The effect of maternal age on still birth in Africa: A systematic review and meta-analysis
Abstract
Background and Aims
Stillbirth is a public health as well as a development problem in low and middle-income countries. The studies that found out maternal age as a factor for the risk of stillbirth reported different findings. This systematic review and meta-analysis is believed to fill the inconclusiveness of these findings. Hence, the aim of this systematic review and meta-analysis is to estimate the pooled effect of advanced maternal age on stillbirth in Africa.
Methods
PubMed & HINARY databases and Google Scholar search engine were searched to access the primary studies. The extracted data using Microsoft excel was exported to Stata 15 software for analysis. The presence of heterogeneity was checked using Cochran's Q statistic and the I2 test. Publication bias was examined by using funnel plot and Egger's test. The pooled effect measure with DerSimonian and Laird method of random-effect model was reported using odds ratio (OR) with respective 95% confidence interval.
Results
Totally, 14 articles are included for the systematic review and meta-analysis. The stillbirth reported by the studies ranges from 15 to 146.7 per 1000 births. The overall OR of advanced maternal age (≥35 years) on stillbirth is 1.42 (1.18, 1.71) when compared with the age group of 20–35 years. The cumulative effect of getting pregnant at advanced age on stillbirth was slightly increasing from year to year.
Conclusion
Advanced maternal age is a risk factor for stillbirth. Health Information Communication on the risk of getting pregnant at the advanced ages on stillbirth should be well addressed to all women of reproductive age group.
1 BACKGROUND AND AIMS
Stillbirth, literally, refers to a dead born fetus.1 This is to mean birth of a baby showing no signs of life.2 World Health Organization (WHO) defined stillbirth as late fetal death at ≥28 completed weeks of gestation or ≥1000 g birth weight.3 However, a gestational age criterion has been suggested as a single parameter since it is a more reliable predictor of viability than birth weight and because gestational age data is more likely to be accessible for stillbirths than birth weight data.4 Thus, in low- and middle-income countries, the WHO recommends that a threshold of 28 completed weeks be considered for mortality audits.5
Stillbirth can happen either during labor (intrapartum death) or before the start of labor (antepartum death). Obstetric problems or maternal diseases can cause fetuses to die intrauterine, before labor begins. However, many antepartum intrauterine deaths have no known cause.6
Stillbirth is problematic for both public health and development in lower- and middle-income regions. Every year, more than two million (2.6) newborns worldwide are expected to die before they are born, resulting to 18.9 stillbirths per 1000 births.5, 7 Though a 14.5% decline in the worldwide stillbirth rate was observed, sub-Saharan Africa and Oceania were having smallest percentage declines (<10%). Three of the five countries with the highest rates worldwide were African countries. These are Nigeria (42 per 1000 births), Djibouti (34 per 1000 births), and Senegal (34 per 1000 births). In addition, 4 of the 10 countries that account for 67% of all stillbirths (1.76 million) and 54% of all births globally are African nations, including Ethiopia.8
Sub-Saharan Africa has an extremely high stillbirth rate of 28 per 1000 births, especially when compared to developed nations where the rate is only 3 per 1000 births.7
The majority of the 2.6 million stillbirths that occur worldwide each year—98%—occur in low-income and middle-income nations, with south Asia and sub-Saharan Africa accounting for three-quarters of them. These impact the families most underserved by health-care systems; around 60% occur in rural areas and over half in conflict and emergency zones.9
Since 2000, stillbirth rates have decreased more slowly than maternal mortality or under five children mortality. By 2030, the target is for every nation to have 12 or fewer stillbirths per 1000 births. Ninety-four countries—mostly high-income and upper middle-income nations—have already reached this target, but at least 56 countries—mostly in Africa and in conflict-affected areas—have not. To achieve this target, they will need to more than double their current rate of progress. Better data are essential to accelerate progress toward this target.4
Annually, stillbirths make up about 3% of all deliveries in sub-Saharan Africa. Every year, more than 3.2 million babies are born dead, and the actual number is likely greater due to underreporting of stillbirths and data limitations.10
The only way to prioritize and advocate for action to lower the stillbirth rate is through better cause of death data and better stillbirth counting.
