Videographic analysis of blink dynamics in patients with chronic progressive external ophthalmoplegia, myogenic ptosis, and facial nerve palsy using smartphone camera: A comparative analysis
Abstract
Background and Aims
Congenital myogenic ptosis (CMP), chronic progressive external ophthalmoplegia (CPEO), and facial nerve palsy (FNP) are among the disorders which can seriously affect the blink dynamics of patients. Smartphone videography is a simple, convenient, and inexpensive way to capture eyelid movement. This study has measured and compared a variety of blink dynamics in these patients compared to healthy controls using 2-dimensional smartphone videography to enhance the utility of this method in both clinical and research settings.
Methods
A total of 30 adult participants with a complaint of impaired eyelid movements including 10 with CMP, 10 with CPEO, and 10 with unilateral FNP, as well as 10 healthy controls were recruited. Using a smartphone camera with a resolution of 240 frames per second in 720 p, various blink dynamics were measured.
Results
All case groups had significantly lower values of peak and average closing velocities, average opening velocity, and palpebral aperture and significantly higher values of eyelid closing duration, compared to controls. FNP participants also had significantly lower values in the full blink rate and peak opening velocity (POV) measures, and CPEO patients showed significantly lower values in the POV. Other measures were not statistically significantly different compared to healthy controls.
Conclusion
Our results indicated that all patients with CMP, FNP, and CPEO had different blinking dynamics compared to healthy controls, which is consistent with previous studies. Smartphone videography has achieved sufficient resolution and frame-rate to provide valuable information and anatomic details for clinical and research purposes. Further studies could utilize smartphone videography for further investigation and confirmation of the methodology in various conditions.
1 INTRODUCTION
Proper eyelid blinking provides the first line of protection, which is required for optimum performance of the eye. The eyelid blink spreads the antimicrobial tear film, removes debris, and stimulates Meibomian gland secretion, which maintains ocular surface physiology.1 There are typically three classes of blinks including voluntary, reflex, and spontaneous blinks which are associated with different dynamics, pathways, and temporal profiles.2
There are various variables to assess blink dynamics such as blink rate and blink duration, which are known to be associated with a wide range of conditions and disorders including state of attention, neurological diseases, ophthalmologic disorders, tiredness, contact lens, and ageing. Additionally, certain blinking patterns can be also used as a diagnostic measure in a variety of conditions and disorders.3 Notably, a previous study reported that the speed of the initial opening phase was reduced in congenital myogenic ptotic (CMP) patients, suggesting intrinsic muscle function change in the disorder's pathogenesis.4 Chronic progressive external ophthalmoplegia (CPEO) is a mitochondrial disorder characterized by slow progressive paralysis of the extraocular muscles, which have been previously linked with blink rate variability.5, 6 Facial nerve palsy (FNP) is a disorder that involves the paralysis of any structures innervated by the facial nerve, that could also lead to abnormalities in eye blinks as pretarsal orbicularis oculi muscles are innervated by the facial nerve.7
The gold standard for measuring the eyelid blink dynamics is still magnetic search coils, which may not be practical in the clinical setting and is mainly utilized for research purposes.8 However, in recent years, advances in high-speed imaging systems allowed us to evaluate these dynamics with a wide range of methodologies including magnetic-based devices, high-speed videography, infrared videography, pupillometry, and direct observation.3 Meanwhile, smartphone video camera has been recently improved and reached enough quality that enable them to produce video data which could be utilized to process and extract blinking metrics for ophthalmologist or research scientist. Previous studies have reported relatively similar results from of high-speed videography and magnetic search coils to produce blinking dynamics metrices.9 An analysis of spontaneous eyelid blink dynamics using smartphone camera concluded that videography by smartphone cameras captures anatomic detail and blink dynamics with sufficient resolution and clarity to provide clinical information about spontaneous eyelid blink rate, dynamics, and function.10
Despite improvements in quality of videos captured by smartphones and universal availability of smartphones, very few studies have investigated dynamics of eye blink among patients with eyelid movement disorder using videography native to smartphones. The objective of this study was to evaluate and compare blink dynamics among patients with CMP, CPEO, and FNP using 2-dimensional smartphone videography. The findings from this research aim to contribute to the existing knowledge base and enhance the utility of this method in both clinical and research settings.
