Imposter phenomenon in physical therapists: A cross-sectional observational study
Abstract
Background and Aims
Imposter phenomenon (IP), or perceived fraudulence, describes an ongoing fear of exposure as a fraud or imposter, despite objective successes and accomplishments. Although there is a growing interest of IP in medicine, IP in the physical therapy profession has been minimally examined. We aimed to determine the prevalence and predictors of IP among licensed physical therapists in the United States.
Methods
This cross-sectional observational study utilized an online survey to assess levels of IP using the Clance Imposter Phenomenon Scale. We assessed degrees of emotional exhaustion and job satisfaction and collected professional and demographic information. A multivariable logistic regression model examined factors associated with IP presence.
Results
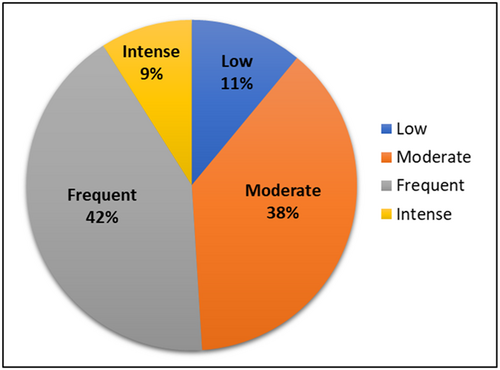
The mean IP score was 60.3 (SD: 15.1, range: 19–95). Fifty-five respondents (10.7%) had low IP, 196 (38.1%) moderate, 215 (41.8%) frequent, and 48 (9.3%) intense IP. The prevalence of IP, defined as frequent or intense IP, was 51.2%. Having manager/supervisor experience (odds ratio [OR] = 0.55, 95% confidence interval [CI] = 0.34–0.90) was associated with a reduced odds of IP presence. Holding a bachelor's or master's degree (vs. Doctor of Physical Therapy (DPT); OR = 2.31, 95% CI = 1.07–5.00), a history of or current mental health diagnosis (OR = 2.77, 95% CI = 1.69–4.54), and emotional exhaustion (moderate vs. low: OR = 5.37, 95% CI = 2.11–13.69; high vs. low: OR = 14.13, 95% CI = 5.56–35.89) were each associated with an increased odds of IP presence.
Conclusions
IP is highly prevalent among licensed physical therapists. Seasoned clinicians with managerial roles seemed to be less susceptible to IP, whereas those with mental health diagnoses, emotional exhaustion, and those without a DPT degree may be more susceptible. Given its high prevalence and potential negative impact on burnout and career advancement, it is crucial to increase IP awareness and provide education on management strategies.
1 INTRODUCTION
Imposter phenomenon (IP), or perceived fraudulence, describes an ongoing fear of exposure as a fraud or imposter, despite objective successes and accomplishments.1 Those with IP tend to attribute their achievements to luck or good timing and question their professional legitimacy and expertise.
A 2020 systematic review2 outlined the prevalence, predictors, and potential treatment of this long-recognized phenomenon that impacts approximately 70% of working professionals at some point in their career. IP was strongly correlated with depression and anxiety, poor work performance, job dissatisfaction, and burnout, particularly among ethnic minority groups.2 Their findings suggested those affected may be limited in achieving their full professional potential and are more likely to experience burnout and a decline in psychological well-being.
Healthcare professionals are prone to experiencing IP due to the demanding nature of their work. The combination of high care standards, long working hours, continuous learning expectations, and emotional stress of dealing with challenging situations creates a constant pressure to excel and fear of falling short. One in four physicians reported frequent or intense IP.3 Poor mental health, higher level of burnout, and lower job satisfaction have been cross-sectionally linked to greater IP among medical students and practitioners.3, 4 However, the role of sex, gender, and years of work experience remains inconclusive.3-8
Despite the growing interest of IP in medicine, IP in the physical therapy profession has been scantly examined. The prevalence of IP was 35% in a sample of 200 physiotherapists in India.5 Among 106 physical therapy students in Slovenia, 38% had frequent or intense IP.6 More advanced age, greater years of study, and having clinical work experience appeared to be associated with lower IP in these students,6 although no multivariable analysis was conducted to control for the effects of other factors.
