Association of BMI and incidence of type 2 diabetes in Saudi population
Abstract
Objective
The study aims to identify the optimal body mass index (BMI) cut-off for obesity based on the risk of developing type 2 diabetes among the general population visiting primary health care in Saudi Arabia.
Methods
A cross-sectional study was conducted in Al-Ahsa City, Saudi Arabia, from January to June 2022. The study included Saudi citizens aged 35 and older who had not previously or currently been diagnosed with type 2 diabetes. Data were collected through electronic health records from 48 primary healthcare centers. The variables derived from medical records were age, gender, HbA1c, weight, and height.
Results
The BMI mean among nondiabetic, prediabetic, and diabetic groups were 29.6 ± 6.2, 31.2 ± 6.6, and 31.7 ± 6.9 kg/m2, respectively. The BMI of the prediabetic and diabetic males were 30.1 ± 6.3 and 30.5 ± 6.5 kg/m2, respectively, and the BMI of the pre-diabetic and diabetic females were 31.9 ± 6.6 and 32.8 ± 7 kg/m2, respectively.
Conclusion
The current study correlated the result of HbA1c levels with BMI cut-off values as a modifiable risk factor for developing type 2 diabetes among the Al-Ahsa population in Saudi Arabia. The BMI mean among nondiabetic, prediabetic, and diabetic groups were 29.6 ± 6.2, 31.2 ± 6.6, and 31.7 ± 6.9 kg/m2, respectively. This study provided a list of BMI values as cut-off points with their sensitivity and specificity measures so the policymaker could utilize them. The best cut-off point could be decided based on cost-effective analysis. Further studies in the future might help evaluate the efficacy of screening programs and the association between BMI and other types of diabetes.
1 INTRODUCTION
Body mass index (BMI), also known as the Quetelet's index, is used to measure nutritional status in the adult population. It can be calculated by dividing a person's weight in kilograms by the square of the person's height in meters (kg/m2).1 It is a valuable screening method for weight, which is categorized into underweight (if BMI < 18.5 kg/m2), healthy weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obesity (BMI 30 kg/m2 and above).2
The prevalence and incidence of being overweight and obese have increased recently.3 Moreover, obesity is estimated to be the sixth most contributing risk factor to the overall burden of disease worldwide. High BMI contributed to an estimated 4 million deaths globally in 2015.4
A previous study showed variation among different ethnicities regarding BMI-related complications. For instance, type 2 diabetes was highly prevalent among Asian populations at a lower BMI than in white people. So, it is wise to determine BMI cut-offs for obesity in which complications, such as type 2 diabetes, are likely to develop and subsequently come up with clinical guidelines for better care.5
Diabetes mellitus (DM) is a significant global disease. According to the International Diabetes Federation (IDF), at least 463 million adults were globally diagnosed with DM in 2019. The prevalence of DM in Saudi Arabia (SA) is growing very fast. Among the Middle East, Saudi Arabia is the second most prevalent in DM and seventh worldwide.6 The main form of diabetes mellitus is type 2 (T2DM), which can be prevented by enhancing the lifestyle of the individual (e.g., losing weight).7 One of the critical risk factors for developing T2DM is excess body fat.
A standard method to estimate excess body fat is BMI, predicting the risk of developing T2DM. A BMI of ≥30 kg/m2 is a crucial risk factor for T2DM, particularly among white populations, even though ethnicity-appropriate obesity cut-offs are much debated.8 For example, there was a high prevalence of T2DM at lower BMI among Asian populations. Thus, the World Health Organization (WHO) recommended that the BMI cut-off for obesity detection in Asian populations is ≥27.5 kg/m2.9 A recent study in England showed the incidence of type 2 diabetes among Arabs at a BMI cut-off of 26.6 kg/m².10 Furthermore, a study done in Kenya in 2021 demonstrated that the optimal cut-off of BMI to predict T2DM was 24.8 kg/m².11
The significance of conducting studies on the relationship between BMI cut-offs and the incidence of diabetes in Saudi Arabia cannot be overstated. Currently, there is a conspicuous absence of research in this specific context, which is quite concerning given the rising prevalence of diabetes in the country. By exploring this crucial link, researchers can establish valuable guidelines for healthcare practitioners and policymakers, leading to improved preventive strategies and more effective interventions.
First, it is important to emphasize that the lack of studies in Saudi Arabia addressing the BMI cut-off and diabetes incidence is a noteworthy research gap. Given the population's unique genetic composition, lifestyle patterns, and cultural practices, generalizing findings from studies conducted in different populations and ethnicities becomes questionable. Therefore, it is crucial to gather data within the Saudi context to ensure the accuracy and applicability of findings, guiding healthcare professionals in their decision-making processes.
