabetes mellitus (DM), hypertension (HTN), chronic kidney disease (CKD), coronary artery disease (CAD), and COVID-19 infection.
In terms of specific cardiovascular testing, all individuals have undergone ECG, echocardiography, and CTPA on admission. ECG and echocardiographic assessments were repeated 12–24 h following systemic thrombolysis. Finally, the mortality rates during hospitalization and admission end results were documented.
2.5 Electrocardiography
Twelve-lead ECGs were obtained from all participants at the time of admission and 12–24 h following systemic thrombolysis. Two expert cardiologists interpreted ECG findings separately while both were oblivious to the diagnosis and outcomes of patients. Regarding discrepancies, a third cardiologist also assessed the ECG up until resolution. S1Q3T3 was defined as the presence of an amplitude of more than 0.15 mV in the S-wave of lead I and Q-wave of lead III, besides the inversion of the T-wave in lead III. The RBBBs, whether complete or incomplete, were determined as their standard criteria. In addition, sinus tachycardia was described as a heart rate of >100 BPM in the presence of a normal P-wave. T-wave inversion was also defined as the presence of an inverted T-wave in three consecutive precordial leads. The mentioned ECG abnormalities are most common abnormalities during acute pulmonary emboli.15
2.6 Echocardiography
We performed TTE utilizing a Philips EPIQ CVx Ultrasound System with a X5-1 Transducer. All echocardiography assessments were conducted by expert cardiologists and assessed according to the current American Society of Echocardiography (ASE) guideline recommendations.16 TTE was done to measure the RV size, PAP, and TAPSE at baseline and 12–24 h after systemic thrombolysis.
Right atrial pressure (RAP) was considered as the following according to the IVC diameter and collapsibility18 (Table 1).
| IVC diameter | Collapsibility | RAP (mmHg) |
|---|---|---|
| Normal | Normal | 3 |
| Normal | Abnormal | 8 |
| Abnormal | Normal | 8 |
| Abnormal | Abnormal | 15 |
2.7 Statistical analysis
Data were analyzed using the SPSS version.26 statistical software (SPSS Inc.) and GraphPad Prism 8.01 software (GraphPad Software Inc.). First, the normality of data was evaluated using the Shapiro–Wilk test. Parametric data were shown as means ± standard deviations (SD), whereas nonparametric data were expressed as median with interquartile range (IQR). Additionally, categorical parameters were defined as a number (N) with a percentage (%) and analyzed using the Chi-square test. As appropriate, the comparison between continuous variables was performed using paired t-test for parametric data or Mann–Whitney U and Wilcoxon tests for nonparametric data. In addition, the correlation between changes in the number of ECG abnormalities and echocardiographic parameters before and after systemic thrombolysis was measured using the Spearman correlation coefficients. The P values ≤ 0.05 levels were considered statistically significant.
3 RESULTS
3.1 Demographic and clinical characteristics
We evaluated 38 patients with PE with a mean age of 56.97 ± 16.5 years. Furthermore, 47.4% of patients were male and 52.6% were female. Additionally, 30 (78.9%) patients with PE were discharged alive from the hospital and 8 (21.1%) died (Table 2). The causes of death in these patients were RV dysfunction and collapse progressive RV dysfunction. All patients that received thrombolytic therapy were in high-risk group. It means that all patients had hemodynamic instability and were in shock. Vasopressor prescription was determined by physician's decision and hemodynamic condition of the patients.