Professional burnout and mental health comorbidities are on a steep rise, further fueled by the recent Covid-19 pandemic.9 While job burnout among physical therapists (PTs) is associated with emotional exhaustion and a decreased sense of personal achievement,10 no study has examined the prevalence of IP in licensed PTs in the United States and explored whether it is linked to burnout and job satisfaction. The objectives of the present study were to (1) examine the prevalence of IP among licensed PTs in the United States, (2) determine demographic and professional factors associated with IP, and (3) examine its relationship with burnout and job satisfaction.
2 METHODS
2.1 Study design and setting
This is a cross-sectional observational survey study. The survey was delivered in English and hosted on Google Forms, a web-based survey tool. Data collection took place from June 10 to July 10, 2022. The study was approved by West Coast University's Institutional Review Board and followed the STROBE guidelines.
2.2 Role of funding source
No funding from agencies in the public, commercial, or not-for-profit sectors played a role in the design, conduct, or reporting of this research.
2.3 Participants, recruitment, and consent
Eligible participants were licensed PTs in the United States. A recruitment flyer was shared with peers/colleagues, posted on social media, and distributed through professional organizations, such as the Academies of the American Physical Therapy Association (APTA) that allow electronic survey distribution to their members, including orthopedics, neurological, geriatrics, home health, and aquatics. Members of the American Academy of Orthopaedic Manual Physical Therapists and both the Illinois Physical Therapy Association as well as the California Physical Therapy Association were also invited to engage in the survey. Each participant provided informed consent before taking the survey and was instructed to only complete the survey once.
2.4 Online survey
The survey was created by the study team of four PTs, each with greater than 5 years of experience in clinical practice. The authors recruited five practicing PTs from various practice settings to pilot-test the survey draft. Their feedback was used to refine the survey before its distribution. The final survey consisted of 18 demographic and professional questions and three subsurveys to measure the degree of IP, emotional exhaustion/burnout, and job satisfaction.
Demographic questions included age, race, gender, sexuality, years of experience, length at current position, practice setting, practice specialty, terminal degree, credentials (e.g., Orthopedic Certified Specialist, Fellow of the American Academy of Orthopaedic Manual Physical Therapists, etc.), APTA membership, geographical location of practice, manager/supervisor experience, time per week spent on direct patient care, duration of initial evaluations, duration of return visits, and mental health diagnosis. In questions where respondents selected “other” in place of the listed options, a free-text box was provided for more detailed responses.
The 20-item Clance Imposter Phenomenon Scale was used to assess the degree of IP.1 It is the most widely used instrument known for its good reliability and validity, and ability to distinguish from self-esteem, social anxiety, and self-monitoring.11-13 The scale uses a 5-point Likert scale for each question with a total score ranging from 20 to 100. A score below or equal to 40 is considered low IP, 41–60 is moderate, 61–80 is frequent, and greater than 80 is intense IP.1
Emotional exhaustion is the greatest predictor of burnout.14 To assess this key attribute, the survey utilized a 9-item emotional exhaustion scale, a subscale within the Maslach Burnout Inventory.15 The items were answered on a 5-point frequency scale ranging from 1 (never) to 5 (always) with a total score ranging from 9 to 45.16, 17 A score of 27 or higher indicates extreme emotional exhaustion level, 19–26 moderate level, and 18 or under low level.16
The Job Satisfaction Subscale of the Michigan Organizational Assessment Questionnaire was used to measure job satisfaction, which includes three questions on a 6-point Likert scale.18 The first question was negatively worded, therefore was scored in reverse to align with the remaining two positively worded questions. The final scores range from 3 to 18. Scores were dichotomized into yes (score ≥12) versus no (score <12) job satisfaction. It took approximately 5–10 min to complete the survey and there was no financial compensation awarded to participants.
2.5 Data cleaning
Respondents who were not licensed PTs, such as physical therapy assistants and students, were excluded. One participant did not answer the demographic questions, therefore was also excluded.
2.6 Data synthesis and analysis
Following recommended guidelines,1, 15, 18 Clance IP raw scores were categorized into four distinct IP levels of low (≤40), moderate (41–60), frequent (61–80), and intense (>80); emotional exhaustion scores to low (≤18), moderate (19–26), and high (≥27); job satisfaction scores to yes (≥12) and no (<12). Descriptive statistics summarized the characteristics for the overall sample and by IP levels. All predictors in the analysis were categorical variables and reported as counts with percentage. Missing data (i.e., the response was “blank”) were not imputed.