Knowing the valid estimate and underlying factors is a prerequisite for reducing this high rate of stillbirth.10 Age is one of the determinant factors reported by the studies. But there is no conclusive report regarding the effect of maternal age on still birth. Some of them reported positive association11-15; some protective association16-19; and the others no association.20, 21 This systematic review and meta-analysis is needed to overcome this inconclusiveness of findings, and the researchers believes that it produced a conclusive finding on the effect of maternal age on risk of stillbirth.
Though few systematic reviews22, 23 regarding the effect of maternal age on stillbirth were conducted previously, they are only systematic reviews that merely present the narrative synthesis of the findings of the different primary studies. This left the inconclusiveness remain unaddressed. They have failed to conduct a meta-analysis that shows the pooled single effect estimate because of high heterogeneity of the included primary studies as stated in the reviews. Hence, our study certainly filled these gaps.
The lancet report also showed that research on stillbirth continues to be underdeveloped and underfinanced compared with the stillbirth burden.24 This study will contribute in narrowing of this research gap.
The 2030 target of having 12 and fewer stillbirths per 1000 births for every country will be only achieved with the support of valid evidence on the causes of the stillbirth. Thus, this study will be one of the valid documents that indicate the effect of age on the risk of still birth. It will help the policy makers formulate and endorse effective policies and interventions for reducing stillbirth. Health care practitioners will also use the finding in their day-to-day activities so that their clients will be informed of the risks of stillbirth. And finally, mothers and fathers can use the information to prevent themselves from unexpected loss due to stillbirth. They will also be also beneficial from the interventions endorsed by the higher officials and implemented by the clinicians.
Generally speaking, healthcare professionals, program managers, administrators, and legislators can help to prevent future deaths and parent grief and improve the quality of care given throughout the health system by keeping track of stillbirths and neonatal deaths, learning where and why these deaths occurred, and attempting to understand the underlying contributing causes and avoidable factors.5
2 METHODS
2.1 Protocol registration and review reporting
The protocol of this systematic review and meta-analysis was registered at International Prospective Register of Systematic Reviews (PROSPERO) with a Registration ID: CRD42020216210. The review process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), which is guidance for reporting of systematic reviews and meta-analyses.25, 26
2.2 Eligibility criteria
Studies were selected according to the criteria outlined below.
2.2.1 Inclusion criteria
Study setting: Africa
Study design: observational studies (cross sectional, case control, and cohort)
Study year: no restriction
Exposure: maternal age
Outcome of interest: stillbirth
Language: articles that are reported in English
Publication condition: published and unpublished articles.
2.3 Exclusion criteria
Studies that do not have maternal age variable as a factor; have different method of outcome measurement; and cannot be accessed the full document after all possible options (like communicating with e-mail) had been tried were excluded.
2.4 Information source and search strategy
Databases such as PubMed/MEDLINE, CINHAL and Health Inter Network Access to Research Initiative (HINARI), and a search engine Google scholar were searched to access the studies.
The search strategy was composed of the following key search terms: age, “risk factor*,” determinants, “associated factor*,” predictors, factors, Stillbirth, “still birth*,” stillborn, “still born*,” Africa, and the names of all African countries. These key terms were used to develop the search strategy using the “Medical Subject Headings (MeSH)” and “All fields” by linking them with Boolean operators “AND” and “OR” as appropriate. Which means synonym terms of the same concept are joined by “OR” whereas different terms of different terms are joined by “AND” (Files S1 and S4). The literature search was restricted to the English language, human study group, journal article, and observational studies. The search for studies was conducted from May 17 to 23, 2021.
