Evaluation of decision to delivery interval and its effect on feto-maternal outcomes in Category-I emergency cesarean section deliveries in Phuentsholing General Hospital, 2020: A retrospective cross-sectional study
Abstract
Background and Aims
When there is an immediate threat to maternal or fetal life, it is recommended to deliver within 30 min of the decision to have favorable perinatal outcomes. However, there is no data on the delivery intervals for Category-I emergency cesarean section in Bhutan. The study evaluated the decision to delivery interval (DDI) and its effect on perinatal and maternal outcomes in Category-I emergency cesarean section.
Methods
A retrospective cross-sectional study was conducted at the Phuentsholing General Hospital, Bhutan, from January 1, 2020 to December 31, 2020. Mothers who underwent Category-I emergency cesarean section were included. The demographic variables, patient transfer time, anesthesia time, operation time, DDI, and maternal and perinatal outcomes were recorded in a standard proforma. The data were analyzed using SPSS version 23.
Results
Of 78 Category-I emergency cesarean sections, only 23 (29.5%) of the cases were able to perform within 30 min of the DDI. The median (interquartile range) DDI was 37 (30–44) min. More time was taken by anesthetists to administer anesthesia (20 [15–8] min). Fetal distress (40, 51.3%) was the commonest indication. The longest DDI was around 39 min for prolonged labor, and the shortest was 26 min for failed instrumental delivery. Over half of the newborns delivered more than 30 min of DDI had low APGAR scores (25, 32.1%) at 1 min and meconium was present (23, 29.5%). Intensive care was required in 11 (14.1%), of which there was 1 (1.3%) neonatal death.
Conclusion
The Category-I emergency cesarean sections performed within recommended DDI of 30 min were much less. The main delay was due to the longer time taken for the patient transfer and time taken by the anesthetists to administer anesthesia. Perinatal outcomes were favorable when the deliveries were conducted within 30 min of DDI.
1 INTRODUCTION
Cesarean section is a commonly performed surgical intervention in obstetrical practices. The cesarean section is classified into four categories based on the urgency of the cesarean section. In Category-I cesarean section, there is an immediate threat to maternal or fetal life; in Category II, there is a maternal or fetal compromise that is not immediately life-threatening; in Category III, there is no maternal or fetal compromise but needs early delivery; and Category-IV is an elective cesarean section.1 Category-I emergency cesarean section is the most commonly performed surgical procedure to prevent maternal and perinatal mortality and morbidity. The Category-I cesarean section should be performed soon as possible and in most situations within 30 min of making a decision.1 This 30 min decision to delivery interval (DDI) is the critical time frame to deliver a distressed fetus, beyond which perinatal and maternal outcome is poor.2 Comparatively better perinatal and maternal outcomes were reported by the other researchers when the Category-I emergency cesarean sections were performed within 30 min of DDI.3, 4 However, a crash cesarean section performed rapidly to save the fetal life was found to endanger maternal life more than benefit.5 That way, the Category-I emergency cesarean section should be performed in an appropriate time frame with justification to avoid jeopardizing maternal and fetal lives.
In Bhutan, there is no information on the DDI for emergency cesarean section, and no specific recommendation has been adopted. No study was conducted in Bhutan to evaluate the DDI and its effect on maternal and fetal outcomes. It is imperative to explore and understand the time taken to perform an emergency cesarean section; that would provide more insight into adopting the international recommendations to our management protocols.
Therefore, this study was conducted to evaluate the DDI of Category-I emergency cesarean section and its effect on feto-maternal outcomes.
2 METHODS
A retrospective cross-sectional study was conducted at the Phuentsholing General Hospital, Bhutan. Ethical clearance was obtained from the Research Ethical Board of Health (REBH), Ministry of Health, Bhutan with Ref No. REBH/Approval/2021/087, dated July 19, 2021. Mothers who underwent Category-I emergency cesarean section with a period of gestation ≥24 weeks of pregnancy were recruited for the study. Informed consent was not taken since this was a retrospective study where there was no direct contact with the patients, however, patient-identifiable data were not recorded for the study. The data were collected by reviewing medical documents maintained at the maternity ward, operation room, and pediatric ward from January 1, 2020 to December 31, 2020. All the investigators are trained midwifery personnel working in the maternity ward, and they are involved in managing emergency cases during their duty hours. The medical documents were reviewed jointly by all the investigators and included only those patients who underwent Category-I emergency cesarean sections for the study. Mothers who have undergone Category II, III, and IV cesarean section, diagnosed with the fetal anomaly, intrauterine fetal death, vaginal deliveries, and incomplete documentation were excluded from the study.