To assess univariate associations between each factor and IP levels, Chi-squared tests were conducted. Factors with a p ≤ 0.20 in the univariate comparisons were considered for inclusion in the final multivariable logistic regression model. For ease of interpretation, IP levels were condensed to a binary outcome of no (combining low and moderate IP) versus yes (combining frequent and intense IP). Multicollinearity check was performed.
Purposeful model selection19 was used to produce the final regression model. Briefly, the iterative process proposed in the purposeful model selection recommends (1) removing predictors with a p ≤ 0.1; (2) adding back a predictor if removing it resulting in ≥20% change in any of the remaining predictor's beta coefficients, because the deleted predictor has provided important adjustment of the effect of the remaining predictors; (3) selecting the model with the highest R2; and (4) including predictors that are clinically meaningful/important based on content expertise and prior literature. The Hosmer–Lemeshow goodness-of-fit test checked the fit of the final model. Results were reported as odds ratios (ORs) and 95% confidence intervals (CIs). ORs >1.0 indicated increased odds and <1.0 indicated decreased odds. All analyses were performed using SPSS 28.0.1.1.
3 RESULTS/FINDINGS
A total of 520 survey responses were recorded. After excluding responses from physical therapy students and/or physical therapy assistants (n = 5) and the response without any demographic data (n = 1), our final analysis sample consisted of 514 records.
Table 1 summarizes the demographic and professional characteristics of the study respondents. The majority of respondents were women (66.1%), at or under 40 years of age (73.2%), and White race (77.0%). The mean IP score was 60.3 (SD: 15.1, range: 19–95). As shown in Figure 1, 55 (10.7%) had low IP, 196 (38.1%) had moderate IP, 215 (41.8%) had frequent IP, and 48 (9.3%) had intense IP. When dichotomized, IP was absent in 251 (48.8%) and present in 263 (51.2%) survey respondents. A sensitivity analysis to compare 4-level versus 2-level IP categories showed immaterial differences in factors with a p ≤ 0.20 (see Supporting Information S1: Table 1).
| Factor | Total N (N = 514) | Low IP (N = 55) | Moderate IP (N = 196) | Frequent IP (N = 215) | Intense IP (N = 48) | p Value* |
|---|---|---|---|---|---|---|
| Age groups (years) | <0.001 | |||||
| 20–30 | 172 | 9 (5.2%) | 60 (34.9%) | 83 (48.3%) | 20 (11.6%) | |
| 31-40 | 204 | 19 (9.3%) | 79 (38.7%) | 85 (41.7%) | 21 (10.3%) | |
| 41–50 | 67 | 10 (14.9%) | 28 (41.8%) | 26 (38.8%) | 3 (4.5%) | |
| 51–60 | 41 | 5 (12.2%) | 18 (43.9%) | 14 (34.1%) | 4 (9.8%) | |
| >60 | 30 | 12 (40.0%) | 11 (36.7%) | 7 (23.3%) | 0 (0.0%) | |
| Race | 0.523 | |||||
| White alone, non-Hispanic | 396 | 43 (10.9%) | 154 (38.9%) | 166 (41.9%) | 33 (8.3%) | |