2.5 Study selection
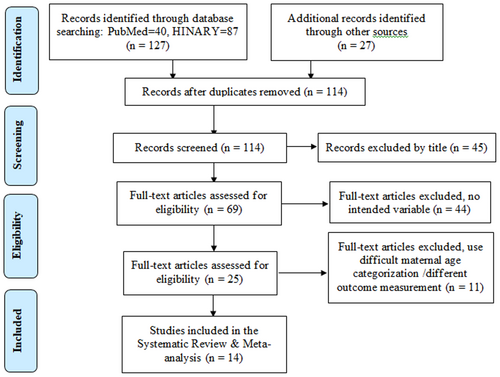
All studies retrieved from different databases and search engines were exported to EndNote X9 reference manager software. Duplicate articles were identified and removed. Two reviewers (A. M. and S. W.) independently screened and selected the articles based on the basis of their Topic, Abstract and full text as necessary. Disagreements between the reviewers were solved by discussion and consensus. The article selection procedure is summarized and synthesized using the PRISMA flow diagram (Figure 1).27
2.6 Quality appraisal
To minimize the risk of bias associated with selection, two reviewers (A. M. and S. W.) evaluated the articles' quality. The studies' quality was assessed using the Joanna Briggs Institute (JBI) critical appraisal checklist (File S2). Those studies that score above 50% were considered as they pass of the quality appraisal (File S5).28
2.7 Data extraction
The two reviewers extracted the data using a Microsoft Excel data extraction sheet that was customized based on a standard JBI data extraction format. The following details were extracted: initial author, study year, study period, publication year, country of the study, sample size, study design, study setting, mean age of mothers, proportion of rurality, proportion of ANC (at least once), proportion of previous stillbirths, proportion of married mothers, proportion of illiterates, rate of stillbirth, and OR of age ≥35 years with corresponding confidence intervals (CIs) (File S3).
2.8 Data analysis
For additional analysis, the extracted data were exported to Stata version 15 software. The descriptive analysis was presented using a text as well as a table to describe the characteristics and findings of each primary study.
The presence of heterogeneity among the studies was determined and quantified using Cochran's Q test and the I2 statistics respectively. A p < 0.1 of Cochran's Q test was used to declare heterogeneity.29 And the I2 statistics (54.9%) was declared as the presence of moderate heterogeneity.30 Heterogeneity analyses (like subgroup analysis, sensitivity analysis, and meta regression) for an investigation of the sources of heterogeneity were not performed because of its moderate heterogeneity.
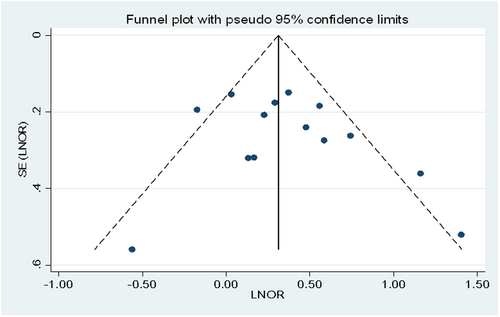
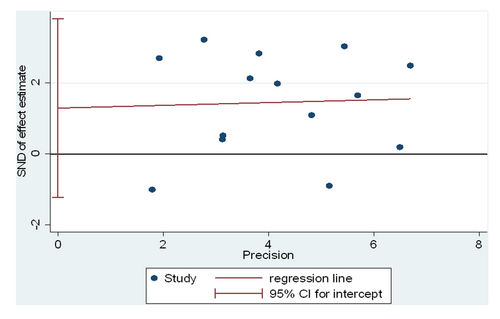
Using an examination of the funnel plot and Egger's graph, as well as Egger's & Begg's test with a p < 0.05, the potential risk of publication bias was determined.
The pooled effect measure was computed with DerSimonian and Laird method of random-effect model and reported using odds ratio (OR) with the respective 95% CI. And finally cumulative meta-analysis was also performed.
3 RESULT
3.1 Study selection
Totally 154 articles were retrieved from databases and search engines. One hundred and fourteen articles were left when duplicate studies were removed. Of these 45 of them were with unrelated titles and were excluded only by reading their titles. The full texts including their abstracts of the left 69 articles were assessed for eligibility determination. Among these 44 of them had not assessed the intended variable (i.e., maternal age). The last 11 removed articles used either different method of outcome measurement or maternal age categorization which is difficult for combining. Finally, 14 articles are included for the Systematic Review and Meta-Analysis (Figure 1).