2.1 Routine practice at the Phuentsholing General Hospital
The maternity ward is staffed with 18 trained midwifery nurses, two obstetricians and gynecologists, and the supporting staff. During office hours, four nurses run the ward, and during the off hours (including night shift) two nurses are on duty. In the maternity ward, a separate patient file is maintained for each patient after admission. The patient file contains all the details of the course of the stay of the patient in the hospital including the blood, urine, and imaging reports. At the time of admission, repeat blood and urine tests are performed in addition to clinical examination and ultrasound scan and electronic fetal monitoring with cardiotocography (i-CTG). All the procedures or deliveries performed during the hospital stay are recorded with date and time in the patient file by the obstetricians and gynecologists, and by the nurses on duty. The “decision for emergency cesarean section” is made after a rapid assessment of the maternal and fetal status by the obstetrician and gynecologist. Instantly after a decision is made, a preoperative preparation form for the emergency cesarean delivery is attached to the patient file signed by the obstetrician and gynecologist with the date and time. The indication for emergency cesarean section is mentioned both in the patient file and in the consent form. The preoperative order consists of obtaining written informed consent, intravenous cannulation, drawing blood for complete blood count and grouping cross-matching (if not performed previously), administration of antibiotic prophylaxis, metoclopramide and ranitidine, and urinary catheterization. Simultaneously, nurses inform the operating room and activate the operating team including the scrub nurses and the anesthetist; at the same time, other nurses prepare the patient for the emergency cesarean section as per the signed preoperative form. The nurses document the preoperative orders carried out with the date and time against medications or procedures performed. The patient is shifted to the operation room along with her file, and upon reaching the operation room the patient is received by the anesthetic technicians and the scrub nurses; and placed the patient to the operation table. A separate register (OR register) is maintained in the operation room by the scrub nurse and records the “patient received time,” along with the documentation of indications and details of the procedures. Then the anesthetists take over the patient and administer the anesthesia (either spinal or general). The anesthetists maintain a standard anesthetic monitoring chart where they record the “starting time of giving anesthesia” and the “time of successful administration.” All the vital signs and the medications administered during the surgery are recorded in the anesthetic monitoring chart. After achieving successful anesthesia, a cesarean section is performed starting with the skin incision, and the scrub nurse note down the skin incision timing as “operation starting time.” When the baby is delivered, the baby is handed over to the pediatrician or the medical officer on duty and the “delivery time” is recorded by the scrub nurse. After the delivery of the baby, the placenta and membrane are delivered, and the uterine incision is closed followed by rectus and skin closure respectively. A time is recorded corresponding to the end of skin closure as “end of operation time.” At the end of the cesarean section, the patient is transferred back to the maternity ward along with the postoperative order and kept under closed monitoring in a postoperative room. The scrub nurse records the time when the patient is transferred back to the maternity ward in the OR register. The details of the newborn including the appearance, pulse, grimace, activity, and respiration (APGAR) scores, birth weight, and sex of the newborn baby are recorded in a neonatal record book. During the postoperative period in the maternity ward, the patient is monitored for vital signs according to the signed postoperative order and recorded in the patient file. The patient is discharged home on postoperative Day 3 if vitals are stable and the cesarean wound is healthy; and if there is discharge from the wound, then the patient is kept in the ward for a few more days on antibiotics for surgical site infections.
-
Category-I emergency cesarean section1: An immediate threat to the life of the woman or fetus which needs delivery of the fetus within 30 min.
-
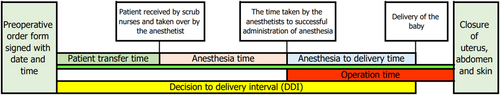
Patient transfer time: The time taken by the nurses to prepare the patients for the emergency cesarean section starting from the preoperative order form signed with the date and time by the obstetrician and gynecologist, to the time patient is received by the anesthetic technicians and the scrub nurses in the operation room.
-
Anesthesia time: The time taken from the arrival of the patient to the operation theater and taken over by the anesthetists to the successful administration of anesthesia.
-
Anesthesia to delivery time: It is the time taken from successful administration of anesthesia to delivery of the baby.
-
Operation time: It is the time taken from the skin incision to the delivery of the baby to the end of closure of the abdominal skin.
-
DDI: The total time taken starting from the decision (preoperative order form signed by the obstetrician and gynecologist with date and time) to delivery of the baby. DDI is the sum of “patient transfer time” + “anesthesia time” + “anesthesia to delivery time” (Figure 1).
-
Perinatal outcome: APGAR score <7 is unfavorable and APGAR score ≥7 is favorable perinatal outcome.