| Asian alone, non-Hispanic | 36 | 5 (13.9%) | 9 (25.0%) | 18 (50.0%) | 4 (11.1%) | |
| Hispanic | 25 | 1 (4.0%) | 10 (40.0%) | 12 (48.0%) | 2 (8.0%) | |
| Other | 57 | 6 (10.5%) | 23 (40.4%) | 19 (33.3%) | 9 (15.8%) | |
| Gender | 0.002 | |||||
| Cisgender woman | 340 | 27 (7.9%) | 117 (34.4%) | 161 (47.4%) | 35 (10.3%) | |
| Cisgender man | 128 | 22 (17.2%) | 55 (43.0%) | 40 (31.3%) | 11 (8.6%) | |
| Other/prefer not to answer | 46 | 6 (13.0%) | 24 (52.2%) | 14 (30.4%) | 2 (4.3%) | |
| Sexuality | 0.670 | |||||
| Heterosexual | 446 | 45 (10.1%) | 169 (37.9%) | 189 (42.4%) | 43 (9.6%) | |
| LGBTQ plus | 38 | 4 (10.5%) | 16 (42.1%) | 16 (42.1%) | 2 (5.3%) | |
| Prefer not to answer | 30 | 6 (20.0%) | 11 (36.7%) | 10 (33.3%) | 3 (10.0%) | |
| Geographic locationa | 0.035 | |||||
| Midwest | 172 | 20 (11.6%) | 69 (40.1%) | 70 (40.7%) | 13 (7.6%) | |
| Northeast | 86 | 15 (17.4%) | 28 (32.6%) | 35 (40.7%) | 8 (9.3%) | |
| Other (e.g., abroad) | 11 | 0 (0.0%) | 1 (9.1%) | 6 (54.5%) | 4 (36.4%) | |
| Southeast | 57 | 8 (14.0%) | 22 (38.6%) | 24 (42.1%) | 3 (5.3%) | |
| Southwest | 34 | 4 (11.8%) | 15 (44.1%) | 10 (29.4%) | 5 (14.7%) | |
| West | 135 | 8 (5.9%) | 50 (37.0%) | 65 (48.1%) | 12 (8.9%) | |
| Time as a licensed PT (years) | <0.001 | |||||
| ≤5 | 198 | 11 (5.6%) | 66 (33.3%) | 95 (48.0%) | 26 (13.1%) | |
| 6–10 | 128 | 8 (6.3%) | 48 (37.5%) | 65 (50.8%) | 7 (5.5%) | |
| 11–20 | 95 | 13 (13.7%) | 43 (45.3%) | 29 (30.5%) | 10 (10.5%) | |
| >20 | 93 | 23 (24.7%) | 39 (41.9%) | 26 (28.0%) | 5 (5.4%) | |
| Time in current position (years)b | <0.001 | |||||
| <1 | 152 | 5 (3.3%) | 51 (33.6%) | 76 (50.0%) | 20 (13.2%) | |
| 1–3 | 169 | 19 (11.2%) | 65 (38.5%) | 71 (42.0%) | 14 (8.3%) | |
| 4–6 | 86 | 9 (10.5%) | 29 (33.7%) | 38 (44.2%) | 10 (11.6%) | |
| >6 | 106 | 22 (20.8%) | 50 (47.2%) | 30 (28.3%) | 4 (3.8%) | |
| Practice settingc | 0.895 | |||||
| Private practice | 229 | 27 (11.8%) | 78 (34.1%) | 101 (44.1%) | 23 (10.0%) | |
| Hospital | 190 | 16 (8.4%) | 81 (42.6%) | 77 (40.5%) | 16 (8.4%) | |
| Academic | 32 | 4 (12.5%) | 13 (40.6%) | 12 (37.5%) | 3 (9.4%) | |
| Military | 12 | 2 (16.7%) | 5 (41.7%) | 3 (25.0%) | 2 (16.7%) | |
| Other non-for-profit | 12 | 1 (8.3%) | 5 (41.5%) | 6 (50.0%) | 0 (0.0%) | |
| Other | 31 | 5 (16.1%) | 11 (35.5%) | 13 (41.9%) | 2 (6.5%) | |
| Practice specialtyd | 0.861 | |||||
| Orthopedics | 374 | 42 (11.2%) | 138 (36.9%) | 157 (42.0%) | 37 (9.9%) | |
| Geriatrics | 31 | 2 (6.5%) | 17 (54.8%) | 12 (38.7%) | 0 (0.0%) | |
| Neurology | 28 | 5 (17.9%) | 8 (28.6%) | 13 (46.4%) | 2 (7.1%) | |
| Pelvic Health | 25 | 2 (8.0%) | 9 (36.0%) | 10 (40.0%) | 4 (16.0%) | |
| Pediatrics | 17 | 0 (0.0%) | 6 (35.3%) | 9 (52.9%) | 2 (11.8%) | |
| Sports | 4 | 0 (0.0%) | 1 (25.0%) | 2 (50.0%) | 1 (25.0%) | |
| Cardiopulmonary | 2 | 0 (0.0%) | 1 (50.0%) | 1 (50.0%) | 0 (0.0%) | |