3.2 Study characteristics
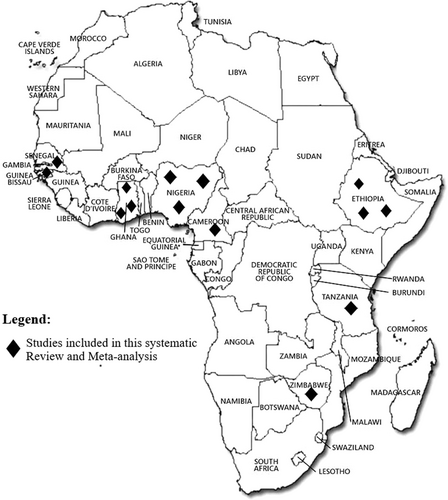
The 14 selected studies were conducted between 1997 and 2019 having a study period that ranges from 3 months16 to 6 years.31 Concerning their study country: three studies are from Ethiopia,16, 32, 33 three studies from Nigeria,19, 34, 35 three studies from Ghana,31, 36, 37 and the rest five studies are contributed from Guinea-Bissau,17 Cameroon,38 Zimbabwe,39 Gambia,40 and Tanzania41 (Figure 2, Table 1). The sample size they used ranges from 28841 to 20,49731 that yields the total sample size for this review 106,646 (Table 1).
| ID | Author | Study year | Study period | Publication year | Country | Sample size | Sample size categorized | Study design | Study setting |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Afulani | 2007 | 1 year | 2018 | Ghana | 4868 | 3052–10,837 | Cross-sectional | Community based |
| 2 | Berhe | 2018 | 3 months | 2019 | Ethiopia | 573 | 565–3052 | Cross-sectional | Institution based |
| 3 | Bjerregaard | 2007–2013 | 5 years and 6 months | 2018 | Guinea-Bissau | 38,164 | >10,837 | Cross-sectional | Both |
| 4 | Dassah | 2009 | 1 year | 2014 | Ghana | 8758 | 3052–10,837 | Cross-sectional | Institution based |
| 5 | Egbe | 2018–2019 | 2 years | 2020 | Cameroon | 592 | 565–3052 | Case-control | Institution based |
| 6 | Engmann | 2002–2008 | 6 years | 2012 | Ghana | 20,497 | >10,837 | Cross-sectional | Community based |
| 7 | Feresu | 1997–1998 | 1 year | 2005 | Zimbabwe | 17,072 | >10,837 | Cross-sectional | Institution based |
| 8 | Jammeh | 2008 | 6 months | 2010 | Gambia | 1519 | 565–3052 | Cross-sectional | Institution based |
| 9 | Lema | 2018–2019 | 8 months | 2020 | Tanzania | 288 | <565 | Case-control | Institution based |
| 10 | Okonofua | 2014 | 6 months | 2019 | Nigeria | 4416 | 3052–10,837 | Cross-sectional | Institution based |
| 11 | Olusanya | 2005–2007 | 3 years | 2009 | Nigeria | 7216 | 3052–10,837 | Cross-sectional | Institution based |
| 12 | Suleiman | 2010–2012 | 3 years | 2015 | Nigeria | 455 | <565 | Case-control | Institution based |
| 13 | Welegebriel | 2011–2015 | 5 years | 2017 | Ethiopia | 540 | <565 | Case-control | Institution based |
| 14 | Yadeta | 2016 | 3 months | 2018 | Ethiopia | 1688 | 565–3052 | Cross-sectional | Institution based |
3.3 Risk of bias within studies
Two assessors (M. A. and K. T.) assessed the quality of individual studies by using the JBI critical appraisal checklist for observational studies. The disagreements raised by the assessors while giving a score were solved by discussion and consensus. Those papers that scored above 50% were considered as they passed the appraisal. All the 14 eligible papers had passed through this appraisal and all of them scored greater than 50% (Files S2 and S).