2.2 Statistical analysis
The collected data were captured and double-entered using Epi data 3.1.2 (Odense, Denmark) and validated to avoid data entry errors. The data were then exported and analyzed using SPSS version 23. Descriptive data were presented as median (interquartile range [IQR]) or mean (SD) for continuous variables and numbers and percentages for categorical variables. The χ2 and Fisher's exact test were used for qualitative variables and Student's t-test was used for quantitative variables. A Pearson's correlation coefficient test was used to measure the statistical correlation between two continuous variables. A multiple logistic regression analysis was used to ascertain the predictors of poor maternal and fetal outcome. A p < 0.05 was considered statistically significant with a confidence interval of 95%.
3 RESULTS
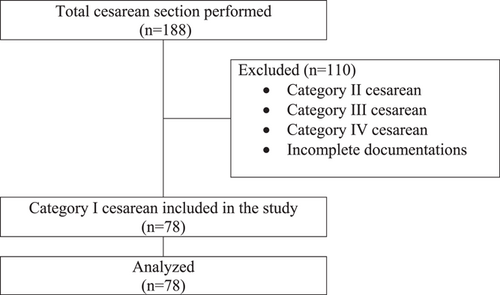
A total of 188 women underwent cesarean sections at the Phuentsholing General Hospital in the year 2020. After reviewing the medical documents, 110 cesarean sections were excluded from the study due to incomplete documents and cesarean sections performed for Category II, III, and IV. A total of 78 women who underwent Category-I emergency cesarean section were included in the study (Figure 2).
3.1 DDI
There were 78 Category-I emergency cesarean sections performed in the year 2020. Of the 78 cases, only 23 (29.5%) of cases Category-I emergency cesarean sections were able to perform within 30 min of the DDI. The median (IQR) of DDI was 37 (30–44) min, and the median (IQR) time taken by anesthetists to administer anesthesia and patients transferring to the operation theater time was 20 and 13 min, respectively (Table 1).
| Decision to delivery interval | n (%) |
|---|---|
| ≤30 min | 23 (29.5) |
| >30 min | 55 (70.5) |
| Decision to different activity time (minutes) | Median (IQR) |
|---|---|
| Decision to patient transfer time | 13 (12–15) |
| Time taken to give anesthesia | 20 (15–28) |
| Anesthesia to delivery time | 3 (2–5) |
| Operation time | 25 (23–30) |
| Decision to delivery interval | 37 (30–44) |
- Abbreviation: IQR, interquartile range.
3.2 Characteristics of the study population
Half of the study subjects were in the age range of 26–35 years. There were 37 (47.4%) multigravida and 34 (43.6%) multiparous patients. The majority (58, 74.4%) of the patients were in term pregnancy. Almost all cases (77, 98.7%) of Category-I emergency cesarean sections were performed under spinal anesthesia, except in one case spinal was converted to general anesthesia after failing spinal anesthesia. The characteristics of the study population were comparable between those delivered within 30 min and those performed after 30 min of the DDI (Table 2).
| Decision to delivery interval, n (%) | |||
|---|---|---|---|
| Variables | ≤30 min | >30 min | Total, n (%) |
| Age (years) | |||
| <18 | 1 (4.3) | 1 (1.8) | 2 (2.6) |
| 18–25 | 2 (8.7) | 13 (23.6) | 15 (19.2) |
| 26–35 | 13 (56.5) | 26 (47.3) | 39 (50.0) |
| 36–45 | 7 (30.4) | 15 (27.3) | 22 (28.2) |
| Gravida | |||
| Primigravida | 8 (34.8) | 28 (50.9) | 36 (46.2) |
| Multigravida | 15 (65.2) | 22 (40.0) | 37 (47.4) |
| Grand multigravida | 0 (0.0) | 5 (9.1) | 5 (6.4) |
| Parity | |||
| Nulliparous | 9 (39.1) | 32 (58.2) | 41 (52.6) |
| Multiparous | 14 (60.9) | 20 (36.4) | 34 (43.6) |
| Grand multipara | 0 (0.0) | 3 (5.5) | 3 (3.8) |
| Gestational age (weeks) | |||
| Preterm | 8 (34.8) | 12 (21.8) | 20 (25.6) |
| Term | 15 (65.2) | 43 (78.2) | 58 (74.4) |
| Types of anesthesia | |||
| Spinal anesthesia | 23 (100.0) | 54 (98.2) | 77 (98.7) |
| General anesthesia | 0 (0.0) | 1 (1.8) | 1 (1.3) |
- Abbreviation: DDI, decision to delivery interval.