Moreover, addressing the absence of studies on this subject in Saudi Arabia is essential due to the rapidly increasing prevalence of diabetes in the country. According to recent reports, Saudi Arabia has one of the highest rates of diabetes worldwide (IDF, 2019). This alarming trend calls for an urgent investigation into the factors contributing to this epidemic, including the role of BMI cut-offs. By identifying the specific thresholds at which the risk of developing diabetes significantly increases within this population, healthcare providers can accurately screen individuals at risk and implement appropriate interventions.
Another significant point to consider is that the scarcity of studies specifically conducted in Saudi Arabia undermines the efficacy of DM risk assessment tools currently in use. Most of these instruments were developed based on data gathered from different populations and ethnicities, potentially compromising their applicability to individuals in Saudi Arabia. Consequently, relying on such tools might lead to inaccurate risk predictions and inadequate preventive measures, further exacerbating the diabetes epidemic in the country. By conducting local studies, researchers can develop tailored risk assessment tools that accurately reflect the Saudi population's unique characteristics.
1.1 Obesity and diabetes: A postpandemic continuum
It has long been known that obesity and type 2 diabetes are linked, and it is believed that between 60 percent and 90% of persons who have type 2 diabetes are now or have previously been overweight.12 According to the researchers, more than half of COVID-19 patients had comorbidities, with hypertension being the most common, followed by diabetes and coronary heart disease, among other conditions (CVDs).
However, despite substantial reporting on the clinical features of COVID-19, no research has yet addressed in detail the involvement of obesity and diabetes in COVID-19, how COVID-19 impacts obesity and diabetes, or specialized therapy for these at-risk groups.13-15 A higher risk of acute and chronic infections has been shown to be connected with diabetes in both diabetics and nondiabetics. While suffering from the COVID-19 pandemic, diabetes patients died at a rate 3.1 times higher than nondiabetic patients, requiring the need of mechanical breathing and hospitalization in an intensive care unit (ICU).16
The COVID-19 outbreak has resulted in an ever-evolving global health hazard that is becoming more widespread. In part, as a result of their increasing incidence, obesity, and diabetes have been linked to a rise in public awareness of infectious diseases in general. For those with diabetes, a long-term, exceptionally high metabolic environment may permanently affect the immune system and worsen the inflammatory response, resulting in a bad prognosis for those who have COVID-19, according to the researchers. There is currently no indication that having diabetes increases the chance of contracting COVID-19 infection. At this time, there are just a few studies that have looked at the influence of COVID-19 on obesity and diabetes.
The importance of screening protocols in identifying high-risk patients cannot be overstated. Early detection through these protocols can significantly improve patient outcomes, reducing morbidity and mortality rates for various diseases. Furthermore, the development of structured screening programs tailored to specific diseases and risk factors allows healthcare providers to allocate resources efficiently and ensure appropriate interventions are initiated promptly. By empowering patients and facilitating informed decision-making, screening protocols also foster a collaborative approach to healthcare, promoting patient engagement and overall well-being. Therefore, healthcare systems should prioritize the development and implementation of comprehensive screening protocols as a vital healthcare tool. So, this study aims to identify the optimal BMI cut-off for obesity based on the risk of developing type 2 diabetes among the general population visiting primary healthcare centers (PHCs) in Al-Ahsa City, Saudi Arabia.
2 METHODS
2.1 Study design and study subjects
A cross-sectional study was conducted in Al-Ahsa City, Saudi Arabia, from January to June 2022. The study included Saudi citizens aged 35 and older who had not previously or currently been diagnosed with type 2 diabetes. Non-Saudis under the age of 35 who had been diagnosed with type 2 diabetes were barred from participating in the research. The study was approved by the IRB committee at King Fahad Hospital (IRB KFHH) in Hofuf (IRB approval number: 36-EP-2021). Permission to access the medical data of primary care providers in the Al-Ahsa cluster was gained with the knowledge and cooperation of the Al-Ahsa cluster's members.
2.2 Sample size and sampling technique
The sample size was calculated using Raosoft software, with a margin of error of 5%, a confidence level of 95%, a population size of approximately 1,000,000, and a response distribution of 50%, all with a margin of error of 5%, a confidence level of 95%, and a confidence level of 95%. It was predicted that 400 people would attend. We did, however, boost the total number of participants to 15858 people. We recruited participants using a convenience sample approach from the electronic health records of 48 PHCs in Saudi Arabia, utilizing information from their electronic health records.
2.3 Study procedure
To achieve the goals of the present study, we used the electronic health records from PHCs. The variables, including age, gender, HbA1c, height, and weight, were taken from medical records to calculate the BMI (kg/m2). Measuring height in cm and weight in kg are routinely measured in each visit to PHCs and are kept in the medical records. According to recent guidelines, the studied population has to be screened for type 2 diabetes for early recognition of the disease.