| Oncology | 1 | 0 (0.0%) | 0 (0.0%) | 1 (100.0%) | 0 (0.0%) | |
| Other | 8 | 1 (12.5%) | 4 (50.0%) | 2 (25.0%) | 1 (12.5%) | |
| Terminal degreeb | 0.015 | |||||
| DPT | 425 | 40 (9.4%) | 158 (37.2%) | 190 (44.7%) | 37 (8.7%) | |
| Bachelor's degrees | 16 | 5 (31.3%) | 4 (25.0%) | 4 (25.0%) | 3 (18.8%) | |
| Master's degrees | 38 | 3 (7.9%) | 16 (41.2%) | 15 (39.5%) | 4 (10.5%) | |
| EdD, DSc, DHS, or PhD | 34 | 6 (17.6%) | 18 (52.9%) | 6 (17.6%) | 4 (11.8%) | |
| APTA membershipe | 0.546 | |||||
| Yes | 312 | 37 (11.9%) | 114 (36.5%) | 129 (41.3%) | 32 (10.3%) | |
| No | 200 | 18 (9.0%) | 81 (40.5%) | 85 (42.5%) | 16 (8.0%) | |
| Credentials | 0.295 | |||||
| Board certified specialties | 103 | 11 (10.7%) | 40 (38.8%) | 43 (41.7%) | 9 (8.7%) | |
| Fellow (FAAOMPT) | 88 | 16 (18.2%) | 37 (42.0%) | 29 (33.0%) | 6 (6.8%) | |
| Other | 61 | 3 (4.9%) | 25 (41.0%) | 27 (44.3%) | 6 (9.8%) | |
| None | 262 | 25 (9.5%) | 94 (35.9%) | 116 (44.3%) | 27 (10.3%) | |
| Manager/supervisor experiencef | <0.001 | |||||
| Yes | 204 | 35 (17.2%) | 90 (44.1%) | 66 (32.4%) | 13 (6.4%) | |
| No | 305 | 20 (6.6%) | 104 (34.1%) | 147 (48.2%) | 34 (11.1%) | |
| Time per week spent on direct patient care (hours/week)e | 0.101 | |||||
| <10 | 66 | 14 (21.2%) | 26 (39.4%) | 23 (34.8%) | 3 (4.5%) | |
| 11–20 | 61 | 6 (9.8%) | 24 (39.3%) | 24 (39.3%) | 7 (11.5%) | |
| 21–30 | 103 | 11 (10.7%) | 42 (40.8%) | 37 (35.9%) | 13 (12.6%) | |
| >30 | 282 | 24 (8.5%) | 103 (36.5%) | 130 (46.1%) | 25 (8.9%) | |
| Time spent with patients during initial evaluations (minutes)g | 0.094 | |||||
| <44 | 147 | 15 (10.2%) | 64 (43.5%) | 58 (39.5%) | 10 (6.8%) | |
| 45–59 | 234 | 24 (10.3%) | 75 (32.1%) | 106 (45.3%) | 29 (12.4%) | |
| ≥60 | 118 | 14 (11.9%) | 53 (44.9%) | 43 (36.4%) | 8 (6.8%) | |
| Time spent with patients during return visits (minutes)h | 0.504 | |||||
| <30 | 95 | 8 (8.4%) | 34 (35.8%) | 43 (45.3%) | 10 (10.5%) | |
| 30–44 | 192 | 22 (11.5%) | 71 (37.0%) | 87 (45.3%) | 12 (6.3%) | |
| 45–59 | 154 | 17 (11.0%) | 62 (40.3%) | 55 (35.7%) | 20 (13.0%) | |
| ≥60 | 59 | 6 (10.2%) | 26 (44.1%) | 22 (37.3%) | 5 (8.5%) | |
| History of or current mental health diagnosis | <0.001 | |||||
| Yes | 134 | 7 (5.2%) | 33 (24.6%) | 73 (54.5%) | 21 (15.7%) | |
| Unsure/not diagnosed by a professional | 76 | 5 (6.6%) | 17 (22.4%) | 40 (52.6%) | 14 (18.4%) | |
| No | 304 | 43 (14.1%) | 146 (48.0%) | 102 (33.6%) | 13 (4.3%) | |
| Emotional exhaustion | <0.001 | |||||
| Low | 63 | 23 (36.5%) | 34 (54.0%) | 5 (7.9%) | 1 (1.6%) | |
| Moderate | 192 | 21 (10.9%) | 91 (47.4%) | 70 (36.5%) | 10 (5.2%) | |
| High | 259 | 11 (4.2%) | 71 (27.4%) | 140 (54.1%) | 37 (14.3%) | |
| Job satisfactioni | 0.023 | |||||
| Low | 89 | 6 (6.7%) | 25 (28.1%) | 50 (56.2%) | 8 (9.0%) | |
| High | 423 | 49 (11.6%) | 169 (40.0%) | 165 (39.0%) | 40 (9.5%) |
- a did not answer (n = 19).