3.3 Indications for Category-I emergency cesarean section
The commonest indication for the Category-I emergency cesarean section was fetal distress (40, 51.3%). Other indications were; prolonged labor (due to obstructed labor), pre-eclampsia and eclampsia, antepartum hemorrhage (placenta previa totalis and abruptio placenta), impending uterine rupture (past cesarean section with scar tenderness), and cord prolapse seen in 19 (24.4%), 9 (11.5%), 5 (6.4%), 3 (3.8%), and 1 (1.3%), respectively. The maximum DDI was around 39 min for prolonged labor, fetal distress, cord prolapse, and impending uterine rupture, and the shortest DDI was 26 min for failed instrumental delivery (Table 3).
| Indications | Decision to delivery interval, n (%) | |||
|---|---|---|---|---|
| ≤30 min | >30 min | Total, n (%) | DDI (min), mean (SD) | |
| Prolonged labor | 5 (21.7) | 14 (25.5) | 19 (24.4) | 39.0 (10.8) |
| Fetal distress | 12 (52.2) | 28 (50.9) | 40 (51.3) | 39.8 (10.7) |
| Cord prolapse | 0 (0.0) | 1 (1.8) | 1 (1.3) | 39.0 (0.0) |
| Impending uterine rupture | 0 (0.0) | 3 (5.5) | 3 (3.8) | 39.0 (7.9) |
| Severe PE/eclampsia | 3 (13.0) | 6 (10.9) | 9 (11.5) | 35.2 (4.7) |
| Failed instrumental delivery | 1 (4.3) | 0 (0.0) | 1 (1.3) | 26.0 (0.0) |
| Antepartum hemorrhage | 2 (8.7) | 3 (5.5) | 5 (6.4) | 33.6 (6.7) |
| Total | 23 (100.0) | 55 (100.0) | 78 (100.0) | 38.5 (9.9) |
- Abbreviations: DDI, decision to delivery interval; PE, pre-eclampsia; SD, standard deviation.
3.4 Category-I emergency cesarean performed by hours of the day
Of 23 cases performed within 30 min of DDI, 19 (82.6%) were conducted during office hours. The likelihood of achieving a DDI of 30 min when performed during office hours is 12.7-fold (95% CI: 3.7–43.3, p = 0.001). The mean (SD) of DDI for after office hours is 42.14 (9.8) min and it is significantly higher than the mean (SD) of DDI for “office hours” (p = 0.001) (Table 4).
| DDI, n (%) | |||||
|---|---|---|---|---|---|
| Hours of the day | <30 min | >30 min | Total, n (%) | OR (95% CI) | p-value |
| Office hours | 19 (82.6) | 15 (27.3) | 34 (43.6) | 12.7 (3.7–43.3) | 0.001a |
| After office hours | 4 (17.4) | 40 (72.7) | 44 (56.4) | ||
| Mean ± SD of DDI for office hours (min) | 33.7 ± 7.8 | 0.001b | |||
| Mean ± SD of DDI for after office hours (min) | 42.14 ± 9.8 | ||||
- Abbreviations: DDI, decision to delivery interval; OR, odds ratio; SD, standard deviation.
- a χ2 test.
- b Student's t test.
3.5 Perinatal outcome and DDI
The perinatal outcomes were poor when delivered after 30 min of DDI. The APGAR score was low (<7 scores) at 1 min of birth in 25 (32.1%) of the newborns. Of these, the majority of the babies with low APGAR scores were delivered after 30 min of DDI. The chance of delivering a baby with a low APGAR score (<7 scores) was 77% less when delivered within 30 min of DDI (95% CI: 0.23 [0.60–0.85], p = 0.021). Meconium was present in 23 (29.5%) newborns. The majority (21, 38.2%) of babies with meconium were delivered after 30 min of DDI. The chance of having meconium was 85% less when the babies were delivered within 30 min of DDI (0.15 [0.03–0.73], p = 0.011). Intensive care was required in 11 (14.1%) cases, of which there was 1 (1.3%) neonatal death (Table 5).
