Prevalence of non-convulsive seizures and electroencephalographic abnormalities in critically ill patients—A retrospective observational study
Abstract
Objective
Electroencephalographic (EEG) abnormalities especially non-convulsive status epilepticus (NCSE) have been found to be associated with worse outcomes in critically ill patients. We aimed to assess the prevalence of non-convulsive seizures and electroencephalographic abnormalities in critically ill patients. Furthermore, we aimed to investigate any association between the type of EEG abnormality and outcomes including ICU mortality and successful ICU discharge.
Methods
This was a cross-sectional observational study carried out among critically ill patients in a mixed medical-surgical ICU from January 1, 2018 to May 15, 2020. A total of 178 records of 30 min bedside EEG records were found. EEG findings were grouped as normal, non-convulsive seizures (NCS), non-convulsive status epilepticus (NCSE), and other abnormalities. Descriptive analytical tools were used to characterize the case details in terms of the type of EEG abnormalities. Chi square test was used to describe the EEG abnormalities in terms of mortality. The status epilepticus severity scores (STESS) were further calculated for records with NCSE. These data were then analyzed for any association between STESS and mortality for cases with NCSE.
Results
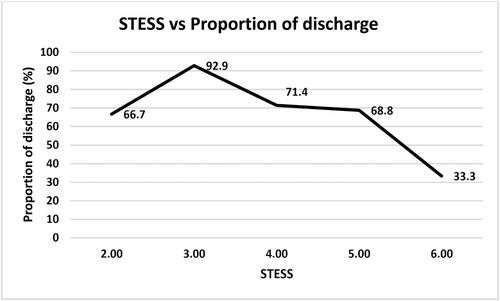
The prevalence of EEG abnormality in our cohort of all critically ill patients was found to be 7.3% (170/2234). Among the patients with altered sensorium in whom EEG was done, 42.9% had non-conclusive seizure activity with 25.2% in NCSE. Though the study was not adequately powered, there was a definite trend towards a lower proportion of successful ICU discharge rates seen among patients with higher STESS (>2) with only 33.3% being discharged for patients with a STESS of 6 versus 92.9% for those with STESS 3.
Significance
When combined with a strong clinical suspicion, even a 30-min bedside EEG can result in detection of EEG abnormalities including NCS and NCSE. Hence, EEG should be regularly included in the evaluation of critically ill patients with altered sensorium.
Plain Language Summary
Electroencephalographic (EEG) abnormalities and seizures can have high prevalence in critically ill patients. These abnormalities notably, non-convulsive status epilepticus (NCSE) has been found to be associated with poor patient outcomes. This was a retrospective observational study analyzing 178 EEG records, from a mixed medical-surgical ICU. The indication for obtaining an EEG was based solely on the clinical suspicion of the treating physician. The study found a high prevalence of EEG abnormalities in 96.5% in whom it was obtained with 42.9% having any seizure activity and 28.8% having NCSE. The study was not powered for detection of association of the EEG abnormalities with clinical outcomes. However, a definite trend towards decreased chances of successful discharge from the ICU was seen. This study used strong clinical suspicion in patients with altered sensorium to obtain an EEG. High detection rates of EEG abnormalities were recorded in this study. Hence, combination of clinical judgement and EEG can improve detection of EEG abnormalities and NCSE.
Key points
- Electroencephalographic abnormalities are being increasingly identified in critically ill patients.
- These EEG abnormalities especially non-convulsive seizures (NCS) and non-convulsive status epilepticus (NCSE) have been associated with worse patient outcomes.
- Early detection and management can be the difference between successful discharge and mortality in many patients.
- Detection of EEG abnormalities can be improved when EEG is combined with a strong clinical index of suspicion.