- b did not answer (n = 1).
- c did not answer (n = 8).
- d did not answer (n = 24).
- e did not answer (n = 2).
- f did not answer (n = 5).
- g did not answer (n = 15).
- h did not answer (n = 14).
- i did not answer (n = 2).
- * p Values comparing across four IP categories ≤0.20 are marked in bold.
Age was strongly correlated with years of experience as a PT (R = 0.85), therefore was excluded from the model to avoid multicollinearity. The initial logistic regression model included the following 11 predictors: gender, geographic location, time as a licensed PT, time in current position, terminal degree, manager/supervisor experience, time spent on direct patient care, time spent with patients during initial evaluations, history of or current mental health diagnosis, emotional exhaustion, and job satisfaction.
Following the principles for purposeful model selection (outlined in the Methods section), we identified the final most parsimonious logistic regression model, shown in Table 2. The Hosmer–Lemeshow goodness-of-fit test had a p = 0.897, suggesting that there was no significant difference between observed and predicted values.
| Factor | Odds ratio | 95% CI (Upper bound) | 95% CI (Lower bound) | p Value* |
|---|---|---|---|---|
| Gender | ||||
| Cisgender man (Reference group) | ||||
| Cisgender woman | 1.30 | 0.79 | 2.15 | 0.308 |
| Other/prefer not to answer | 0.58 | 0.25 | 1.33 | 0.197 |
| Time as a licensed PT (years) | ||||
| ≤5 (Reference group) | ||||
| 6–10 | 1.25 | 0.70 | 2.23 | 0.451 |
| 11–20 | 0.55 | 0.28 | 1.08 | 0.081** |
| >20 | 0.98 | 0.43 | 2.26 | 0.962 |
| Time in current position (years) | ||||
| <1 (Reference group) | ||||
| 1–3 | 0.94 | 0.56 | 1.60 | 0.821 |
| 4–6 | 1.03 | 0.53 | 2.03 | 0.925 |
| >6 | 0.50 | 0.24 | 1.04 | 0.064** |
| Manager/supervisor experience | ||||
| No (Reference group) | ||||
| Yes | 0.55 | 0.34 | 0.90 | 0.017 |
| Terminal degree | ||||
| DPT (Reference group) | ||||
| Bachelor's or Master's degrees | 2.31 | 1.07 | 5.00 | 0.034 |
| EdD, DSc, DHS, or PhD | 0.71 | 0.28 | 1.81 | 0.469 |
| History of or current mental health diagnosis | ||||
| No (Reference group) | ||||
| Yes | 2.77 | 1.69 | 4.54 | <0.001 |
| Unsure/not diagnosed by a professional | 3.21 | 1.74 | 5.94 | <0.001 |
| Emotional exhaustion | ||||
| Low (Reference group) | ||||
| Moderate | 5.37 | 2.11 | 13.69 | <0.001 |
| High | 14.13 | 5.56 | 35.89 | <0.001 |
- * p ≤ 0.05 are marked in bold
- ** p < 0.10.