2 METHODS
This case-control study was carried out at Farabi Eye Hospital, Tehran University of Medical Sciences, Iran, in 2021, following the guidelines of the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement. The research methods adhered to the principles outlined in the Declaration of Helsinki. The hospital ethics review board approved the protocol of the study and an informed consent was obtained from participants before entering the study.
2.1 Participants and design
In this study, a total of 30 adult participants with a complaint of impaired eyelid movements including 10 with CMP, 10 with CPEO, and 10 with unilateral FNP, as well as 10 healthy adult controls were recruited. Among the studied population, 35% of the participants (14/40) were male and the mean age of all participants was 36.25. Patients who had a history of previous eye surgery, corneal diseases, wearing contact lens, or used dopaminergic medications in the past year were excluded. All diagnoses were made by a group of attending eye surgeons.
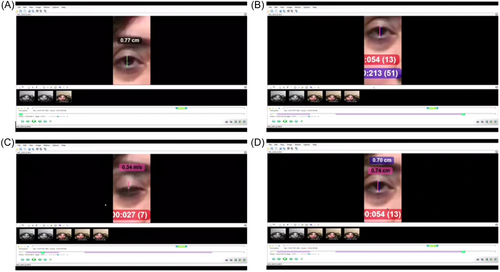
As a previous study revealed that a smartphone camera recording at 240 frames per second in 720p would be able to record spontaneous eyelid blink dynamics with sufficient clarity to provide robust objective information about spontaneous eyelid blink rate, dynamics, and function,10 we used a smartphone camera with similar specifications to record participants' eyelid blinkdynamics. The phone (iPhone 7; Apple Inc.) was placed on a tripod, 50 centimeters away from the subject. Participants were asked to relax and simply stare at the phone for 180 s, while their blinks were recorded. The chosen recording duration was intended to ensure a sufficient number of blinks for analysis and to replicate a logistically feasible recording timeframe during a clinical ophthalmology appointment. A ruler was placed beside the eyes of each participant to calibrate distance measurements. The first 10 s of each recorded video were discarded to eliminate the time it takes for a participant to adapt to the environment, minimize the influence of their initial awareness of being observed, and aim to capture authentic blink rates and dynamics. After the videos were recorded, video recordings were transferred to a computer and analyzed using a motion analysis software, a software designed for the tracking of markers used in human motion analysis.11 We used Kinovea software (version 0.9.5), a 2D motion analysis software that can be used to measure kinematic parameters, to analyze eyelid blink dynamics (Figure 1).
The following data for each patient were extracted using the software: (1) Blink rate (BR): the number of blinks per minute; (2) Full blink rate (FBR): the number of times eyelids completely close on each other per minute. (3) Eyelid opening duration (EOD): the average time it takes, in milliseconds, for the eyelids to open. (4) Eyelid closing duration (ECD): the average time it takes, in milliseconds, for the eyelids to close. (5) Peak closing velocity (PCV): the maximum velocity, in millimeters per second, of eyes closing. (6) Peak opening velocity (POV): the maximum velocity, in millimeters per second, of eyes opening. (7) Average closing velocity (ACV): the average velocity, in millimeters per second, of eyes closing during the time. (8) Average opening velocity (AOV): the average velocity, in millimeters per second, of eyes opening during the time. (9) Palpebral aperture (PA): the vertical distance, in millimeters, between the central points of the upper and lower eyelid margins.
2.2 Statistical analysis
To achieve a 5% error margin with 95% confidence levels and 80% power, the desired sample size for this study was calculated to be 40, with the addition of one extra person to each group. Continuous variables were reported as median [interquartile range]. The gender difference between the groups was evaluated using Pearson's χ2 test, while the comparison of age between groups utilized the Kruskal-Wallis H test. To Compare blinking dynamics measurements between each group and healthy controls, a nonparametric Mann−Whitney U test was employed due to the presence of 10 subjects in each group. The effect size of Mann−Whitney U test was calculated and reported for each comparison. Data analysis was conducted using IBM SPSS Statistics for Windows, version 25.0 (Armonk, NY: IBM Corp.). Statistical significance was defined as a two-sided p < 0.05.