1 INTRODUCTION
Alteration in mental status is a commonly encountered problem in the ICU. Across the various etiologies of altered mental status, electroencephalographic (EEG) abnormalities are increasingly being reported to be more common than previously thought.1-3 In patients with altered sensorium or coma, the prevalence of non-convulsive status epilepticus (NCSE) has been found to range from 8% to 40% depending on the population type and the duration of EEG examination that is, continuous or 30-min examination.1, 4-7 These EEG abnormalities, especially non convulsive seizures (NCS) and NCSE have been linked unfavorably to patient outcomes in terms of length of ICU stay, length of hospital stay, morbidity, and even mortality.5, 8-12 But because of their undramatic, non-convulsive nature with only a few if any subtle clinical signs, they are often not diagnosed, or diagnosed very late during the course of treatment.13 Studies have found delays of as much as 24 h in detecting the first seizure activity during sessions of continuous EEG monitoring.14, 15 Prognostication scores like status epilepticus severity score (STESS) have also been developed to help predict the outcomes in NCSE.9 Since the presence of and delay in detection of NCSE have been found to be adversely associated with poor outcomes, numerous studies have suggested continuous EEG monitoring in patients with unexplained low mentation. This is based on the increasing body of evidence that early detection and management of EEG abnormalities could reflect into improved patient outcomes.4, 16 However, in many parts of the world especially in low middle income countries, access to even 30 min EEG monitoring is very limited.8 In this 17 month retrospective hospital record based study including 178 EEG examinations of critically ill patients from a medical surgical ICU from Nepal, the investigators try to characterize the documented EEG abnormalities and their association with clinical outcomes if present. The criteria used for obtaining the EEG were based solely on the clinical decision of the treating teams. Though, the criteria used could not be standardized due to the retrospective observational nature of the study, the usual practice of ordering an EEG in this particular ICU is by the ICU physician based on the low GCS or altered sensorium which may be either not improving or fluctuating despite treatment. This often follows a multidisciplinary discussion with the neurologist and the primary admitting physician. Thus indirectly, this study evaluates the role of clinical suspicion on actual detection of EEG abnormalities especially non convulsive seizures which are possibly treatable.
2 METHODS
The study was a retrospective period prevalence cross sectional observational study done in the mixed medical surgical adult ICU of Om Hospital and Research Centre, Nepal from January 1, 2018 to May 15, 2020. Ethical approval for the study was obtained from the Institutional Review Committee of the National Health Research Council (Ref. No. 2795) and the hospital administration for the provision of the hospital records. A Proforma was used to collect the data from the hospital records. Individual patient files were screened for inclusion in the study.
2.1 Study population
A single inclusion criterion of all patients admitted to the ICU with altered sensorium undergoing EEG as a part of their diagnostic work-up was used. The decision for EEG was completely up to the treating medical team.
2.2 EEG variables
EEG was obtained using a 24 channel bedside NeuroCompact Portable EEG System (©Medicaid Systems). EEG electrodes were placed according to the 10/20 placement system. High and low pass filters were set at 0.5–1 Hz and 70 Hz respectively. Notch filter was set at 50 Hz and impedance at 75 Ohms. Recording was done for 30 min at the bedside and electronically recorded.
Formal reporting was done by a single neurologist using the Salzburg criteria. He was provided with brief clinical details of the patients during the management of the patient in the ICU as per the institutional practice. Patients who had undergone multiple EEG recordings during the same admission were included just once. All EEG findings following the first one for each of these patients were excluded as duplicates.
2.3 Statistical analysis
Descriptive analyses were performed on baseline characteristics and reported in terms of means with standard deviations, medians with interquartile ranges or frequency with percentages as appropriate. Six entries in which the EEG were normal were excluded from outcome analyses. Chi square test was done for the association of variables with outcome analyses in terms of discharge from the ICU or mortality. The values were expressed in terms of odds ratio with 95% confidence intervals (CI). A P value of 0.05 was set for the level of significance.