| Decision to delivery interval, n (%) | |||||
|---|---|---|---|---|---|
| Perinatal outcomes | ≤30 min (n = 23) | >30 min (n = 55) | Total, n (%) | OR (95% CI) | p-valuea |
| Apgar score at 1 min | |||||
| <7 score | 3 (13.0) | 22 (40.0) | 25 (32.1) | 0.23 (0.60–0.85) | 0.021 |
| ≥7 score | 20 (87.0) | 33 (60.0) | 53 (67.9) | ||
| Apgar score at 5 min | |||||
| <7 score | 1 (4.3) | 6 (10.9) | 7 (8.9) | 0.37 (0.04–3.27) | 0.372 |
| ≥7 score | 22 (95.7) | 49 (89.1) | 72 (92.3) | ||
| Presence of meconium | |||||
| Present | 2 (8.7) | 21 (38.2) | 23 (29.5) | 0.15 (0.03–0.73) | 0.011 |
| Absent | 21 (91.3) | 34 (61.8) | 55 (70.5) | ||
| Immediate neonatal resuscitation | |||||
| Yes | 1 (4.3) | 12 (21.8) | 13 (16.7) | 0.16 (0.02–1.34) | 0.093 |
| No | 22 (95.7) | 43 (78.2) | 65 (83.3) | ||
| Intensive care | |||||
| Yes | 1 (4.3) | 10 (18.2) | 11 (14.1) | 0.20 (0.02–1.70) | 0.162 |
| No | 22 (95.7) | 45 (81.8) | 67 (85.9) | ||
| Perinatal death | |||||
| Yes | 0 (0.0) | 1 (1.8) | 1 (1.3) | ||
| No | 23 (100.0) | 54 (98.2) | 77 (98.7) | ||
- Abbreviations: CI, confidence interval; OR, odds ratio.
- a χ2 test.
3.6 Relation of indications for Category-I emergency cesarean section to perinatal outcome
Among the 25 cases with low APGAR score (<7) at 1 min of birth, the fetal distress (11, 44%) presented the maximum cases with low APGAR score followed by prolonged labor (6, 24%). The lowest mean (SD) of APGAR score was seen with the cord prolapse and failed instrumental delivery; however, the mean differences between the indications for the emergency cesarean section are comparable (p = 0.84) as shown in Table 6.
| Apgar score at 1 min | |||||
|---|---|---|---|---|---|
| Indications | Total | <7 | ≥7 | Mean (SD) | p-valuea |
| Prolonged labor | 19 (24.3) | 6 (24) | 13 (24.5) | 7.6 (1.4) | 0.84 |
| Fetal distress | 40 (51.3) | 11 (44) | 29 (54.7) | 7.4 (1.8) | |
| Cord prolapse | 1 (1.3) | 1 (4) | 0 (0.0) | 6 (0.0) | |
| Impending uterine rupture | 3 (3.8) | 1(4) | 2 (3.8) | 7.3 (1.2) | |
| Pre-eclampsia/eclampsia | 9 (11.5) | 3 (12) | 6 (11.3) | 7.8 (1.4) | |
| Failed instrumental delivery | 1 (1.3) | 1 (4) | 0 (0.0) | 6 (0.0) | |
| Antepartum hemorrhage | 5 (6.4) | 2 (8) | 3 (5.7) | 6.8 (2.9) | |
| Total | 78 (100) | 25 (100) | 53 (100) | 7.4 (1.7) | |
- a χ2 test.
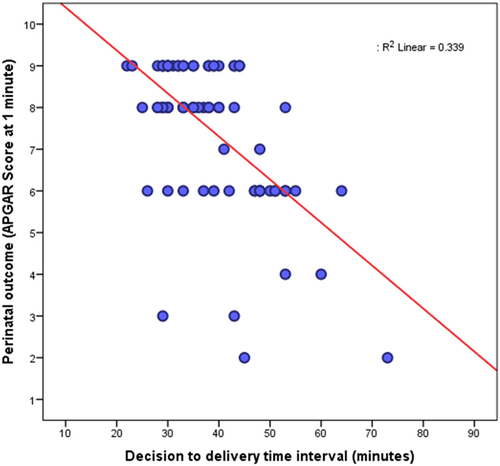
3.7 Correlation of DDI and perinatal outcome
The perinatal outcome was unfavorable with the increase in the length of the DDI. There was a significant negative correlation between the decision to the delivery time interval and perinatal outcome; r = −0.44, p = 0.012 (Figure 3).
3.8 Predictors of the poor perinatal outcome (low APGAR score)
Perinatal outcomes (based on APGAR scores) were taken as dependent variables, and the factors (age, gravida, parity, gestational age, patient transfer time, DDI, anesthesia time, and hours of the day) were considered as independent variables. The combined effect of the factors on the perinatal outcomes were studied using the logistic regression test. Primigravida is five times more likely to have poor perinatal outcome (low APGAR score) as compared with multigravida, however, it is not significant (OR: 5.06, 95% CI: 0.85–29.82, p = 0.073). Babies delivered within 30 min of DDI has favorable perinatal outcome as compared with DDI more than 30 min (OR: 0.68, 95% CI: 0.51–0.91, p = 0.009). The details are summarized in Table 7.
