A novel referral strategy to enhance the enrollment of patients with heart failure in cardiac rehabilitation: A feasibility study
Abstract
Background and Aims
Rehabilitation targeting patients with cardiac conditions are evident and acknowledged in clinical guidelines. However, participation rates remain suboptimal, with only 50% of all patients with cardiac conditions participating in these programs across Europe. Considering the well-documented effects of rehabilitation, increasing the referral rate to cardiac rehabilitation would be desirable. This study aimed to evaluate the feasibility of a novel referral strategy that could potentially enhance enrollment in cardiac rehabilitation for patients with heart failure.
Methods
This prospective feasibility study incorporating both quantitative and qualitative methods was conducted in an outpatient heart failure clinic and a municipal health care center. 106 patients with heart failure were referred to the heart failure clinic from September 2021 through July 2022. A 15−20 min face-to-face physiotherapy consultation was incorporated into usual care, evaluating patients' habitual and actual level of functioning, disability, and physical activity and assessing their potential need and motivation for cardiac rehabilitation. Three predefined quantitative feasibility outcomes: reach, referral rate, and data completeness were assessed. Additionally, semi-structured interviews explored acceptability among patients and health care professionals at the municipal health care center and the hospital. Finally, the potential effect was assessed based on the enrollment rate.
Results
Physiotherapy consultations were offered to 86% of eligible patients; of these, 52% were referred to cardiac rehabilitation. Ninety-one percent data completeness was achieved. The intervention was well-accepted by patients and health care professionals. The enrollment rate reached 79%.
Conclusion
The novel referral strategy proved feasible concerning reach and data completeness, although the referral rate suggested that further refinements are required before a full-scale trial. The novel referral strategy was well-accepted, and enrollment rate approached an acceptable level.
1 INTRODUCTION
Rehabilitation targeting patients with cardiac conditions are evident and acknowledged in clinical guidelines.1-3 Therefore, most European countries have implemented cardiac rehabilitation programs.4 However, participation rates remain suboptimal, with only 50% of all patients with cardiac conditions participating in these programs across Europe.5
Various facilitators and barriers to participation in cardiac rehabilitation exist, encompassing patient-related factors such as coping strategies and support from relatives, service-level factors that involve health care professional-related aspects, and structural factors like geographic or economic accessibility of cardiac rehabilitation programs.3, 6, 7 However, patient referral is a crucial prerequisite for successful cardiac rehabilitation participation.8 Furthermore, research indicates that successful referral appears less influenced by patient-related factors and more strongly associated with service-level factors, such as health care professionals' understanding and advocacy of cardiac rehabilitation.6, 9
In the Danish model, referral of patients with cardiac conditions to cardiac rehabilitation is typically the responsibility of the discharging hospital, while delivery is primarily the responsibility of the patient's municipal of residence.10 The transition to cardiac rehabilitation has shown to be critical in terms of dropout.11 The referral procedure is primarily overseen by physicians or nurses who possess expertize in addressing cardiac conditions in terms of symptoms and medication but may have limited knowledge about cardiac rehabilitation.3, 12 Expertize within cardiac rehabilitation typically falls within the domain of the physiotherapy profession, making them crucial stakeholders in cardiac rehabilitation.
Although systematic assessment of rehabilitation needs for all patients with heart failure is recommended,13 fewer than 50% are currently referred.14 Considering the well-documented effects of rehabilitation,2, 3, 7 increasing the referral rate to cardiac rehabilitation would be desirable. Hence, a novel referral strategy was developed at Silkeborg Regional Hospital to improve cardiac rehabilitation enrollment for patients with heart failure. The rationale underpinning the novel referral strategy was informed by existing evidence, recognized principles of health education15-17 and the International Classification of Functioning, Disability and Health (ICF),18 and in addition involvement of multidisciplinary health care professionals from the municipal health care center and the heart failure clinic. Patients with heart failure have a severe manifestation of cardiac disease and a pressing need of long-term cardiac rehabilitation and care, emphasizing the importance of successful enrollment.14
Therefore, this study aimed to evaluate the feasibility of a novel referral strategy that could potentially enhance enrollment in cardiac rehabilitation for patients with heart failure.