Having managerial or supervisory experience reduced the likelihood of IP by 45% (OR = 0.55, [95% CI = 0.34–0.90]). Having a terminal bachelor's or master's degree (vs. a terminal DPT degree) (OR = 2.31, [95% CI = 1.07–5.00]); history of or current mental health diagnosis (OR = 2.77 [95% CI: 1.69–4.54]), unsure/undiagnosed mental health diagnosis (OR = 3.21 [95% CI: 1.74–5.94]), and moderate or high level of emotional exhaustion (OR = 5.37 [95% CI: 2.11–13.69]; OR = 14.13 [95% CI: 5.56–35.89], respectively] each increased the odds of IP. Having 11–20 years of clinical experience (vs. ≤5 years) and holding their current position >6 years (vs. <1 year) may reduce the odds of IP (OR = 0.55 [95% CI: 0.28–1.08, p = 0.08]; OR = 0.50 [95% CI: 0.24–1.04, p = 0.06], respectively). It is important to point out that these associations were cross-sectional; no causal inference could be made. For example, the negative association of having managerial or supervisory experience and the presence of IP could be bidirectional. Those with IP might not believe that they could be in a leadership role, therefore may not seek a managerial/supervisory position; or managers/supervisors were less likely to experience IP.
4 DISCUSSION
IP is highly prevalent among PTs in the United States. Over half of the survey respondents reported frequent or intense IP. Seasoned clinicians holding managerial positions exhibited a lower susceptibility to IP, whereas individuals with a mental health diagnosis, emotional exhaustion, and lacking a DPT degree were more prone to this phenomenon. Other factors, such as gender, race, sexuality, geographic location, practice specialty/setting, APTA membership, and job satisfaction did not significantly influence IP. A reduced likelihood of experiencing IP appeared to be associated with a greater length of time held in a professional position. Interestingly, there appeared to be a sweet spot in terms of years as a licensed PT. Specifically, having 11–20 years of clinical practice experience may be linked to reduced IP. To the best of our knowledge, this is the first report investigating the prevalence, predictors, and impact of IP among licensed PTs in the United States. Given the high prevalence of IP and its potential negative impacts on mental well-being, it is important to provide education and resources to effectively manage and overcome this phenomenon in the physical therapy community.
The current study findings are in general agreement with previous research conducted in other licensed healthcare professions. In a literature review of studies involving medical students, residents, and physicians,4 the prevalence of IP ranged from 22.5% to 46.6%. The mean imposter scores within these studies ranged from 47.0 to 61.2. Frequent-to-intense IP was observed in 38.9% of neurosurgeons and neurosurgery residents, with the majority of individuals reporting moderate levels of IP (42.7%).20 A significant proportion of radiologists (71%) experienced frequent-to-intense IP.21 This finding should be interpreted with caution. The limited number of participants (n = 21) may introduce the possibility of participation bias, which could potentially overestimate the rate of IP. It is unknown whether the extent of IP differs in various healthcare providers. To our knowledge, no study has directly compared IP prevalence across different healthcare professionals.
A noteworthy result emerged from the current study, revealing that over 40% of respondents reported a diagnosed or suspected mental health condition. This finding underscores the significance of pre-existing mental health comorbidities in PTs. These conditions can be further exacerbated by elevated levels of occupational stress resulting from a number of factors, including demanding physical and mental workloads, significant administrative work (e.g., documentation and billing), high patient expectation and demands, the constant pressure to stay updated in the field and continually learn, and productivity benchmarks within healthcare settings.10, 22, 23 Our data showed that respondents with diagnosed or suspected mental health conditions were approximately three times more likely to experience IP. Poor mental health can significantly hinder professional performance, elevate the risk of medical errors, contribute to burnout, and amplify the experience of IP.3, 4, 24 Further, individuals with perfectionist tendencies and difficulty internalizing their successes are more susceptible to experiencing IP. These tendencies not only contribute to the development of IP but can also function as precursors to mental health conditions, such as anxiety and depression. This interplay between perfectionism, inadequate self-assessment of achievements, IP, and mental health challenges could have detrimental effects on professional and personal outcomes.3, 4, 22, 24
The majority of PTs (87.7%) in this survey experienced at least moderate levels of emotional exhaustion and approximately half experienced high levels. Emotional exhaustion has been identified as a central measure of burnout,25, 26 which could lead to medical errors, reduced productivity, and turnover.10, 23 Contrary to a previous study that reported no clear relationship between burnout and IP in 48 internal medicine residents,27 we found a dose–response relationship between emotional exhaustion. A higher level of emotional exhaustion was associated with a greater likelihood of IP. PTs may be more susceptible to burnout, given the prolonged and frequent patient encounters within a typical work week.10 However, in our study sample, reported job satisfaction was high among PTs (82%). Time spent on direct patient care or time spent with patients during initial evaluation and return visits did not appear to heavily impact IP. Thus, factors beyond workload and time spent with patients must be further explored to better understand the underlying causes for emotional exhaustion in PTs.
