Efforts at making the diagnosis of acute-onset autoimmune hepatitis†
Potential conflict of interest: Nothing to report.
We read with great interest the article by Stravitz et al.,1 who report that patients with indeterminate acute liver failure (ALF) often have features of autoimmune hepatitis (AIH) according to histological, serological, and clinical analyses. Fifty-eight percent of their patients with indeterminate ALF were diagnosed with probable AIH-ALF on the basis of pathological features, and they had higher serum globulin levels and higher levels of anti-nuclear antibodies, anti–smooth muscle antibodies, or both in comparison with patients without histological findings suggestive of probable AIH-ALF.
As hepatologists struggling against intractable liver diseases in Japan, we applaud their efforts at making the diagnosis of acute-onset AIH.
In past Japanese surveys of ALF, a specific etiology could not be identified in 30% to 40% of adult patients.2 Since the establishment of the criteria of the International Autoimmune Hepatitis Group3 and the recognition of acute-onset AIH, patients with autoimmune ALF have begun to be diagnosed.4 However, in the early stages of their illness, they often demonstrate a histological pattern atypical for AIH that consists of centrilobular necrosis with or without portal changes.5-7
Recently, we have also reported that AIH is not a rare cause of ALF in our unit, and the number of patients with unknown causes could decrease according to the precise diagnosis of AIH, which is based on a combination of the aforementioned pathological features and the original revised criteria.8 In our unit, AIH has been involved in 29% of ALF cases, and unknown causes have been involved in 12%; this means that in comparison with the results of a national survey, approximately half of our patients with unknown causes have been diagnosed with AIH-ALF.
In our recent studies,7-10 the severity of acute-onset AIH was not high at its onset in most patients, but some of them advanced to severe diseases without a precise diagnosis or treatment. For an early diagnosis, it is most important to exclude other causes systematically, to remember acute-onset AIH in the differential diagnosis, and then to apply the scoring system; comprehensive evaluations of clinical, biochemical, radiological, and histological features are necessary. In particular, a precise pathological evaluation plays an important role in the differential diagnosis, as the authors describe. However, this is complicated by the fact that there is still no gold standard for making the diagnosis of acute-onset AIH, as the authors repeatedly note.
We believe that one of the pathological characteristics of acute-onset AIH is its histological heterogeneity, especially in severe and fulminant AIH. Histological heterogeneity leads to radiological heterogeneity. Unenhanced computed tomography often shows hypoattenuated and hyperattenuated areas, with the former reflecting massive hepatic necrosis and the latter reflecting regenerative islands. Ultrasound shows similar heterogeneity. Histological heterogeneity also leads to clinical heterogeneity. The time from onset to admission to our unit did not differ with the clinical severity (nonsevere, severe, or fulminant), and the time from onset to histological examination did not differ with the histological features (chronic hepatitis, severe acute hepatitis, or massive/submassive necrosis; Fig. 1).
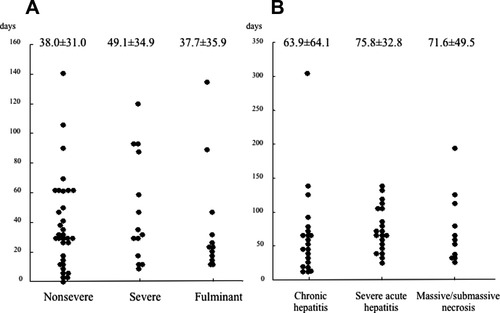
Associations between (A) the clinical severity and the time from onset to admission and (B) the histological features and the time from onset to histological examination.
Characteristic morphological patterns of liver necrosis and regeneration should exist in patients with acute-onset AIH, and a better understanding of these patterns would be helpful in making the diagnosis.
References
Keiichi Fujiwara M.D.*, Shin Yasui M.D.*, Osamu Yokosuka M.D.*, * Department of Medicine and Clinical Oncology, Graduate School of Medicine, Chiba University, Chiba, Japan.