2 METHODS
2.1 Design
This prospective feasibility study used quantitative and qualitative methods.19 The study was reported according to the CONSORT Statement: extension to randomized pilot and feasibility trials.20 According to Danish legislation and the Act on Biomedical Research Ethics Committee System in Denmark, research using questionnaires or register based research without human biological material does not require approval from an ethics committee (§14 Section 2).21 In accordance with the guidelines of the Danish Data Protection Agency, the hospital management at Regional Hospital Central Jutland granted permission for data collection from electronic medical records. Sensitive personal information was securely stored in RedCap and MidtX (a secure regional digital platform). All informants provided written informed consent to participate in the interviews
2.2 Setting and participants
The study was conducted in Denmark, where health care services, including rehabilitation, are financed through taxation, ensuring free and equal access for all citizens.
In Denmark, it is recommended that cardiac rehabilitation is provided by a multidisciplinary team twice a week for 30−60 min over a span of 12−26 weeks.13 The patients attending cardiac rehabilitation in the present study were provided sessions twice a week for 60 min over a 12-week period by a multidisciplinary team. As per the guideline, the cardiac rehabilitation encompassed physical exercise, patient education, psychosocial support (including job retention), assistance for dietary changes, support for smoking cessation, optimization of medication, and clinical follow-up with a focus on maintaining goals.13 Patients were recruited from the heart failure clinic, an outpatient clinic within the Diagnostic Center at Silkeborg Regional Hospital. Patients with heart failure were referred to this clinic from general practice, other outpatient clinics, or following hospitalization. According to the Danish national clinical guideline on cardiac rehabilitation13 it is considered good practice that patients with heart failure are systematically assessed for participation in cardiac rehabilitation. For that reason, all patients meeting the following inclusion criteria were included from September 2021 through July 2022: (1) age ≥ 18 years, (2) diagnosed with heart failure within the last 4 weeks, and (3) no previous consultation in the heart failure clinic.
2.3 Interventions
In the usual care setting in the heart failure clinic preceding the feasibility study, a nurse had 45 min to discuss diet, smoking, alcohol, and physical activity with the patient. With the novel referral strategy, physiotherapy was integrated into usual care which meant that the nurse's consultation time was reduced to 30 min since the physiotherapist now addressed physical activity, exercise, and rehabilitation in a separate 15-min session. Despite the integration, patients still received a 45-min consultation, with both health professionals addressing the same issues from their distinct backgrounds and expertize. Table 1 presents the intervention description inspired by the Template for Intervention Description and Replication (TIDieR) checklist.22 Additionally, a logic model was developed to outline the novel referral strategy, detailing the planned work and intended results, which served as a guide for research questions and methodologies24 (Supporting Information: Appendix 1).
|
A novel referral strategy to improve the enrollment of patients with heart failure in cardiac rehabilitation. |
|
The rationale behind integrating physiotherapy consultations was based on a combination of the following:
Further, the novel referral strategy was based on existing evidence, and experiences and insights of health care professionals from both the municipal health care center and the heart failure clinic. |
|
A dialogue guide based on principles of health education and ICF (see Item 2) was developed to support the physiotherapy consultation. In addition, patients were given a pamphlet describing the cardiac rehabilitation programs provided in the municipal health care center and the hospital, respectively. Finally, for patients preferring home-based exercise, an individual exercise program was designed in collaboration with the patient. A telephone list was provided to the health professionals at both sites to facilitate communication between the municipal health care center and the heart failure clinic. The research team and health care professionals at both sites agreed on predefined variables for standardized reporting in the electronic medical record. |
|
By combining knowledge from the principles of health education and ICF (see Item 2), the physiotherapist could assess patient's habitual and actual level of functioning, disability, and physical activity, and assess their potential need and motivation for cardiac rehabilitation. Patients who accepted the offer of cardiac rehabilitation were referred to a cardiopulmonary exercise test as part of risk stratification. The test was performed some days/weeks later at the hospital, supervised by a physiotherapist and a nurse with the use of Electrocardiography and blood pressure monitoring. Patients classified with intermediate risk (stable hemodynamics, absence of angina and significant ST depression, absence of failure symptoms during the test, and absence of significant arrhythmia) were referred to cardiac rehabilitation in the municipal health care center (group or individual rehabilitation), and patients classified with high risk were referred to the hospital (group rehabilitation).23 If the patient was not eligible for either of these options or declined, the physiotherapist initiated a discussion of the patient's motivation for physical activity and/or home-based exercises. Patients were offered a follow-up telephone consultation after 14 days and three months to adjust their exercise program and motivate them to continue with their exercise program. |