3.4 Results of individual studies
Only 7 out of the 14 studies reported the mean age of the mothers that ranges from 26.5933 to 30 years.41 All except one study reported rate of stillbirth per 1000 births. Based on their report the highest rate (146.7/1000) is found from Nigeria34 and the lowest (15/1000) is from Ghana36 (Table 2).
| ID | Author | Age of mothers (mean) | Rurality proportion (%) | ANC proporn (at least once) | Previous stillbirth proporn (%) | Married proporn (%) | Illiterates proporn (%) | Rate of stillbirth (per 1000 births) | OR of age ≥35 years | LnOR of age ≥35 years | SELnOR of age ≥35 years |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Afulani | NR | 0.67 | 1 | 4 | 72 | 33.3 | 15.8 | 1.61 | 0.48 | 0.24 |
| 2 | Berhe | NR | 6.8 | NR | NR | 96.5 | 9.8 | 36.8 | 4.07 | 1.40 | 0.52 |
| 3 | Bjerregaard | 25 | NR | NR | NR | NR | 15.3 | 50 | 1.34 | 0.29 | 0.18 |
| 4 | Dassah | 27.4 | NR | NR | NR | NR | NR | 59 | 1.03 | 0.03 | 0.15 |
| 5 | Egbe | 27.54 | 20.6 | NR | 1.2 | 67.1 | 0 | 35 | 1.14 | 0.13 | 0.32 |
| 6 | Engmann | NR | NR | 63.3 | NR | NR | 44.2 | 23 | 1.45 | 0.37 | 0.15 |
| 7 | Feresu | 24.6 | 14.2 | 89.4 | NR | NR | NR | 56 | 0.57 | −0.56 | 0.56 |
| 8 | Jammeh | NR | NR | NR | NR | NR | NR | 156 | 1.25 | 0.23 | 0.21 |
| 9 | Lema | 30 | 59 | NR | 12 | 86.8 | NR | 42 | 1.18 | 0.17 | 0.32 |
| 10 | Okonofua | 28.6 | 17.2 | 60.3 | 5.2 | 97.7 | NR | 39.6 | 1.75 | 0.56 | 0.18 |
| 11 | Olusanya | NR | NR | 64 | 6.2 | 98.4 | NR | 146.7 | 0.84 | −0.17 | 0.19 |
| 12 | Suleiman | NR | NR | NR | NR | NR | 53.8 | 46.9 | 2.10 | 0.74 | 0.26 |
| 13 | Welegebriel | NR | NR | 64.3 | NR | NR | NR | NR | 3.19 | 1.16 | 0.36 |
| 14 | Yadeta | 26.59 | 44.14 | NR | NR | 95.7 | 47 | 85.3 | 1.79 | 0.58 | 0.27 |
- Abbreviations: NR, not reported; proporn, proportion.
Two of the studies34, 39 reported protective association of advanced age (≥35 years) in resulting stillbirth relative to 20–35 age groups though they are not statistically significant. The other 12 studies showed a risk association of advanced age on stillbirth. Their OR ranges from 1.0337 to 4.06.16 Among these, five of them are not statistically significant17, 37, 38, 40, 41 (Table 2).