Respondents with managerial/supervisory roles or longer time in the current position were less likely to experience IP. Prior research has not consistently demonstrated a clear relationship between job ranks or professional longevity with IP. Among surgeons, IP was more prevalent and worse in trainees and residents than faculty mentors.20, 28 On the contrary, nontenured faculty had lower IP scores than their tenure-track counterparts29 and IP was common in those working in top research institutions.30 This is potentially due to the high-pressure research environments and intense competition for funding and recognition. The conflicting observations could be related to differences in job security, workload, and expectations between clinical and academic settings.
Gender was not linked to IP when accounting for other demographic, professional, and mental health factors. While early studies primarily focused on the prevalence of IP in females in various occupational settings, updated research revealed that IP is common in both men and women.2 Notably, the univariable association between gender and IP attenuated to non-significance after adjusting for other variables. This finding highlights that gender alone may not be a significant predictor of IP and caution against drawing conclusions solely on gender when seeking to understand the risk profile of IP.
The present study has significant strengths. This is the first study that comprehensively examined IP and its predictors among licensed PTs, using a widely accepted, validated outcome measure to categorize IP. Compared to previous research of IP in healthcare professionals, the present study included the largest sample to date and employed a more rigorous analytic approach of multivariable regression modeling that encompasses a broad spectrum of demographic and professional factors. Our study sample was representative of the demographics of licensed PTs in the United States, as reported by the US Bureau of Labor Statistics, 2022.31 This alignment with the broader PT community enhances the generalizability of our findings and allows for meaningful comparisons and inferences regarding IP in PTs. Additionally, a focus group was utilized before survey distribution to ensure inclusivity and ease with the survey experience.
Our study also has limitations. The cross-sectional study design precludes us from establishing causal relationships. We cannot definitively determine whether the identified demographic and professional factors were predictors for or consequences of IP. Nonetheless, this study provides a valuable framework for future investigations aimed at mitigating potential risk factors associated with IP. Future longitudinal studies could provide a more in-depth understanding of the dynamics over time and allow for the examination of causal relations. An online survey study design has some inherent limitations. The decision of invited survey participants to respond or not could be influenced by their level of interest in the topic or their availability at the time of the survey invitation, potentially introducing bias to the sample. Additionally, self-reported data may be influenced by factors like social desirability and recall bias. Although this survey was peer reviewed by a focus group of PTs from diverse clinical settings to ensure clarity and comprehensibility before its dissemination, some variability in the interpretation of the survey questions may have occurred. Due to the multiple channels of survey distribution and deidentified collection of information, individuals may have accessed and responded to the survey more than once, despite being informed to avoid repeated attempts.
IP is highly prevalent among licensed PTs, with more than half reporting frequent or intense IP. Seasoned clinicians with managerial roles seemed to be less susceptible to IP, whereas those with mental health diagnoses, emotional exhaustion, and those without a DPT degree may be more likely to experience IP. Given the high prevalence of IP and its negative impacts, it is important to prioritize education and awareness about this phenomenon. PT clinicians and students need to be equipped with information, strategies, and resources to effectively manage and mitigate IP, ensuring their long-term professional success and personal well-being.
AUTHOR CONTRIBUTIONS
Alexandra R. Anderson: Conceptualization; data curation; investigation; methodology; project administration; writing—original draft; writing—review and editing. Jamie LaPenna: Conceptualization; investigation; methodology; project administration; writing—original draft; writing—review and editing. Dustin Willis: Data curation; investigation; methodology; project administration; writing—original draft; writing—review and editing. Khyrah Simpson: Data curation; formal analysis. Alison H. Chang: Data curation; formal analysis; methodology; writing—original draft; writing—review and editing.
ACKNOWLEDGMENTS
The authors would like to thank survey participants for their contribution to the study.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Study approved by West Coast University's Institutional Research Board. Each participant provided informed consent before taking the survey.
TRANSPARENCY STATEMENT
The lead author Alexandra R. Anderson affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
Data are available from the corresponding author upon reasonable request.