For the 43 entries with NCSE, STESS was calculated. Summary of this score is presented in Table 1. Further outcome analysis for these patients was done with respect to discharge from ICU or mortality. Individual STESS and outcomes were expressed in terms of proportions.
| SN | Parameter | Features | STESS |
|---|---|---|---|
| 1. | Consciousness | Alert or somnolent/confused | 0 |
| Stuporous or comatose | 1 | ||
| 2. | Worst seizure type | Simple-partial, complex-partial, absence, myoclonic | 0 |
| Generalized-convulsive | 1 | ||
| Non-convulsive status epilepticus in coma | 2 | ||
| 3. | Age | <65 years | 0 |
| ≥65 years | 2 | ||
| 4. | History of previous seizures | Yes | 0 |
| No or unknown | 1 | ||
| Total | 0–6 | ||
- Note: Adapted from Rosetti et al.9
All analyses were done using IBM SPSS Statistics for windows, Version 19.0. Armonk, NY: IBM Corp.
3 RESULTS
Among the 2234 admissions during the study period, a total of 178 EEG examinations were obtained. Eight patient entries were excluded from these as duplicate recordings obtained during the same ICU admission.
3.1 Baseline characteristics
The baseline characteristics of the included patients are shown in Table 2. The mean age of the patients was 59.1 years. A total of 51 out of 170 (i.e., 30%) patients were under mechanical ventilation. Majority that is, 164 (96.5%) of the patients had some abnormality while 6 (3.5%) had normal EEG recordings noted during the 30-min examination. These patients were excluded from further analyses of the outcomes. As evident in the Table 3, 73 (42.9%) patients had seizure activity of which more than half, 43 (58.9%) patients were in NCSE. Besides seizures, other abnormalities like diffuse slowing and burst suppression patterns were present in 91 patients (53.6%) of the patients.
| Characteristic | |
|---|---|
| Mean age | 59.1 years |
| Sex | N (%) |
| Female | 66 (38.8) |
| Male | 104 (61.2) |
| Age group | |
| <65 years | 93 (54.7) |
| ≥65 years | 77 (45.3) |
| Mechanical ventilation | 51 (30) |
| LOS ICU | |
| Mean ± SD = 5.7 ± 5.1, Range 1–36 days | |
| Outcome | |
| Discharge | 109 (64.1) |
| Expire | 44 (25.9) |
| LAMA | 17 (10) |
| Total | 170 |
| EEG finding | |
|---|---|
| Normal | 6 (3.5) |
| NCSE | 49 (28.8) |
| NCS | 24 (14.1) |
| Others | 91 (53.6) |
Table 4 divides patients into various categories based on the primary admitting diagnosis presumed to be cause for neurological dysfunction. These were grouped into two broad categories. More than half 58.8% had non-neurological diagnoses, labeled as “Metabolic.” All surgical (except neurosurgical) cases and all medical diagnosis besides the specific categories (including community acquired pneumonia, heart failure, tuberculosis, systemic lupus erythromatosis with septic shock, dengue shock syndrome etc.) were grouped together as “Others.” This group was the largest group with neurological dysfunction comprising of 18.8% patients.
| SN | Category | N (%) | |
|---|---|---|---|
| Neurologic 70 (41.2) | 1 | Epilepsy | 16 (9.4) |
| 2 | Intracranial space occupying lesion | 2 (1.2) | |
| 3 | Meningoencephalitis | 26 (15.3) | |
| 4 | Stroke | 19 (11.2) | |
| 5 | Traumatic brain injury | 7 (4.1) | |
| Metabolic 100 (58.8) | 6 | Hepatic | 23 (13.5) |
| 7 | Hyponatremia | 5 (2.9) | |
| 8 | Toxic | 17 (10) | |
| 9 | Uremia | 23 (13.5) | |
| 10 | Others | 32 (18.8) |
- Note: Others included all surgical (except neurosurgical) cases, community acquired pneumonia, heart failure, tuberculosis, systemic lupus erythromatosis with septic shock, dengue shock syndrome etc. Toxic included drug overdoses and poisoning (including organophosphorous poisoning and alcohol withdrawals).