3.5 Synthesis of results
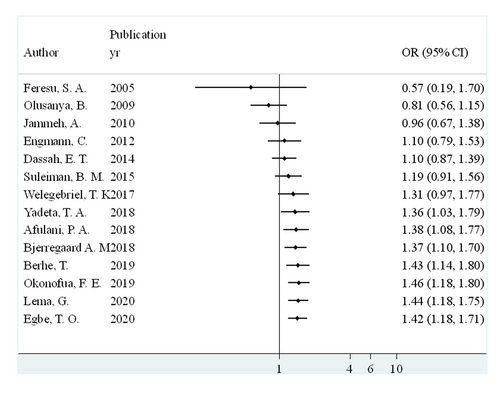
3.5.1 The effect of maternal age on stillbirth
The pooled OR of advanced maternal age (≥35 years) on stillbirth, as the forest plot (Figure 3) displays, is 1.42 (1.18, 1.71) when compared with the age group of 20–35 years. The Cochran's Q test revealed the presence of heterogeneity with significant χ2 statistics (Q = 28.79 (df = 13) p = 0.007). This heterogeneity is quantified by I2 statistics which became I2 = 54.9% (p = 0.007) which can be classified as moderate heterogeneity.30
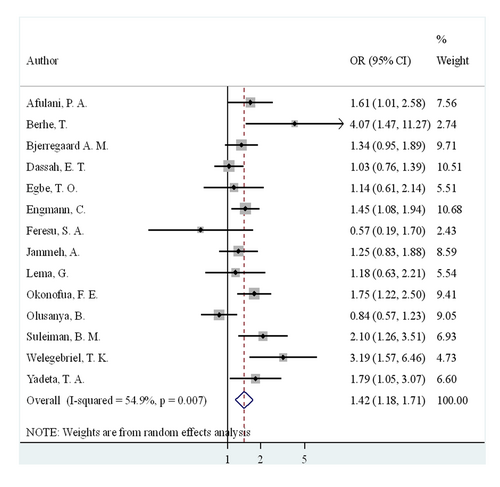
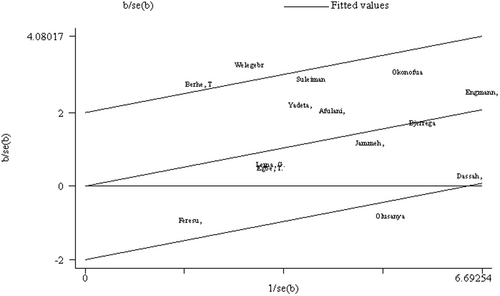
The absence of considerable heterogeneity can also be seen subjectively from the forest plot as most of the studies have overlapping intervals (Figure 3) and from the Galbraith plot (Figure 4) as most of the studies lie with in the 95% CI.
3.6 Risk of bias across studies
Funnel plot (Figure 5): We consider the presence of publication bias or small studies effect if the distribution of the studies about the funnel is asymmetric. Whereas we have got more or less symmetric distribution which indicates the absence of publication bias.
3.6.1 Egger's and Begs test
Egger's test
The graphical presentation (Figure 6) as well as the statistical finding of the Egger's test (p = 0.287) (Table 3) indicate no publication bias in the favor of the Funnel plot's result. The graph shows no publication bias because the intercept of the regression line is with in the 95% confidence and not far from zero.
| Number of studies = 14 | Root MSE = 1.474 | |||||
| Std_Eff | Coef. | Standard error | t | p > |t| | [95% confidence interval] | |
| Slope | 0.0387622 | 0.2594442 | 0.15 | 0.884 | −0.526518 | 0.6040425 |
| Bias | 1.28959 | 1.156166 | 1.12 | 0.287 | −1.229479 | 3.808658 |
- Note: Test of H0: No small-study effects. p = 0.287.
Begg's test (Table 4)
The result of Begg's test (p = 0.477) also supports the finding of funnel plot and Egger's test which is the absence of publication bias.
| adj. Kendall's score (P–Q) | = | 13 |
| Standard deviation of score | = | 18.27 |
| Number of studies | = | 14 |
| z | = | 0.71 |
| Pr > |z| | = | 0.477 |
| z | = | 0.66 (continuity corrected) |
| Pr > |z| | = | 0.511 (continuity corrected) |
3.7 Cumulative meta-analysis
The cumulative meta-analysis as indicated in Figure 7 showed that the effect of advanced maternal age on stillbirth had a little increment from year to year as a new study is added to the previous ones.
4 DISCUSSION
The objective of this systematic review and meta-analysis was to assess the effect of advanced maternal age on experiencing stillbirth.
This review found out that advanced maternal age is a risk factor for stillbirth with the OR of 1.42. That means, the odds of experiencing stillbirth among women whose age is greater than 35 years will increase by 42% when compared with those in the age group of 20–35 years.