3 RESULTS
There was no significant difference in age and gender between groups (p = 0.731 and 0.932, respectively). Table 1 details the demographic characteristics of each group. There was no significant difference in either of studied blinking dynamics between gender groups.
| CMP | FNP | CPEO | HC | p Value | ||
|---|---|---|---|---|---|---|
| Age (years) | Median [IQR] | 33.50 [25.75−44.00] | 41.50 [27.50−51.25] | 30.50 [23.75−45.50] | 38.00 [24.25−48.50] | 0.731 |
| Gender | Female | 6 (60.0%) | 7 (70.0%) | 6 (60.0%) | 7 (70.0%) | 0.932 |
| Male | 4 (40.0%) | 3 (30.0%) | 4 (40.0%) | 3 (30.0%) |
- Abbreviations: CMP, congenital myogenic ptosis; CPEO, chronic progressive external ophthalmoplegia; FNP, facial nerve palsy; HC, healthy control; IQR, interquartile range.
Table 2 reported blink rate, blink durations, blink velocity parameters, and PA in each group of participants compared to healthy controls. Regarding between-groups differences, BR and EOD domains did not show any significant difference in either of groups compared to healthy controls. However, the FBR value was significantly lower in FNP group compared to controls; similarly, MCP and CPEO patients also had lower FBR values than controls, but these differences were not statistically significant. The ECD showed significant higher values in all three groups of patients (i.e., MCP, FNP, and CPEO) compared to healthy subjects. Concerning blink velocity parameters, all four measurements including PCV, POV, ACV, and AOV showed statistically significant lower values in each group compared to healthy controls, except for the POV domain in MCP participants, which did not differ statistically with the healthy subjects. Eventually, all groups of cases had significantly lower PA values compared to controls, and as was expected, MCP patients had the lowest values with an average of 6.96 mm of PA.
| CMP | FNP | CPEO | HC | ||
|---|---|---|---|---|---|
| BR | Median [IQR] | 21.00 [16.50−26.00] | 14.00 [11.50−20.50] | 19.00 [11.50−27.00] | 19.50 [17.25−23.50] |
| Effect sizea (r) | −0.102 | −0.348 | −0.034 | - | |
| p Value (vs. HC) | 0.648 | 0.120 | 0.879 | - | |
| FBR | Median [IQR] | 8.00 [2.00−15.00] | 3.50 [2.00−7.75] | 7.50 [4.00−15.25] | 12.50 [10.75−15.75] |
| Effect size (r) | −0.391 | −0.619 | −0.040 | - | |
| p value (vs. HC) | 0.081 | 0.006 | 0.075 | - | |
| EOD | Median [IQR] | 240.00 [206.50−262.50] | 250.00 [217.50−292.50] | 255.00 [209.00−285.00] | 211.50 [119.75−216.25] |
| Effect sizea (r) | −0.339 | −0.406 | −0.347 | - | |
| p Value (vs. HC) | 0.130 | 0.069 | 0.121 | - | |
| ECD | Median [IQR] | 98.50 [90.00−124.75] | 115.00 [100.00−143.50] | 105.00 [86.75−138.00] | 87.50 [72.75−92.75] |
| Effect sizea (r) | −0.542 | −0.817 | −0.465 | - | |
| p Value (vs. HC) | 0.015 | <0.001 | 0.037 | - | |
| PCV | Median [IQR] | 169.00 [152.25−02.50] | 153.00 [105.00−180.75] | 166.50 [135.50−205.75] | 220.00 [194.25−237.25] |
| Effect sizea (r) | −0.474 | −0.524 | −0.516 | - | |
| p Value (vs. HC) | 0.034 | 0.019 | 0.021 | - | |
| POV | Median [IQR] | 118.00 [57.50−147.75] | 55.00 [40.00−74.75] | 77.50 [40.00−115.75] | 138.50 [130.00−148.00] |
| Effect sizea (r) | −0.313 | −0.867 | −0.711 | - | |
| p Value (vs. HC) | 0.161 | <0.001 | 0.001 | - | |
| ACV | Median [IQR] | 81.00 [60.00−90.25] | 58.00 [38.50−80.00] | 69.50 [50.50−94.00] | 112.50 [109.75−124.25] |
| Effect sizea (r) | −0.677 | −0.846 | −0.745 | - | |
| p Value (vs. HC) | 0.002 | <0.001 | 0.001 | - | |
| AOV | Median [IQR] | 26.00 [18.75−31.00] | 20.00 [17.75−23.25] | 19.50 [15.75−22.00] | 34.50 [31.75−38.00] |