3.2 Outcome analysis
Among the patients with abnormal EEG records after exclusion of those who had left against medical advice (LAMA) and hence the outcome was unknown, 43 (29.3%) patients had mortality. None of the variables examined in the study were found to have statistical significance for association with odds of mortality as shown in Table 5.
| Variable | Outcome | P value | OR | 95% CI | |
|---|---|---|---|---|---|
| Expired | Discharged | ||||
| Sex | |||||
| Female | 17 (29.8%) | 40 (70.2%) | 0.903 | 1 | |
| Male | 26 (28.9%) | 64 (71.1%) | 1.04 | (0.505–2.16) | |
| Age Group | |||||
| <65 years | 22 (26.5%) | 61 (73.5%) | 0.405 | 1.35 | (0.663–2.765) |
| ≥65 Years | 21 (32.8%) | 43 (67.2%) | 1 | ||
| Type of EEG abnormality | |||||
| NCSE | 11 (25.6%) | 32 (74.4%) | 0.733 | 1.22 | (0.532–2.822) |
| NCS | 8 (34.8%) | 15 (65.2%) | 0.78 | (0.296–2.107) | |
| Other | 24 (29.6%) | 57 (70.4%) | 1 | ||
| Diagnosis | |||||
| Metabolic | 30 (34.9%) | 56 (65.1%) | 0.07 | 1 | |
| Neurological | 13 (21.3%) | 48 (78.7%) | 1.98 | (0.928–4.214) | |
3.3 STESS
STESS was calculated for the 43 patients who had NCSE. A score of <3 was present in 3(7%) patients while 40(93%) patients had a score of ≥3. The frequency distribution of patients according to their STESS categories and their outcomes are shown in Table 6 and depicted graphically in Figure 1.
| STESS | ICU discharge | Mortality | Proportion of discharge (%) |
|---|---|---|---|
| 1 | 0 | 0 | 0 |
| 2 | 2 | 1 | 66.7 |
| 3 | 13 | 1 | 92.9 |
| 4 | 5 | 2 | 71.4 |
| 5 | 11 | 5 | 68.8 |
| 6 | 1 | 2 | 33.3 |
| Total | 32 | 11 | 43 |
4 DISCUSSION
This study shows utilization of EEG in only 170 patients among the 2234 patients who were admitted. This accounts for a mere 7.6% which is a very low utilization considering current evidences which point to higher rates of NCS/NCSE in critically ill patients. When considering only these patients who were clinically suspected of having any abnormality, a very high detection rate of 96.5% (164/170) was found. No exact criteria were present for obtaining an EEG and was based solely on clinical suspicion. No other study to the authors' knowledge has found such high rates of detection. However, the detection rates are found to be consistently on the rise in literature. Wang et al. have found the incidence to be >50% in patients in neuro-intensive ICU.17 This may suggest than detection rates may increase if obtaining an EEG is coupled with low GCS or clinical suspicion in high risk patients. This may be important in low resource setting where availability may be of concern.
Our study has also found the prevalence of any seizure activity and NCSE to be high (42.9% and 28.8%, respectively).1, 5, 18 NCSE was present in 58.9% of patients in whom any seizure activity was detected. The high prevalence of NCSE found in our study can be used to safely assume that their detection can be enhanced with the use of bedside EEGs. This is important since seizure activities have been found to self-propagate and cause irreversible neurological injury after a certain time.19-21 Furthermore, critically ill patients with multiple underlying pathologies have been found to have very shortened times after which neurological damage occurs.1, 14 Hence, this may be the reason why seizures have been found to have worse outcomes in this subgroup of patients. It is beyond the scope of this research to detect the long term neurological outcomes, nonetheless it can be safely said that diagnosis and timely treatment is of profound importance if the outcomes are to be improved.