|
The six physiotherapists providing the physiotherapy consultation participated in a refresher session covering the principles of health educational and ICF. They were also introduced to the materials described in Item 3. |
|
All physiotherapy consultations were face-to-face, with the exception of follow-up telephone consultations offered to patients performing home-based exercises. |
|
Consultation rooms were located at the heart failure clinic, Silkeborg Regional Hospital. |
|
The physiotherapy consultation lasted 15 min, and was provided following the nurse consultation which lasted 30 min. |
|
The same dialogue guide was employed for each physiotherapy consultation; however, variations arose as the intervention was adjusted to accommodate patients' specific needs. |
2.4 Feasibility outcomes
To assess the feasibility of the novel referral strategy, three predefined quantitative feasibility progression criteria were selected, and classified using a traffic light system.25 Accordingly, green indicates proceeding as planned, amber suggests proceeding with amendments, and red signifies that issues must be addressed before moving forward or halting the process altogether (Table 2). The first feasibility outcome, reach, was defined as the proportion of eligible patients offered a physiotherapy consultation.26 The second feasibility outcome, referral rate, represented the number of patients who received a physiotherapy consultation and were subsequently referred to cardiac rehabilitation. The third and final feasibility outcome pertained to data completeness in relation to cardiac rehabilitation on (1) enrollment (participant attendance at initial visit), (2) adherence (participating in at least 80% of the cardiac rehabilitation sessions27), and (3) completion (participant attendance at the final evaluation). Data on reach was collected from the Patient Administrative System, and data on referral rate was collected from the electronic medical record. Data completeness on enrollment, adherence and completion was collected from the electronic medical record post cardiac rehabilitation. As no formal cut-off criteria exist in terms of reach and data completeness,25 the authors collaboratively determined these thresholds based on what they deemed adequate data quality to ensure valid results in a full-scale trial. The cut-off for referral rate was chosen in accordance with the latest Danish clinical guideline for cardiac rehabilitation, which recommends that all patients with heart failure are systematically assessed for participation in cardiac rehabilitation,13 and a Danish study revealing that approximately 50% of patients with heart failure are referred to cardiac rehabilitation.14 Table 2 shows the predefined green, amber and red criteria for each feasibility outcome.
| Feasibility outcome | Green | Amber | Red |
|---|---|---|---|
| Proceed | Proceed with amendments | Issues must be solved before proceeding or not proceeding | |
| Reach | ≥80% | 60−79% | <60% |
| Referral rate | ≥75% | 50−74% | <50% |
| Data completeness | ≥80% | 60−79% | <60% |
2.5 Qualitative process evaluation
Inspired by the Medical Research Council's guidance on process evaluation of complex interventions, a qualitative process evaluation was incorporated into the study to explore the perspectives of patients receiving the physiotherapy consultation and health care professionals delivering it.26 The assessment of the novel referral strategy's acceptability encompassed these perspectives. A semi-structured interview guide was employed, drawing inspiration from two of the three key functions of a process evaluation: mechanism of impact, which involves patients' responses to and interaction with the intervention and/or any unanticipated pathways and consequences, and context which pertains to contextual factors that affect and may be affected by implementation, intervention mechanisms, and outcomes.26 Individual interviews were conducted with four patients, by telephone, three to 6 months after the consultation in the heart failure clinic. The patients were selected from the quantitative study population using stratified purposeful sampling; two were referred to the municipal health care center (group and individual rehabilitation), one was referred to the hospital (group rehabilitation), and one performed home-based exercises. In the semi-structured interview guide for patients, predefined themes included perspectives on (1) the content of the physiotherapy consultation, such as the assessment of the need for cardiac rehabilitation and the information provided about it, and (2) the timing of the physiotherapy consultation as well as the period following the physiotherapy consultation, which encompassed aspects like participation in and adherence to cardiac rehabilitation. Additionally, approximately 6 months after the study commenced, we conducted two individual interviews with health care professionals from the municipal health care center (two physiotherapists), along with a focus group that included a convenience sample of three health care professionals from the heart failure clinic (two nurses and a physiotherapist) at their respective workplaces. The predefined themes in the semi-structured interview guides for the health care professionals included perspectives on (1) the integration of physiotherapy consultations in usual care, such as collaboration in the multidisciplinary team, changes to multidisciplinary and cross-sectoral teamwork and patient feedback, (2) organization, in terms of time consumption, and coherence of the patient pathway, and (3) recommendations for modifications to the novel referral strategy. Three different researchers conducted the interviews and facilitated the focus group.