| Characteristics | N = 38 | |
|---|---|---|
| Age | 56.97 ± 16.5a | |
| Gender | Male | 18 (47.4%)b |
| Female | 20 (52.6%)b | |
| Hypertension | 15 (39.5%)b | |
| Hyperlipidaemia | 1 (2.6%)b | |
| Diabetes | 1 (2.6%)b | |
| CKD | 0 (0)b | |
| IHD | 3 (7.9%)b | |
| History of Covid-19 | 23 (60.5%)b | |
| Hospitalization result | Discharge Alive | 30 (78.9%)b |
| Death | 8 (21.1%)b | |
| Pulmonary CT angiography | MPA | 19 (50%)b |
| LPA | 1 (2.6)b | |
| DIS RPA | 2 (5.3)b | |
| DIS LPA | 2 (5.3)b | |
| PRO LPA | 3 (7.9)b | |
| PRO RPA | 1 (2.6)b | |
| PRO RPA + R seg | 3 (7.9)b | |
| DIS RPA + R seg | 1 (2.6)b | |
| DIS RPA + L seg | 1 (2.6)b | |
| PRO LPA + L seg | 2 (5.3)b | |
| DIS LPA + L seg | 1 (2.6)b | |
| DIS LPA + DIS RPA | 1 (2.6)b | |
| PRO RPA + DIS LPA | 1 (2.6)b | |
- Note: Chronic kidney disease (CKD), ischemic heart disease (IHD), Main pulmonary artery (MPA), Left pulmonary artery (LPA), Right pulmonary artery (RPA), Proximal (PRO), Distal (DIS), Left segmental (L seg), Right segmental (R seg); Data presented as
- a Mean ± SD or
- b N (%).
The results of pulmonary CT angiography of studied patients are presented in Table 2. We found that 50% of our studied patients had pulmonary emboli in the main pulmonary artery (MPA). Additionally, the median time between systemic thrombolysis and second electrocardiographic and echocardiographic evaluation was 12.0 (12.0) h.
3.2 Echocardiographic measurements
The echocardiographic results of PE patients before and after systemic thrombolysis are shown in Table 3. Our results showed that TAPSE significantly increased after systemic thrombolysis (p < 0.001). In contrast, RV size and PAP notably decreased after systemic thrombolysis in PE patients (p < 0.001 for both).
| Variables | Before | After | P-value | |
|---|---|---|---|---|
| Echocardiographic | TAPSEa | 11.42 ± 2.71 | 12.89 ± 2.78 | <0.001d |
| RV sizeb | 39.0 (10.25) | 30.0 (9.0) | <0.001e | |
| PAPb | 36.0 (14.0) | 33.5 (10.25) | <0.001e | |
| Electrocardiographic | Normal sinus rhythmc | 0 (0%) | 21 (55.3%) | <0.001 c |
| Sinus tachycardiac | 14 (36.8%) | 1 (2.6%) | ||
| Sinus tachycardia +RBBBc | 13 (34.2%) | 1 (2.6%) | ||
| Sinus tachycardia + S1Q3T3c | 6 (15.8%) | 2 (5.3%) | ||
| Sinus tachycardia + S1Q3T3+ precordial inverted T-wavec | 1 (2.6%) | 0 (0%) | ||
| Sinus tachycardia + precordial Inverted T-wavec | 3 (7.9%) | 0 (0%) | ||
| Sinus rhythm + RBBBc | 1 (2.6%) | 5 (13.2%) | ||
| Sinus rhythm + S1Q3T3c | 0 (0%) | 6 (15.8%) | ||
| Sinus rhythm + precordial inverted T-wavec | 0 (0%) | 2 (5.3%) |
- Abbreviations: PAP, pulmonary artery pressure; RBBB, right bundle branch block; RV, Right ventricular; TAPSE, tricuspid annular plane systolic excursion; Data presented as
- a Mean ± SD,
- b Median (Interquartile range), or
- c N (%); comparing the results of before and after systemic thrombolysis
- d using paired t-test,
- e Wilcoxon test, and e: using Chi-square test.