| Characteristics | β | SE | Wald | p-value | OR (95% CI) |
|---|---|---|---|---|---|
| Age | −0.040 | 0.080 | 0.255 | 0.613 | 0.96 (0.82–1.12) |
| Gravida | 1.622 | 0.905 | 3.213 | 0.073 | 5.06 (0.85–29.82) |
| Parity | −1.251 | 0.876 | 2.039 | 0.153 | 0.28 (0.05–1.59) |
| Gestational age | 0.316 | 0.186 | 2.892 | 0.089 | 1.37 (0.95–1.97) |
| Patient transfer time | 0.246 | 0.156 | 2.490 | 0.114 | 1.27 (0.94–1.73) |
| Anesthesia time | 0.113 | 0.133 | 0.729 | 0.393 | 1.11 (0.86–1.45) |
| DDI | −0.377 | 0.146 | 6.642 | 0.009 | 0.68 (0.51–0.91) |
| Hours of the day | −0.930 | 0.954 | 0.949 | 0.330 | 0.39 (0.06–1.56) |
| Constant | −1.625 | 6.535 | 0.062 | 0.803 | 0.197 |
- Abbreviation: DDI, decision to delivery interval.
3.9 Maternal outcomes
The main maternal complications observed were postoperative fever and surgical site infections. Fever was present in 13 (30.2%) of the mothers, of which 6 (7.7%) had surgical site infections. Anticonvulsant was administered in 9 (20.9%) and 8 (18.6%) cases that required blood transfusion. The maternal outcomes were comparable between deliveries conducted within 30 min and after 30 min (Table 8).
| Maternal outcomes | Decision to delivery interval, n (%) | ||||
|---|---|---|---|---|---|
| ≤30 min | >30 min | Total, n (%) | OR (95% CI) | p-valuea | |
| Fever | |||||
| Yes | 4 (17.4) | 9 (16.4) | 13 (16.7) | 1.1 (0.29–3.92) | 0.575 |
| No | 19 (82.6) | 46 (83.6) | 65 (83.3) | ||
| Surgical site infection | |||||
| Yes | 2 (8.7) | 4 (7.3) | 6 (7.7) | 1.2 (0.21–7.14) | 0.576 |
| No | 21 (91.3) | 51(92.7) | 72 (92.3) | ||
| Perioperative blood transfusion | |||||
| Yes | 2 (8.7) | 6 (10.9) | 8 (10.3) | 0.78 (0.15–4.17) | 0.564 |
| No | 21 (91.3) | 49 (89.1) | 70 (89.7) | ||
| Use of diuretics | |||||
| Yes | 4 (17.4) | 3 (5.5) | 7 (9.0) | 3.65 (0.75–17.83) | 0.109 |
| No | 19 (82.6) | 52 (94.5) | 71 (91.0) | ||
| Use of anticonvulsant | |||||
| Yes | 4 (17.4) | 5 (9.1) | 9 (11.5) | 2.1 (0.51–8.68) | 0.437 |
| No | 19 (82.6) | 50 (90.9) | 69 (88.5) | ||
- Abbreviations: CI, confidence interval; OR, odds ratio.
- a χ2 test.
4 DISCUSSION
Category-I emergency cesarean sections were able to perform within 30 min only in 29.5% of the cases. In an emergency, it is critical to deliver the baby as first as possible to prevent further compromising perinatal outcomes and or to prevent fatal maternal complications. American College of Obstetricians and Gynecologists (ACOG), Royal College of Obstetricians and Gynaecologists (RCOG), and National Institute for Health and Care Excellence (NICE) guidelines recommend performing a Category-I cesarean section within 30 min of DDI.6 However, in reality, it is challenging to deliver within that critical time frame of 30 min of DDI. Few studies have reported a much lesser percentage of delivery conducted within 30 min of recommended DDI.7, 8 In the study of Ayele et al.9 delivery within 30 min of the decision was achieved only in 17.5%.9 A similar finding was reported by Kitaw et al.10 study, where the DDI was achieved in 20.3%.10 Other studies have reported better achievement of DDI within 30 min ranging from 60% to 71%.11-13 One study reported 100% of Category-I emergency cesarean sections were performed within 30 min of DDI.14 However, the majority of the published literature showed not able to meet the recommended DDI of 30 min. In Phuentsholing Hospital, the reasons for not being able to perform Category-I cesarean within 30 min of decision is probably due to an acute shortage of staff in the maternity ward, labor room, operation theater, and on top, many staff were engaged in COVID-19 containment activities during the pandemic year 2020.