Telephone interviews and the focus group at the heart failure clinic were documented through extensive notes, and the interviews in the municipal health care center were recorded and transcribed verbatim.
2.6 Potential effect
The potential effect of the intervention was evaluated by assessing the enrollment rate, defined as participant attendance at the initial visit in the cardiac rehabilitation program. The predefined cut-off for an acceptable enrollment rate was 80%. Data was collected from the electronic medical record.
2.7 Sample size
Regarding sample size, our objective was not to achieve statistical power. Instead, we chose an inclusion period of approximately 1 year to accommodate organizational and seasonal variations while considering available resources. This period was considered suitable for capturing a broad representation of the target population, generating sufficient data on feasibility, and accounting for potential dropouts.
2.8 Data analyses
Feasibility outcomes and potential effect were analyzed descriptively and presented with mean,standard deviations (SD), median, interquartile range, numbers, and proportions. STATA 17 (V.17 Stata) was used for data management and analysis.
In the qualitative analysis, acceptability was analyzed employing principles of thematic analysis, following a three-step approach to organize and interpret data.28 First, an inductive approach was used for the initial coding, allowing for openness to unexpected findings and emerging new themes. Second, categories were developed and refined, leading to the identification of overarching themes. To ensure validity and accuracy in data interpretation, two researchers independently reviewed and assessed the data and collaboratively reassessed the final interpretations during the data condensation process.29
3 RESULTS
3.1 Patient characteristics
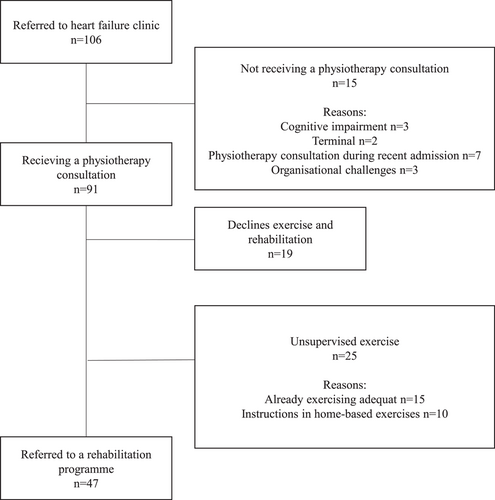
106 patients were referred to the heart failure clinic, with 91 receiving the physiotherapy consultation. Of these, 19 patients declined any exercise or cardiac rehabilitation. Another 25 patients were not referred to cardiac rehabilitation, 15 of these because they already participated in suitable exercise activities (e.g., cardiac rehabilitation or exercise activities at their local club). The remaining 10 preferred home-based exercises. In total, 47 patients were referred to cardiac rehabilitation in the municipal health care center (group rehabilitation: n = 27; individual rehabilitation: n = 9) or at the hospital (group rehabilitation: n = 11) (Figure 1).