| Effect sizea (r) | −0.655 | −0.849 | −0.830 | - | |
| p Value (vs. HC) | 0.003 | <0.001 | <0.001 | - | |
| PA | Median [IQR] | 7.00 [6.00−7.25] | 9.00 [6.75−10.00] | 9.00 [6.80−9.25] | 10.00 [9.00−11.25] |
| Effect sizea (r) | −0.811 | −0.453 | −0.526 | - | |
| p Value (vs. HC) | <0.001 | 0.043 | 0.019 | - |
- Abbreviations: ACV, average closing velocity; AOV, average opening velocity; BR, blink rate (numbers per min); CMP, congenital myogenic ptosis; CPEO, chronic progressive external ophthalmoplegia; ECD, eyelid closing duration (ms); EOD, eyelid opening duration (ms); FBR, full blink rate (numbers per min); FNP, Facial nerve palsy; HC, healthy control; IQR, interquartile range; PA, palpebral aperture; PCV, peak closing velocity; POV, peak opening velocity;
- a Effect size of Mann−Whitney U test.
4 DISCUSSION
In this research, we compared a variety of blink parameters including blink rate, blink duration, blink velocity, and PA between subjects with CMP, FNP, CPEO, and healthy controls. Briefly, all case groups had significantly lower values in the PCV, ACV, AOV, and PA domains and significantly higher values in the ECD, compared to healthy controls. Additionally, FNP participants also had significantly lower values in the FBR and POV measures, and CPEO patients showed significantly lower values in the POV.
A study by Doane was the first to apply high-speed videography for a detailed assessment of the eyelid blink, using a camera able to capture 64 frames per second. However, it was noted that an eyelid blink comprises approximately 4 frames, and thus, 64 frames per second were insufficient to confer significant details.12 As a result, subsequent studies used the more advanced magnetic search coils to record spontaneous blink dynamics,13-15 however, this method proved to be very expensive, particularly from the clinical view. Other methods were also proposed for studying blink dynamics such as a novel magnet-based device,16 infrared sensors,17 and a method based on pupillometry noise.18 However, a recent study revealed that a smartphone camera with a resolution of 240 frames per second in 720p, would indeed be able to provide high-quality data for blinking measurements with significantly lower costs.10 Since then, this method has been used as a reliable way of recording blink dynamics in a series of studies.19 A recent review on smartphone ophthalmic imaging techniques explored utility of smartphone camera in ophthalmology work-up from anterior to posterior segments imaging extended in eyelid disorders and strabismology.20 A recent interventional study comparing the eyelid blink characteristics of patients with ptosis assessed using a smartphone camera before and after levator resection reported increased postoperative blink velocity captured by smartphone camera.21 However, it's worth noting that these studies focused on a restricted number of healthy individuals when analyzing spontaneous eyelid blinking using smartphone imaging. In contrast, our study aimed to delve into these measurements across a spectrum of disorders, namely CMP, FNP, and CPEO, characterized by eyelid movement impairments. Furthermore, we aimed to conduct a comparative analysis between patients and healthy controls to gain a more comprehensive understanding of the differences. Ultimately, in contrast to prior studies that relied on manual analysis of measurements, we employed motion analysis software to quantitatively assess blink dynamics.