2.4 Data management and statistical analysis
The data were stored in a drive with high privacy and confidentiality. Data were analyzed using the SPSS version 26 program. A negative binomial model was used. It was age-adjusted and sex-adjusted and fitted with incident type 2 diabetes. The BMI value was calculated for the predicted incidence of type 2 diabetes among individuals.
Based on the outcomes of BMI estimates that were compared with the HbA1c%, the values of 100−specificity, specificity, sensitivity, Receiver Operating Characteristic (ROC) curve, and Area Under the Curve (AUC) were determined. These measures were used to evaluate the accuracy of BMI estimates in identifying people with T2DM and to evaluate the appropriateness of varied cut-off points.
3 RESULTS
There were 11,181 people from Saudi Arabia who had been analyzed regarding their hemoglobin A1c (HbA1c) level and its association with BMI. Those people were collected from 48 different PHCs located in five different zone areas of Al-Ahsa city (North, West, East, and Middle areas). Based on their HbA1c %, the included people were divided into three groups: nondiabetic with HbA1c < 5.7% (N = 4754), prediabetic with HbA1c 5.7–6.4% (N = 3936) and diabetic with HbA1c > 6.5% (N = 2491).
The results in (Table 1) showed that the BMI means among nondiabetic, prediabetic, and diabetic groups were 29.6 ± 6.2, 31.2 ± 6.6, and 31.7 ± 6.9 kg/m2, respectively. The mean BMI was statistically lower in the nondiabetic group compared to the pre-diabetic and diabetic groups (p < 0.01).
| Variable | HbA1c level | p Value | ||
|---|---|---|---|---|
| <5.7 | 5.7–6.5 | >6.5 | ||
| Mean BMI (SD) | 29.62 (6.2) | 31.2 (6.6) | 31.7 (6.9) | 0.001 |
| Mean age (SD) | 48.04 (9.4) | 51.36 (10.3) | 55.88 (10.8) | 0.001 |
| Male N (%) | 1761 (37.04) | 1538 (39.07) | 1183 (47.5) | 0.001 |
| N = 4754 | N = 3936 | N = 2491 | ||
The BMI of the prediabetic and diabetic males were 30.1 ± 6.3 and 30.5 ± 6.5 kg/m2, respectively, and the BMI of the prediabetic and diabetic females were 31.9 ± 6.6 and 32.8 ± 7 kg/m2, respectively (Table 2). The BMI of the prediabetic and diabetic groups showed a decline as participants' age increased (Table 3).
| Male patients with HbA1c 5.7–6.5 | Female patients with HbA1c 5.7–6.5 | Male patients with HbA1c >6.5 | Female patients with HbA1c >6.5 | |
|---|---|---|---|---|
| Mean BMI (SD) | 30.1 (6.3) | 31.9 (6.6) | 30.5 (6.5) | 32.8 (7) |
| Mean age (SD) | 51.7 (10.9) | 51.2 (9.9) | 55.7 (10.8) | 56 (10.8) |
| HbA1c 5.7-6.5 | HbA1c > 6.5 | |||||
|---|---|---|---|---|---|---|
| Age category | 35–44 y | 45–54 y | >55 y | 35–44 y | 45–54 y | >55 y |
| Mean BMI | 31.7 (7.4) | 31.4 (6.2) | 30.5 (6.1) | 33.2 (8.3) | 32.2 (6.9) | 30.9 (6.3) |
| N = 406 | N = 484 | N = 454 | N = 225 | N = 403 | N = 754 | |
Figure 1 shows the ROC curve and the AUC based on the BMI estimates. The sensitivity rate is plotted in function of 100-specificity at varied BMI estimates' cut-off points, with an AUC ≈ 0.5.
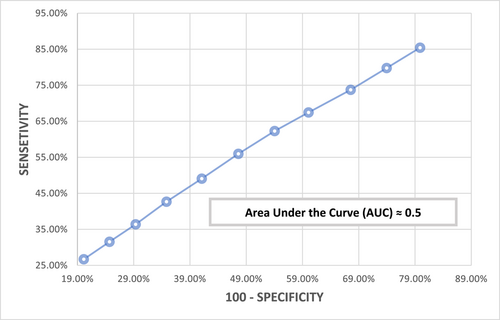
Table 4 revealed the false positive rate (100−specificity), sensitivity, and specificity at different cut-off points of the BMI estimates. Yet, the cut-off point at >31 m/k2 was 58.9% specific and 49.08% sensitive in identifying people with T2DM.