This finding is consistent with some guidelines and systematic reviews. Queensland Clinical Guideline for maternity and neonatal care42 stated that maternal age over 35 years is a risk factor for stillbirth though it described nothing about the magnitude of the risk. Another inline systematic review revealed that women with advanced maternal age have an increased risk of stillbirth with a relative risk range of 1.20–1.53 though it was not pooled estimate.43
Meta-analysis of six studies from high income countries44 also showed an inline risk of association (OR = 1.65) between maternal age older than 35 years and experience of stillbirth.
The review additionally revealed that the cumulative effect of getting pregnant at advanced age on stillbirth was slightly increasing from year to year. This can be caused by the effect of increased power of the cumulation as it increases the sample size and the proportion of the stillbirth while one study is added on the previous ones.
Age-related pregnancy outcomes are caused by a progressive decline in the number and quality of oocytes as mother age increases.45 During the reproductive years, atresia persists, progressing at a faster pace after the age of 37 in the average woman. The quality of oocytes reduces as the number of oocytes decreases, finally reaching a point where conception is unachievable. An increase in the proportion of aneuploid oocytes is the primary cause of the decline in quality.46 Autosomal trisomy is the most common type of nondisjunction, and it's assumed to be linked to age-related alterations in the meiotic spindle.47
In addition to ovarian variables, older women are more likely to have underlying medical pathology, such as endometriosis, fibroids, tubal disease, and polyps, which can make it difficult for successful conception.48 These and other diseases may raise the chances of a stillbirth in a woman of advanced maternal age.
Multiparous women in developing nations are more likely to become pregnant at an advanced maternal age for a variety of reasons, including lack of or ineffective family planning, poverty, and cultural preferences for many children.49 So, it has a public health as well as clinical implications in which all stakeholders should consider.
5 CONCLUSIONS
The rate of stillbirth in Africa ranges from 15 to 146.7 per 1000 births. Advanced maternal age is a risk factor for stillbirth with the OR of 1.42. That means, the odds of experiencing stillbirth among women whose age is greater than 35 years will increase by 42% when compared with those in the age group of 20–35 years. Additionally, that the cumulative effect of getting pregnant at advanced age on stillbirth was slightly increasing from year to year.
6 RECOMMENDATION
The countries' higher health departments should develop guidelines (or update the existing ones) incorporating the risk experiencing stillbirth while getting pregnant at the advanced ages.
Health information communication (HIC) on the risk of getting pregnant at the advanced ages on stillbirth should be well addressed to all women of reproductive age group and the health professionals whose work is related to maternal and reproductive health by the concerned higher health department of the countries.
Women in their 20s and 30s ought to get age-related stillbirth risk counseling. For these women, preconception counseling on the risks of stillbirth with advanced maternal age should be taken into consideration.
7 STRENGTHS
The studies in this meta-analysis are not highly heterogeneous; rather, they are close to moderately heterogeneous (I2 = 54%), which is one of its main advantages. The fact that the included studies span the entire continent is another glaring strength except the northern ones (Figure 2).
8 LIMITATIONS
The effect of residual confounding is a well-known drawback of meta-analysis of observational data. One of the review's limitations was that it only covered English publications and reports.
9 ETHICS STATEMENT
Even though it is not a mandatory as well as a requirement, letter of ethical clearance was secured from Research Ethical Review Committee of Wollo University College of Medicine and Health Sciences to be abided by the principle of the college. The informed consent and confidentiality were considered to be addressed by the authors of the primary studies.
AUTHOR CONTRIBUTIONS
Mengistu Abate: Conceptualization; formal analysis; investigation; methodology; project administration; software; supervision; writing—original draft; writing—review & editing. Mastewal Arefaynie: Resources; visualization. Amare Muche: Data curation; resources; validation. Asressie Molla: Conceptualization; methodology; writing—review & editing. Shambel Wodajo: Conceptualization; methodology; writing—review & editing. Kibir Temesgen: Data curation; investigation; resources. Zinabu Fentaw: Data curation; investigation. Zenebe Tefera: Data curation; investigation; resources. Tesfa D. Habtewold: Conceptualization; methodology; supervision; writing—review & editing. All authors have read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Mengistu Abate affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that supports the findings of this study are available in the Supporting Information of this article. Mengistu Abate had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.