The mean age was 73 years (range 42−92), and the majority were men with a left ventricular ejection fraction (LVEF) below 40% (Table 3).
| All patients | Declines cardiac rehabilitation | Referred to cardiac rehabilitation | Unsupervised exercise | |
|---|---|---|---|---|
| n = 91 | n = 19 | n = 47 | n = 25 | |
| Age (mean, SD) | 73 (12) | 75 (11) | 72 (8) | 73 (15) |
| Gender (female) n (%) | 33 (36) | 8 (42) | 17 (36) | 8 (32) |
| Marital status n (%) | ||||
| Married | 50 (55) | 11 (58) | 31 (66) | 8 (32) |
| Unmarried, divorced, or widow(er) | 41 (45) | 8 (42) | 16 (34) | 17 (68) |
| Multimorbidity | ||||
| <2 | 1 (1) | 0 (0) | 1 (2) | 0 (0) |
| ≥2 | 90 (99) | 19 (100) | 46 (98) | 25 (100) |
| Left ventricular ejection fraction (LVEF) n (%) | ||||
| ≤40% | 79 (87) | 14 (74) | 42 (96) | 20 (80) |
| >40% | 12 (13) | 5 (26) | 2 (4) | 5 (20) |
| New York Heart Association (NYHA) n (%) | ||||
| Classification I | 32 (35) | 4 (21) | 20 (43) | 8 (32) |
| Classification II | 45 (50) | 10 (53) | 23 (49) | 12 (48) |
| Classification III | 13 (14) | 4 (21) | 4 (9) | 5 (20) |
| Classification IV | 1 (1) | 1 (5) | 0 (0) | 0 (0) |
3.2 Progression criteria
Based on the predefined progression criteria, reach was classified as green, referral rate as amber, and data completeness as green (Table 4).
| Feasibility outcome | Green | Amber | Red |
|---|---|---|---|
| % (n/N) | % (n/N) | % (n/N) | |
| Reach | 86% (91/106) | ||
| Referral rate | 52% (47/91) | ||
| Data completeness | |||
| Enrollment | 91% (43/47) | ||
| Adherence | 89% (42/47) | ||
| Completion | 91% (43/47) |
3.3 Qualitative process evaluation results
Drawing from the interviews on acceptability, several themes emerged. First, patients positively described the timing and content of the physiotherapy consultation. The health care professionals from the municipal health care center also held favorable views. However, they experienced an increase in patients participating in preliminary clarifying interviews before commencement of cardiac rehabilitation without being motivated for subsequent participation in cardiac rehabilitation. Furthermore, they expressed a preference for continuous meetings rather than email correspondence to discuss the feasibility study and its progress. Such meetings were believed to strengthen commitment to the study (e.g., ensuring accurate documentation) and enhance cross-sectoral collaboration in general. Lastly, the health care professionals at the heart failure clinic found the focus on physical activity, induced by the novel referral strategy, advantageous. They also experienced increased multidisciplinary teamwork and continuity in the patient pathway across sectors. More details on acceptability, summarized themes and citations are shown in Table 5.
| Theme | Results |
|---|---|
| Individual interviews with patients (n = 4) | |
| “Focus on physical activity” | Patients positively described the physiotherapy consultation and appreciated the focus on physical activity. |
| “The physiotherapist convinced me that I had to get physically strong…I was already walking, but I hadn't thought of getting the heart rate up.” | |
| “Timing of the physiotherapy consultation, and the period following the consultation” | Three patients agreed that the timing of the physiotherapy consultation was appropriate. |
| “I think it was correctly scheduled, according to timing, right after the nurse consultation.” | |
| One patient preferred that it be later due to a referral for additional medical assessment at another hospital. | |
| Individual interviews with the health care professionals from the municipal health care center (n = 2) | |
| “Integration of physiotherapy consultations” “Organization” and “Recommended modifications” | The health care professionals from the municipal health care center did not experience any remarkable workflow changes due to the novel referral strategy (e.g., work tasks and the number of referred patients). However, they reported a tendency towards a higher rate of patients declining cardiac rehabilitation after the preliminary clarifying interview in the study period. |
| “They (the patients) probably wanted to meet the expectations from the physiotherapist at the heart failure clinic and accepted referral to the municipal health care center may be they even participated in the preliminary clarifying interview at the municipal health care center, and then regretted before the initial rehabilitation session.” | |
| The novel referral strategy was experienced as advantageous for the municipal health care center as it seems to be offered to the patients who needed it the most. The health care professionals had no suggestions for modifying the novel referral strategy. Still, they asked for better communication with the heart failure clinic to strengthen the cross-sectoral teamwork if a full-scale trial is conducted. | |
| Focus group with health care professionals from heart failure clinic (n = 3) | |
| “Focus on physical activity” and “Multidisciplinary teamwork” | The health care professionals from the heart failure clinic concurred that the intervention fostered a heightened emphasis on physical activity, increased multidisciplinary teamwork, and improved the quality of service in the heart failure clinic. In addition, the nurse perceived enhanced continuity in the patient pathway and felt that more patients accepted the offer of cardiac rehabilitation when a physiotherapist focused on disability, physical activity, and cardiac rehabilitation during the consultation. |
| “It created a natural connection when the physiotherapist conducted the consultation on physical activity. I am convinced this continuity made sense for the patients.” | |
| “Logistics” | During the study period, there were logistical challenges regarding consultation rooms. However, the health care professionals showed great willingness to solve this in the future. |
3.4 Potential effect
Regarding the potential effect of the novel referral strategy, 47 patients were referred to cardiac rehabilitation. Of those, four patients were lost to follow-up without data in the electronic medical record on enrollment, adherence or completion, and six patients did not start cardiac rehabilitation, resulting in an enrollment rate of 79% (37/47).