| BMI estimates cut-off point | Specificity | Sensitivity | 100-specificity | AUC |
|---|---|---|---|---|
| >35 | 79.87 | 26.7 | 20.13 | 0.0121752 |
| >34 | 75.31 | 31.55 | 24.69 | 0.01467075 |
| >33 | 70.66 | 36.39 | 29.34 | 0.01994172 |
| >32 | 65.18 | 42.67 | 34.82 | 0.02679676 |
| >31 | 58.9 | 49.08 | 41.1 | 0.031902 |
| >30 | 52.4 | 55.96 | 47.6 | 0.03603824 |
| >29 | 45.96 | 62.29 | 54.04 | 0.03756087 |
| >28 | 39.93 | 67.45 | 60.07 | 0.05052005 |
| >27 | 32.44 | 73.74 | 67.56 | 0.0471936 |
| >26 | 26.04 | 79.78 | 73.96 | 0.04730954 |
| >25 | 20.11 | 85.43 | 79.89 | 0.17179973 |
| – | – | – | – | 0.49590846 (≈0.5) |
4 DISCUSSION
The current study correlated the result of HbA1c levels with BMI values as a modifiable risk factor for developing type 2 diabetes compared with the nonmodifiable risk factors, including age and gender. The outcomes showed that the risk of transition from pre-diabetic (mean BMI = 31.2 kg/m2) to diabetic (mean BMI = 31.7 kg/m2) is sooner because there was no large gap between the mean BMI values.
Moreover, this study provided a list of BMI values as cut-off points with their sensitivity and specificity measures. In addition, the ROC curve has an AUC value ≈ 0.5, which indicates that we cannot notice a specific BMI cut-off point with an acceptable Youden's index. Despite thia, taking into consideration other risk factors for T2DM, the policy maker could utilize the list of BMI cut-off points in screening programs and determine a particular risk weightage per each cut-off point.
Compared to the outcomes of the current study, the incidence of type 2 diabetes among the White ethnic group in England was correlated with a BMI of 30.0 kg/m2.10 Among Asian Americans, more than 84% of them were recognized to have type 2 diabetes at a BMI value of ≥23 kg/m2.17 Black ethnic groups living in England were found to have type 2 diabetes onset at a BMI value of 28.1 kg/m2.10 South Asians, almost like Asian Americans, showed to have a BMI of 23.9 kg/m2 when during their diagnosis of type 2 diabetes.10
Based on the abovementioned results of different ethnic groups, the Al-Ahsa city population was quite similar to the English White ethnic group. Both populations showed that the risk of type 2 diabetes incidence was probably minimal when they were overweight. However, the risk weight of overweight among people with Asian and African origins is likely to be high. This highlights the importance of screening overweight people, especially those related to Asian and African ethnic groups, which can help in early detection, early intervention, preventing diabetic complications, and reducing the economic burden in the health care system.
4.1 Limitations
Due to the high prevalence of sickle cell trait and sickle cell disease in Al-Ahsa City, the accuracy of HbA1c outcomes might be affected.18, 19 Besides, the results revealed in the current study are limited to the Al-Ahsa city population and cannot be generalized to all Saudi citizens.
5 CONCLUSION
The current study correlated the result of HbA1c levels with BMI cut-off values as a modifiable risk factor for developing type 2 diabetes among the Al-Ahsa population in Saudi Arabia. The BMI mean among nondiabetic, prediabetic, and diabetic groups were 29.6 ± 6.2, 31.2 ± 6.6, and 31.7 ± 6.9 kg/m2, respectively. This study provided a list of BMI values as cut-off points with their sensitivity and specificity measures so the policymaker could utilize them. The best cut-off point could be decided based on cost-effective analysis. Further studies in the future might help evaluate the efficacy of screening programs and the association between BMI and other types of diabetes.
AUTHOR CONTRIBUTIONS
Qasem AlJabr: Conceptualization, data curation, funding acquisition, methodology, project administration, supervision, validation, visualization. Mohammed Alalawi: Methodology, writing—original draft. Baqer Aldehneen: Data curation, formal analysis, project administration, resources. Ali Al Gharash: Methodology, visualization, writing—original draft, writing—review and editing. Mohammed Aldabbab: Data curation, methodology, resources, software. Ali Bu-Khamseen: Data curation, validation, writing—original draft, writing—review and editing. Abdullah Alkattan: Formal analysis. Abdullah Al Sayafi: Data curation, formal analysis.
ETHICS STATEMENT
Ethical approval was granted from the Institutional Review Board committee of King Fahad Hospital in Al-Hofuf and approval number is (36-EP-2021).
TRANSPARENCY STATEMENT
The lead authors Ali Al Gharash, Abdullah Alkattan affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are included within the article.