The changes in echocardiographic variables before and after systemic thrombolysis according to the number of ECG abnormalities (one or two) before systemic thrombolysis are presented in Table 4. We showed that the median of changes in RV size before and after was higher in patients with two ECG abnormalities (8.5 (8.5)) than one abnormality (4.0 (4.0), p = 0.02). However, no significant differences were found in mortality, delta PAP, and delta TAPSE between PE patients with one and two ECG abnormalities (p = 0.14, 0.075, and 0.249, respectively, Table 4).
| Number of ECG abnormalities | 1 | 2 | P-value | |
|---|---|---|---|---|
| Delta PAPa | 3.0 (3.0)a | 2.0 (2.25)a | 0.075c | |
| Delta RV sizea | 4.0 (4.0)a | 8.5 (8.5)a | 0.024c | |
| Delta TAPSEa | 1.0 (1.0)a | 2.0 (2.0)a | 0.249c | |
| Mortalityb | Yes | 3 (2.0) | 4 (18.2) | 0.14d |
| No | 12 (80.0) | 18 (81.8) | ||
- Abbreviations: PAP, Pulmonary artery pressure; RV, Right ventricular; RBBB, right bundle branch block; TAPSE, tricuspid annular plane systolic excursion; Data presented as
- a Median (interquartile range) or
- b N (%); comparing the results of two groups
- c using Mann–Whitney t-test and
- d using the Chi-square test.
3.3 Electrocardiographic assessments
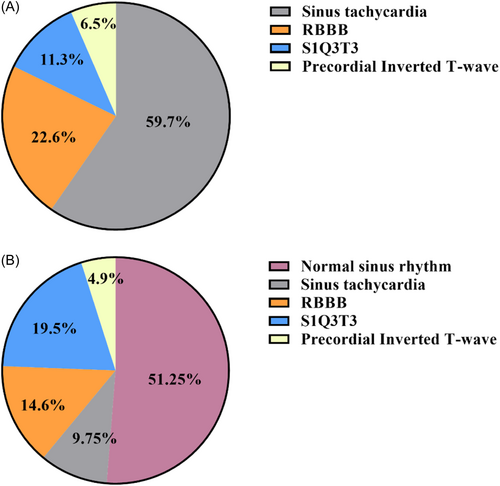
The ECG results of PE patients before and after systemic thrombolysis are shown in Table 3 and Figure 2. The ECG abnormalities markedly diminished after systemic thrombolysis in PE patients (p < 0.001). Before systemic thrombolysis, 59.7% of PE patients had sinus tachycardia, 22.6% had RBB, 11.3% had S1Q3T3, and 6.5% had precordial inverted T-wave. After systemic thrombolysis, 51.25% had normal sinus rhythm, 19.5% had S1Q3T3, 14.6% had RBBB, 9.75% had sinus tachycardia, and 4.9% had precordial inverted T-wave.
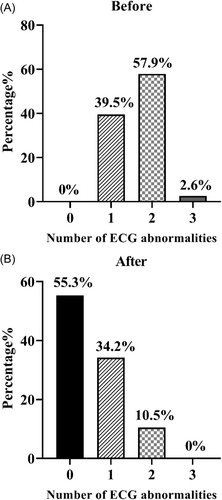
The number of ECG abnormalities in PE patients is illustrated in Figure 3. Before systemic thrombolysis, 39.5% of patients had one, 57.9% had two, and 2.6% had three abnormalities. Furthermore, 55.3% had no ECG abnormalities after systemic thrombolysis, 34.2% had one, and 10.5% had two abnormalities (Figure 3). Additionally, the median number of ECG abnormalities remarkably attenuated after systemic thrombolysis (decreased from 2.0 (1.0) to 0.0 (1.0), p < 0.001).
3.4 Correlation between ECG abnormalities and echocardiographic changes
The correlation between changes in the number of ECG abnormalities and echocardiographic parameters before and after systemic thrombolysis is represented in Figure 4. Our results revealed that delta RV size (r = 0.51, p = 0.001) and delta TAPSE (r = 0.4, p = 0.012) were positively correlated with changes in the number of ECG abnormalities. Additionally, mortality was negatively correlated with changes in the number of ECG abnormalities before and after systemic thrombolysis (r = −0.55, p = 0.001).