4 DISCUSSION
The novel referral strategy was found feasible in terms of reach and data completeness, while the referral rate indicates the need for some adjustments before proceeding to a full-scale trial. Nevertheless, patients and health care professionals perceived the novel referral strategy as acceptable, and the potential effect, expressed through the enrollment rate, was close to acceptable.
In total, 86% of the intended population were offered the physiotherapy consultation, classifying reach as green. Reasons not receiving the physiotherapy consultation were patient-related (e.g., cognitive impairments or terminal illness) or service-level related (e.g., the physiotherapists being ill or on holiday). Data completeness was similarly classified as green without reminding the health care professionals at the municipal health care center to report data. Reminders at the end of the study enhanced the rates of data completeness.
Of those receiving a physiotherapy consultation, only 52% were referred to cardiac rehabilitation. Thus, the referral rate was classified as amber. The novel referral strategy ensured that all patients with heart failure were systematically assessed regarding participation in cardiac rehabilitation as recommended in the latest Danish clinical guideline.13 Despite this, the novel referral strategy did not enhance the referral rate above the mean referral rate of 50% for patients with heart failure in Denmark, most recently estimated in 2018.14 The study, as mentioned above, defines a referral as whether the patient was referred to or started cardiac rehabilitation.14 In contrast, our study defined the referral rate as the number of patients referred to cardiac rehabilitation. For that reason, a direct comparison to our estimate is not possible. Nevertheless, the Danish estimates are much higher than those from the United Kingdom, with around 15% of patients with heart failure being referred to cardiac rehabilitation.5 An unexpected finding was the many patients who expressed a preference for unsupervised exercise (n = 25). In hindsight, whether the predefined cut-off criteria for referral rate of 75% was too ambitious can be discussed. Also, it can be questioned whether the effects of unsupervised exercise are the same as participation in an evidence-based cardiac rehabilitation program (i.e., offering exercise, education, risk factor management, and psychological counseling).1 Considering the increased focus on patient-centered interventions in health care and the urgent need to support models of delivery to improve access and uptake of cardiac rehabilitation, new models of cardiac rehabilitation as for example offering evidence-based heart failure-specific home-based cardiac rehabilitation program like the REACH-HF30 or digitally supported models of delivery is worth paying attention to in a future full-scale trial.3
The qualitative findings showed positive perception of the novel referral strategy by patients and health care professionals. However, the health care professionals from the municipal health care center raised a concern regarding an increased number of patients who participated in the preliminary clarifying interview without being motivated for subsequent participation in cardiac rehabilitation. This means the patients were registered as enrolled but did not adhere to or complete the program. Hence, implementing a systematic referral strategy, like in our study, may increase the need for a strategy to enhance enrollment and completion of cardiac rehabilitation at the municipal health care center. Otherwise, the effort of referring patients could be wasted. Additionally, the health care professionals from the municipal health care center requested continuous meetings about the feasibility study and its progress. This will be integrated into a full-scale trial.