The median DDI was 37 min in the current study. The median time taken for patient transfer and the time taken by the anesthetist to administer anesthesia was 13 and 20 min, respectively. It was observed that in total over 30 min were spent on patient transfer and anesthesia time alone. In the current study, patient preparation and transfer time are inclusive of waiting time to gather logistics, laboratory reports, and waiting time for the arrival of operating teams. Similar factors delaying performing emergency cesarean section were reported in other studies.6 A study by Hirani et al.7 reported a much longer median DDI of 60 min as compared with 37 min in the current study.4, 7, 15 Gupta et al.16 and Temesgen et al.17 reported more time was spent on collecting the surgical materials, preparation, and shifting the patient to the operation theater.16, 17
In the present study, more than half of the emergency cesarean sections were performed during off-hours. The mean time taken to perform an emergency cesarean section during “off-hours” was significantly higher as compared with those performed during “office hours” (42.1 vs. 33.7 min). The study finding is contrary to Khemworapong et al.8 study showed a shorter time was taken when the emergency cesarean section was performed during the “off-hours.”8 Over 80% of the emergency cesarean performed during office hours achieved a DDI of 30 min. Emergency cesarean performed during office hours is 12 times more likely to achieve a DDI of 30 min. This is because, during the office hours, all the units are functional, and the operating teams are in the station. Emergencies are unpredictable and can occur at any time of the day or night. The operation performed after office hour requires the activation of the on-call operating team. In the local scenario, a hospital utility vehicle has to go and pick up staff residing outside the hospital campus. In this way, emergency cesarean section cases are kept waiting till all the on-call operating teams reach the operation theater. In an attempt to administer anesthesia, often junior anesthetists require more time to administer spinal anesthesia by making multiple repeated pricks. The learning curve for the junior anesthetists has high threshold and they need to perform at least 50 attempts to administer spinal anesthesia to gain the required appropriate skills.18, 19 Sometimes, spinal anesthesia does not work or fails and needs to convert to general anesthesia. Converting to general anesthesia takes another half an hour extra.20 In a few cases, the surgeon finds difficulty in opening the peritoneal cavity due to massive adhesion and taking a long time to operate. In some acute emergency cases, especially in severe pre-eclampsia and eclampsia, initial maternal resuscitation and stabilization are required before taking for emergency cesarean section. These are the likely reasons for not being able to perform an emergency cesarean section within 30 min of DDI.
In more than half of the cases, emergency cesarean sections were performed for fetal distress followed by 24% for prolonged labor (obstructed labor) in the current study. The longest time taken was around 39 min for fetal distress and prolonged labor, and the shortest time taken was 26 min for failed instrumental vaginal delivery. In Khemworapong et al.8 study, the most common indications were obstructed labor (due to cephalopelvic disproportion) followed by impending uterine rupture. In the same study, the shortest DDI was 47 min for fetal distress (nonreassuring fetal heart rate tracing) as compared with other indications for Category-I emergency cesarean.8 Similar indications for the Category-I cesarean section were reported in other studies.21, 22 The prolonged labor with a fetus in distress is supposed to deliver as soon as possible to prevent further jeopardizing the fetus and or mother, but due to unavoidable circumstances, the distressed fetus has to deliver beyond the recommended time of delivery. Most of the published articles have used the term “fetal distress,” however it is too broad and vague to be applied with any precision to clinical situations.23 In the current study, the Category-3 fetal heart rate tracing, a nonreassuring fetal status that required immediate intervention is labeled as fetal distress.24 Pre-eclampsia/eclampsia is not an indication for emergency cesarean section.23 However, in the current study, nine cases underwent emergency cesarean section for having uncontrolled severe hypertension with features of HELLP syndrome and nonreassuring fetal status.