4 DISCUSSION
PE is considered the third major cause of cardiovascular emergency and mortality worldwide. Thrombolytic therapy in these patients quickly dissolves the thrombus and restores hemodynamic stability.19 However, there is limited data on the impacts of systemic thrombolysis with alteplase and reteplase on ECG and echocardiographic changes in acute PE patients. Therefore, we aimed to determine the ECG and echocardiographic changes in patients with PE before and after systemic thrombolysis.
Our results showed that TAPSE significantly increased while RV size, PAP, and ECG abnormalities notably decreased after systemic thrombolysis in PE patients. We also showed that the median of changes in RV size before and after was higher in patients with two ECG abnormalities than one abnormality. Additionally, delta RV size and delta TAPSE were positively correlated, while mortality was negatively correlated with changes in the number of ECG abnormalities before and after systemic thrombolysis.
Several pieces of evidence emphasized that PE patients had RV dysfunction, which is commonly assessed by echocardiography.20, 21 Echocardiographic-confirmed right ventricular (RV) dysfunction was shown to be a valuable prognostic factor among PE patients.4, 5 After systemic thrombolysis, we found that TAPSE were markedly elevated, while RV size and PAP was strikingly alleviated in PE patients. In line with our results, Nishanth and coworkers noticed that RV function remarkably improved while PAP and tricuspid regurgitation severity notably diminished after systemic thrombolysis in PE patients.22 Alsancak et al. demonstrated that PAP notably attenuated while systolic and diastolic blood pressure markedly elevated after thrombolytic therapy in acute PE patients.23 These studies may confirm our results regarding changing RV size, TAPSE, and PAP after systemic thrombolysis. In fact, the pulmonary hypertension following pulmonary emboli is due to acute obstruction in pulmonary artery by large clot and neuro-hormonal activation that leads to increase in pulmonary vascular resistance. When you relieve the obstruction, neuro-hormonal release will decrease gradually and pulmonary hypertension and pulmonary vascular resistance will decrease consequently. So, RV dysfunction and TR are related to increase in pulmonary vascular resistance that after successful treatment, logically will decrease.
We found that before systemic thrombolysis, 59.7% of PE patients had sinus tachycardia, 22.6% had RBB, 11.3% had S1Q3T3, and 6.5% had precordial inverted T-wave. After systemic thrombolysis, 51.25% had normal sinus rhythm, 19.5% had S1Q3T3, 14.6% had RBBB, 9.75% had sinus tachycardia, and 4.9% had precordial inverted T-wave. In the other words, 39.5% of our patients had one, 57.9% had two, and 2.6% had three ECG abnormalities before systemic thrombolysis. Interestingly, after systemic thrombolysis, 55.3% of our patients had zero, 34.2% had one, 10.5% had two, and 0% had three ECG abnormalities. In line with our results, Marwah et al. investigated 48 PE patients and showed that 56.25% had sinus tachycardia, 16.67% had S1Q3T3, and 6.3% had precordial inverted T-wave.24 Bolt and coworkers evaluated 380 acute PE patients and determined that 82% had at least one ECG abnormality. Furthermore, they noticed that 26% of PE patients had tachycardia, 15% had S1Q3T3, 15% had RBBB, and 13% had precordial inverted T-wave.25
We also revealed that ECG abnormalities notably diminished after systemic thrombolysis in PE patients. In addition, 100% of our patients had more than one ECG abnormality at baseline. Interestingly, 55.3% of patients had no ECG abnormalities after reperfusion therapies. In line with our results, Alsancak and coworkers showed that heart rate, QT dispersion, corrected QT interval, T peak-to-end interval (Tp-e), Tp-e/QT ratio, and index of cardiac electrophysiological balance (iCEB) value strikingly diminished after thrombolytic therapy in acute PE patients.23 Sahan et al. supported that the frontal plane QRS‑T (f[QRS-T]) angle meaningfully decreased after thrombolytic treatment in patients with acute PE.26 Another study also suggested that heart rate, ECG abnormalities, and f[QRS-T] were meaningfully reduced after thrombolytic therapy in PE patients.27 The results of these studies are in line with our results regarding the reduction of ECG abnormalities after systemic thrombolysis in PE patients.