The potential effect of the novel referral strategy, expressed as the enrollment rate, was predefined as acceptable if it reached 80%, a very ambitious cut-off. Recently, a Danish study showed that 25% of referred patients with ischaemic heart disease did not enroll in cardiac rehabilitation.31 In contrast, another Danish study estimated that approximately 50% of eligible patients with heart failure are enrolled in cardiac rehabilitation.14 In the United Kingdom, a report from 2019 showed that approximately 50% of eligible patients with various cardiac conditions, except heart failure, are enrolled in cardiac rehabilitation.5 However, even fewer patients with heart failure are enrolled in cardiac rehabilitation.5 Hence, the enrollment of patients with heart failure in cardiac rehabilitation continues to be a significant challenge.5 In light of these results, reaching an enrollment rate of 79% in our study seems more than acceptable.
A review from 2019 assessed interventions provided to increase the enrollment of patients with various cardiac conditions, including heart failure.1 The review found that multiple interventions to increase enrollment were indeed successful, resulting in 27% greater enrollment than observed with usual care. The review revealed that the provider (i.e., nurse or allied health care provider, e.g., physiotherapist), and face-to-face intervention delivery positively influenced the enrollment rate. Heterogeneity was found to be substantial, and further research was recommended. Therefore, findings from this review1 support the planning of a full-scale trial assessing the effect of the novel referral strategy that a physiotherapist delivers face-to-face. Before proceeding to a full-scale trial, specific attention will be paid to managing the large group of patients requesting unsupervised exercise and enhancing communication across sectors.
The study's strengths include the thorough development of the novel referral strategy and the study design based on existing evidence, theory, and the involvement of health care professionals as a substantial part of the modeling of processes and outcomes.32 Furthermore, by combining quantitative data relating to progression criteria and thoroughly collecting qualitative data on acceptability, we gained comprehensive and clinically relevant knowledge about the intervention's feasibility, facilitating decision-making about whether to proceed to a full-scale trial, even though not all progression criteria were met. Limitations of the study are the lack of comparative data on the enrollment rate reached by usual care and the single-center setup, which restricts generalizability. Finally, a fully powered randomized controlled trial is needed to determine the effect of the novel referral strategy.
A novel referral strategy integrating physiotherapy consultations into usual care to enhance enrollment in cardiac rehabilitation is feasible. Patients and health care professionals accepted it, contributing to promising results. Thus, the novel referral strategy may be one way to increase enrollment in cardiac rehabilitation effectively; however, a subsequent randomized controlled trial amending the intervention according to the predefined referral progression criteria will determine whether the novel referral strategy is superior to usual care in improving enrollment in cardiac rehabilitation.
AUTHOR CONTRIBUTIONS
Anne Mette Schmidt: Conceptualization; data curation; formal analysis; methodology; supervision; writing—original draft; writing—review and editing. Jannie Rhod Bloch-Nielsen: Conceptualization; data curation; formal analysis; writing—original draft; writing—review and editing. Helene Nørgaard: Conceptualization; data curation; formal analysis; writing—original draft; writing—review and editing. Loui Hannibal: Conceptualization; formal analysis; writing—review and editing. Sarah Holm Junge Jensen: Data curation; formal analysis; writing—review and editing. Lars Hermann Tang: Data curation; formal analysis; methodology; supervision; writing—original draft; writing—review and editing. Nanna Rolving: Data curation; formal analysis; methodology; supervision; writing—original draft; writing—review and editing.
ACKNOWLEDGMENTS
The authors are grateful to all participants and the health care professionals from the municipal health care center and the heart failure clinic, who made this study possible. In addition, we thank data manger Andrew Bolas and language editor Eileen Dorte Shanti Connelly for their assistance. No grant was received from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
According to Danish legislation and the Act on Biomedical Research Ethics Committee System in Denmark, research using questionnaires or register based research without human biological material does not require approval from an ethics committee (§14 Section 2). In accordance with the guidelines of the Danish Data Protection Agency, the hospital management at Regional Hospital Central Jutland granted permission for data collection from electronic medical records. All informants provided written informed consent to participate in the interviews.
TRANSPARENCY STATEMENT
The lead author Anne Mette Schmidt affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.