Around one-third of the newborn had a low APGAR score (<7) at 1 min, and in about 9% of the cases low APGAR score persisted even after 5 min. Approximately half of the babies with low APGAR scores were delivered after 30 min of DDI, and most of the babies delivered after 30 min of DDI had meconium at birth. However, the need for immediate neonatal resuscitation, intensive care, and perinatal death was comparable for babies delivered after 30 min of DDI. Boriboonhirunsarn et al. study showed a comparable perinatal outcome across the categories of DDI.21 On contrary, other studies had shown an unfavorable perinatal outcome when babies were delivered after 75 min of DDI2; however, no significant difference was found between the APGAR scores of babies delivered within 30 min and after 30 min of DDI.25 The unfavorable perinatal outcomes observed in the current study were partly due to the failure to perform a Category-I emergency cesarean section within 30 min of DDI due to unavoidable circumstances. However, the APGAR score alone is not a good predictor of poor perinatal outcomes. APGAR score has to be considered in combination with other clinical parameters of the baby and associated maternal and fetal risk factors while assessing for the perinatal outcome.26
Over one-third of the mothers had fever during the postoperative period, and out of which only 7.7% had surgical site infection. The temperature rise is expected immediately in the recovery and postoperative period, and it does not necessarily mean infection. It is often due to the body's response to tissue trauma and the release of inflammatory agents and foreign bodies that occurred during surgery.27 Infection at the cesarean section site is usually higher for emergencies as compared with elective cesarean section. In dare emergencies, minimal time is spent on surgical safety measures, and operation is performed rapidly to save the life of the fetus and or the mother with minimal or compromising sterility. Emergency cesarean section is considered contaminated surgery; there is contamination and injury to the surrounding tissues and, more bleeding and hematoma as compared with elective cesarean section. These are the possible reasons for more surgical site infections in emergency cases.28
Less than one-quarter of mothers received a blood transfusion in the current study. Bhutanese women get pregnant in an anemic state and get worsen with the progression of pregnancy.29 In a crash emergency cesarean section, the intention is to take out the distressed fetus rapidly. In the process, often emergency cesarean section is challenged with massive bleeding due to inadvertently injuring the vessels. The mild to moderate blood loss aggravates anemia and patient who underwent emergency cesarean section are likely to receive blood transfusions more often. In another one-quarter of the mothers, anticonvulsant magnesium sulfate (MgSO4) was administered. The MgSO4 was administered for severe pre-eclamptic patients as prophylaxis to prevent eclampsia, and as a therapeutic treatment for eclamptic patients. However, the maternal complications are comparable between the deliveries conducted within 30 min of DDI and after 30 min of DDI. Temesgen et al.17 study showed that the DDI was longer than the recommended time but it did not have an effect on the maternal and perinatal outcomes.17
This study was not without limitations. The study was conducted retrospectively by reviewing the medical documents and the results are based on the available data from the medical record. During the review of the medical records, many patient files were not documented properly. Documentation is very poor in Bhutan and conducting retrospective research is challenging.
The study sample size was comparatively less since the study was conducted by reviewing the data for the year 2020 only, however, the post hoc power analysis showed acceptable power of 96% for the sample size of 78.
This study was conducted on Category-I emergency cesarean section. Retrospectively categorizing the emergency cesarean section is challenging. There could have been some recall bias in categorizing the emergency cesarean section into Category-I in the current study. However, the categorization was performed by the investigators who were involved directly in the management of the emergency patients during their duty hours. So, the chances of wrongly classifying the patients into a different category of emergency cesarean sections were almost nil.
The current study was conducted during the pandemic year and contributed to the low achievement of DDI, however, during the pandemic year, the maternity ward, labor room, operation theater, and pediatric wards were kept functional. Although routine medical services were kept closed, the emergency services were kept open as usual. During the pandemic, there was an acute shortage of staff in the hospital since many were diverted to handle the pandemic; however, the majority of the staff were mobilized from the Outpatient Department, and sufficient in-ward staff were kept in the hospital to manage emergencies and to provide services to warded patients. The maternity ward was run by 2–4 trained midwifery nurses on 6 h duty on shift during the pandemic.
This study explored the time taken for patient preparation to the administration of anesthesia to delivery of the baby, and the study finding showed more time was spent on patient preparation and transferring to the operation theater, and by the anesthetists to administer anesthesia and hampering the delivery of the baby within 30 min of the decision to deliver. This study finding leaves an opportunity for the researchers to further study the likely reasons for the delay in performing an emergency cesarean section, and to explore possible ways to improve the service delivery to ensure acute emergency cases are delivered within the recommended time interval.
5 CONCLUSION
The DDI of 30 min was achieved only in 29.5% of cases. The Category-I emergency cesarean sections performed within 30 min of DDI were associated with favorable perinatal outcomes. It is challenging to conduct an emergency cesarean section within 30 min of the decision to delivery. There is a need to establish a “Category-I cesarean section” protocol within the local hospital to facilitate the rapid and safe conduct of cesarean delivery in a dire emergency.
AUTHOR CONTRIBUTIONS
Yeshey Dorjey: Conceptualization; data curation; formal analysis; methodology; resources; software; supervision; validation; visualization; writing – original draft. Yezer Tshomo: Data curation; methodology; validation; visualization; writing – original draft. Dorji Wangchuk: Conceptualization; data curation; methodology; validation. Purushottami Bhandari: Data curation; investigation; methodology; validation. Choki Dorji: Conceptualization; formal analysis; methodology; validation; visualization. Diptika Pradhan: Data curation; investigation; methodology; validation; visualization. Rinzin Pemo: Data curation; investigation; methodology; software; validation.
ACKNOWLEDGMENTS
The authors would like to acknowledge Dr. Deep Kiran Chhetri, consultant obstetrician, and gynecologist, Trashigang Hospital, Bhutan for his kind review and corrections.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Yeshey Dorjey affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