Our results supported that delta RV size and delta TAPSE were positively correlated with changes in the number of ECG abnormalities before and after systemic thrombolysis. Similarly, Novicic et al. showed that changes in RV systolic pressure were notably greater in PE patients with ECG abnormalities, including S-wave in the I lead and aVL, and RBBB at the first 5 days of hospitalization.28 Golpe and coworkers suggested that ECG score was positively correlated with PAP, pulmonary artery diameter, and RV/LV ratio in PE patients with hemodynamic stability.29 Taken together, RV size and TAPSE improvement were observed in patients with more decreased number of ECG abnormalities after systemic thrombolysis.
The in-hospital mortality rate in PE patients who underwent systemic thrombolysis in our study was 21.1%. Similarly, Singh and coworkers determined that in-hospital mortality was 35% in high-risk PE and 11% in intermediate-risk PE patients.30 Another study showed an overall in-hospital mortality of 18% in acute PE patients admitted to ICU.31 However, Novicic et al. evaluated 110 hospitalized patients with PE and reported an in-hospital mortality rate of 13.6%.28 The difference in mortality rate may be related to the lower number of our patients and the severity of PE patients in our study.
Our results also showed that in-hospital mortality was negatively correlated with changes in the number of ECG abnormalities. In this regard, mortality was lower in patients with normal ECG after systemic thrombolysis. Novicic and coworkers revealed that the presence of three ECG abnormalities, including S-wave in the I lead, S-wave in the aVL, and RBBB during the 5 days of hospitalization, is correlated with 30-day survival.28 Similarly, right ventricular strain, any abnormal ECG signs, and the number of abnormal ECG signs were notably associated with 90-day mortality or in-hospital complications in acute PE patients.25 A meta-analysis also emphasized that ECG abnormalities such as S1Q3T3, RBBB, T-wave inversion, and atrial fibrillation strongly predict in-hospital mortality in PE patients.32 Collectively, a higher number of ECG abnormalities at baseline leads to a greater in-hospital mortality rate.
Our study also has a number of limitations. First, it was a single-center study with a small sample size. The second limitation is the lack of long-term follow-ups to better understand the improvement of PE patients after systemic thrombolysis. It is recommended to perform multi-center studies with a larger population and longer duration of follow-ups. As another important limitation, we did not record the patient's hemodynamics before and after systemic thrombolysis, including heart rate, oxygen saturation, systolic and diastolic blood pressure, and mean arterial pressure. Considering the importance of hemodynamics in PE patients, it is highly recommended to evaluate these parameters in future studies.
5 CONCLUSION
Our results showed that systemic thrombolysis improved echocardiographic and electrocardiographic findings in PE patients. Additionally, delta RV size and delta TAPSE were positively correlated, while mortality was negatively correlated with changes in the number of ECG abnormalities before and after systemic thrombolysis.
AUTHOR CONTRIBUTIONS
Mostafa Dastani: Conceptualization; Methodology; Funding acquisition; Supervision. Vahid Reza Askari: Formal analysis; Writing—original draft; Writing—review and editing. Arya Nasimi Shad: Investigation; Writing—original draft. Niyayesh Ghorbani: Data curation; Investigation. Vafa Baradaran Rahimi: Investigation; Formal analysis; Software; Writing—original draft; Writing—review and editing.
ACKNOWLEDGMENTS
This study was financially supported by the research council of Mashhad University of Medical Sciences (Grant Number: 4011045).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
TRANSPARENCY STATEMENT
The lead author Niyayesh Ghorbani, Vafa Baradaran Rahimi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ETHICS STATEMENT
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences under the approval code of IR.MUMS.MEDICAL.REC.1401.439. IR. MUMS. MEDICAL. REC.1401.439. Additionally, written informed consent was obtained from all individuals. Written informed consent was obtained from all volunteers who participated in this study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. Data is available from the corresponding author upon reasonable request.