Patients with underlying metabolic mechanisms for the altered sensorium, which was 58.5% (86/147) had half the odds of getting successfully discharged from the ICU than the ones with underlying neurological etiologies though statistically not significant (OR = 0.50, P = 0.07). Similar findings have been found in various studies.3, 9, 10 This could be in part because of the higher utilization of prophylactic anti-seizures drugs and higher index of clinical suspicion for seizures in patients with underlying neurological diseases. This further highlights the importance of early detection and management of non-convulsive seizures in non-neurological cases where the etiology may not be evident and diagnosis may be delayed.
For the 43 records with NCSE, STESS was calculated. This study did not have any patient with a STESS of 1, while only two patients had a score of 2. Though the study was found to be inadequately powered to assess the correlation between STESS and outcome, trends could be appreciated as depicted in Figure 1. Severe scores of ≥3 had decreasing odds of getting discharged from the hospital with increasing scores. This study helps to further validate the findings of Rossetti et al who had found similar results.9
From the unpublished hospital records during the same duration, the overall mortality rate was 12% compared to 29.3% among patients with abnormal EEG from this study. Again, this study was not powered enough to compare the mortalities, but the difference of 17% seems too high to be not mentioned here. Numerous other studies have found statistically significant mortality differences with poor outcomes in patients with NCSE.9, 14
4.1 Limitations
This study has several limitations. First, being a retrospective study, the decision of obtaining an EEG was not under the control of the study design. There could have been more patients in whom EEG could have been warranted but not obtained. The low utilization in our knowledge is in part due to financial factors of the patients' caregivers and unavailability during public holidays and off office hours. The interesting finding though, is the very high incidence of EEG abnormalities in whom it was performed.
Second, since this was a retrospective record based study, we could not ascertain the number of patients who had an indication for EEG but was not done due to reasons like open scalp injuries, dressings, artifacts, or others.
Third, patients with non-neurological diagnoses accounted for almost 60% of the total patients. The cause of NCS/NCSE in these patients could be related to the severity of the patients' illnesses. In addition to this, many patients were on prophylactic or therapeutic antiepileptics especially neurosurgical patients. Both of these factors, severity of illness and use of anti-epileptic drugs could not be captured in this study due to limited data availability owing to the design of the study. This could have very well affected the prevalence and association with outcomes.
Fourth factor which has negatively impacted the results of this study is the high rate of LAMA patients. Outcome could not be traced for 10% (17/170) of the patients, six of whom had NCSE. These patients were excluded from outcome analyses since it was not unknown. Inclusion of data from these patients could have changed some of the results significantly.
Despite these limitations, we believe that the findings are significant enough to advocate for provision of regular EEG facilities in all critical care units. Though continuous EEG monitoring is what should be aimed for, even a 30-min EEG coupled with a strong clinical index of suspicion can be useful especially where cost and availability can be very strong limiting factors in a resource limited setting like ours.
5 CONCLUSION
The findings of our study represent that of a mixed medical surgical ICU in a low middle income country. Though the utilization rate is very low, we have found very high rates of EEG abnormalities and NCS/NCSE, most probably due to inclusion of only patients with strong clinical suspicion. In addition, definite trend towards worse outcomes in terms of successful ICU discharge has been seen in his study with the presence of NCSE. Hence, coupled with strong clinical suspicion, increased utilization of EEG could be a step ahead in improving outcomes in critically ill patients.
ACKNOWLEDGMENTS
The authors would like to extend their gratitude to Mr. Jahirul Hussein, MPH and Mr. Santosh Chalise for their valuable support during the conduction of this study. This study had received a research grant from Nepal Academy of Science and Technology (Research Grant FY-2077/78).
CONFLICT OF INTEREST STATEMENT
None. We confirm that we have read the Journal's position on issue's involved in ethical publication and affirm that this report is consistent with those guidelines.