Our findings indicate that patients who suffer CMP, FNP, or CPEO have significantly lower velocity values in all aspects of blinking, compared to healthy individuals. The only exception was the POV in CMP participants, revealing that the maximum velocity of eyelid closure could potentially match that of healthy individuals, and thus, the function of the muscles that close the eyelids (pretarsal orbicularis oculi and to some extent, corrugators) are partially intact in these patients. We use the term “partially” as the ACV values were still significantly lower in these patients, compared to controls. Indeed, it has been previously shown that the overactivity of the pretarsal orbicularis oculi muscles in myogenic ptosis patients presents with a reduced PA, aggregating the ptosis due to a disparity between the eyelid closing and eyelid opening muscles.22 As a result, resection of pretarsal orbicularis oculi muscle has been suggested as a method to correct ptosis, without any procedure on LPS muscle.23 Another noticeable finding was the significant reduction in the FBR values of FNP patients. This indicates the pivotal role of ophthalmologists in the acute phase of the disorder, as such low FBR could seriously result in corneal exposure of the affected eye, eventually resulting in corneal dryness, ulceration, and even blindness. This could be easily prevented by using intensive lubrication, botulinum toxin injection, or upper lid weighting.24
Although most of our findings were consistent with previously published studies, some were in contrast with their findings. In a previous study on 26 ptosis patients and 45 control subjects, cases were found to have significantly lower PA and a trend for a higher blinking duration. However, they didn't find any difference in the opening and closing velocities of the eyelids between the groups.4 Another study on 20 senile aponeurotic ptosis patients and 10 healthy controls, found lower PA and blink velocity values in the patients.25 Another study on 55 patients with Bell's palsy or Ramsay Hunt syndrome found that the PA and movement of the eyelids on the affected side were significantly reduced compared to the unaffected side.26 Blink dynamics in CPEO patients have been less investigated thorough the current literature.
Our study findings can provide better understanding of the blinking movements among individuals with eyelid movement disorders with smartphone videography which is a simple, convenient, and inexpensive way to capture eyelid movements. However, the results of this study should be interpreted in lights of a number of limitations. First, although we included three groups of patients and a control group for comparison of observed blink dynamics, a small sample size could affect final results and observed differences between groups. Second, it was a case-control study with known intrinsic limitation while a longitudinal design with larger sample sizes could confirm and expand our knowledge of videographic technique in blinking disorders. Thirdly, it is worth considering the potential influence of the Hawthorne effect on the measurements in our study. The Hawthorne effect refers to the modification of behavior in study participants due to their awareness of being observed. Finally, future studies could explore alternative image acquisition modalities, devices, and applications across different diseases. This comparative analysis would enable us to assess the efficacy of different methods and their suitability for diverse conditions.
In conclusion, our results indicated that all patients with CMP, FNP, and CPEO had significantly lower values in the PCV, ACV, AOV, and PA domains and significantly higher values in the ECD, compared to healthy controls, which is in line with previously published studies. Smartphone videography has achieved sufficient resolution and frame-rate to provide valuable information and anatomic details for clinical and research purposes. To enhance the applicability of this method specifically in clinical settings, future studies can explore the utilization of smartphone videography in a broader range of conditions.
AUTHOR CONTRIBUTIONS
Nazanin Hedayati Amlashi: Conceptualization; data curation; writing—original draft. Mohammad Taher Rajabi: Conceptualization; data curation; methodology; supervision; writing—review and editing. Mahan Shafie: Formal analysis; methodology; writing—original draft; writing—review and editing. Somayeh Heidarzadeh: Data curation; methodology. Mohammad Bagher Rajabi: Conceptualization; supervision. Seyedeh Simindokht Hosseini: Methodology. Ainaaz Haadi: Writing—original draft. Parnian Soltani: Writing—original draft.
ACKNOWLEDGMENTS
We would like to express our appreciation to the medical staff at Farabi Eye Hospital for their assistance in collecting patient data for this research. No funding was received to assist with the preparation of this manuscript.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Mohammad Taher Rajabi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis. The data that support the findings of this study are available from the corresponding author upon reasonable request.




