Epilepsy and neurocysticercosis in rural areas of the Bolivian Chaco: What has changed during the last 30 years?
Funding Information
Financial support for this work was provided by Sanofi's Access to Medicines Department. Sanofi has not been involved in the study design, data collection, analysis, or interpretation.
Abstract
Objective
Neurocysticercosis (NCC) is considered the major cause of epilepsy in endemic regions. In the rural areas of the Bolivian Chaco prevalence of NCC among people with epilepsy (PWE) was 27.4%, according to a population-based survey carried out in 1994. The aim of the study was to estimate the prevalence of Epilepsy Associated with Tonic–Clonic Seizures (EATCS) and to evaluate the prevalence of NCC among PWE in the rural communities of the Bolivian Chaco after 30 years.
Methods
Twenty-two rural communities (total population 12 852) were involved in the study. PWE in the study area were ascertained by multiple sources and the diagnosis was confirmed by a neurologist. All PWE identified were invited to undergo brain CT scan examination and diagnosis of NCC was sought according to the revised Del Brutto criteria.
Results
Seventy-eight PWE (30 men, 38.4%; mean age at onset was 12.7 ± 13.2 years) with EATCS were identified giving a crude prevalence of 6.1/1000 (95% CI: 4.7–7.3). Due to the COVID-19 lockdown, the study was interrupted in 2020 and only 36 PWE (46%) of the whole sample underwent CT scan examination. Of these, 8 (22.2%) fulfilled the criteria for NCC of whom 6 (75%) presented only single or multiple calcifications.
Significance
This is the first study reassessing the prevalence of NCC among PWE after 30 years, in the same rural area and using a population-based design. T. solium is still endemic in the Bolivian Chaco where more than 20% of EATCS may be attributable to NCC. Our findings show a substantially unchanged prevalence of NCC over the past 30 years despite improved knowledge, underlining the need for active intervention programs to control T. solium transmission in this area.
Plain Language Summary
Neurocysticercosis is still endemic in the Bolivian Chaco. The proportion of epilepsy attributable to neurocysticercosis is about 22%. Systematic efforts towards elimination of neurocysticercosis in these areas should be implemented.
Key Points
- In the Bolivian Gran Chaco epilepsy treatment gap is 25% when considering active epilepsy.
- Neurocysticercosis is still endemic in the Bolivian Chaco and about 22% of epilepsy cases in this region may be attributable to it.
- The actual proportion of epilepsy attributable to neurocysticercosis is close to that reported almost 30 years ago.
- Cysticercosis continues to be a neglected disease. Systematic efforts toward its elimination through active intervention should be enacted.
1 INTRODUCTION
Epilepsy is one of the most common neurological diseases, that affects more than 65 million people worldwide and accounting for an estimated 0.7% of the global burden of diseases.1 More than 80% of people with epilepsy (PWE) live in low-and middle-income countries (LMIC), where the disease remains largely untreated.2
In the Chaco region, Plurinational State of Bolivia, the estimated prevalence of lifetime epilepsy was 12.3/1000 (11.1/1000 for active epilepsy)3 and 7.2/1000 for Epilepsy Associated with Tonic–Clonic Seizures (EATCS) (6.6/1000 for active EATCS).4 During our long-lasting activity in the rural areas of the Bolivian Chaco we performed several epidemiological surveys, training programs directed to GPs, nurses, and Community Health Workers (CHWs) working in the rural communities of the Chaco region as well as community awareness programs, mainly directed to the detection and management of EATCS.5-13
Cysticercosis is considered a major public health problem, especially in LMIC, representing the most common helminthic infection of the nervous system in humans. In the usual life cycle of T. solium, humans acquire intestinal taeniasis by ingesting poorly cooked pork containing the parasitic cystic larvae or cysticerci. Once the adult tapeworm develops in the human small intestine, its microscopic eggs are shed with the stools of the tapeworm carrier. In places with poor sanitation and domestic pig raising, pigs ingest human stools and get infected with cysticercosis. Humans can also acquire cysticercosis by fecal-oral contamination from a tapeworm carrier in their intestine.14 In endemic regions, including Latin American Countries (LAC), neurocysticercosis (NCC), caused by infection of the central nervous system with the larval stage of T. solium, is a frequent cause of neurological morbidity.14 Although the clinical manifestations are extremely variable, parenchymal NCC accounts for about 30% of all epilepsy cases in endemic regions, therefore, representing the most important cause of acquired epilepsy worldwide.15
Prevalence of NCC among PWE was evaluated in a previous survey carried out in 1994 in the rural areas of the Bolivian Chaco. In particular, in this population-based survey, 27.4% of PWE fulfilled the Del Brutto diagnostic criteria16 for definitive or probable NCC.17 The aim of the present survey was to evaluate the prevalence of EATCS and the frequency of NCC among PWE in the rural communities of the Bolivian Chaco 30 years after the previous survey.
2 MATERIALS AND METHODS
2.1 Study area and study population
The Plurinational State of Bolivia is a low-income country where almost 4 million people live under the “poverty line”, especially in rural areas, and where access to the health system is still difficult.18
The southeast region of Bolivia is part of the “Gran Chaco,” a subtropical area also including Argentina and Paraguay. The ethnic group living in the study area is mainly represented by native Guaraní people, living in poor dwellings located in rural communities often reachable only by rural roads, without running water or electricity, and with a local economy based on agriculture and animal husbandry. The study included 22 rural communities located in two municipalities (Gutierrez and Eiti) of the Cordillera province, Department of Santa Cruz, Bolivia, that are part of the Gran Chaco region, with a total population of 12 852 inhabitants, according to the 2018 census.
2.2 Case ascertainment
PWE in the study area were ascertained by multiple sources. The main source for the case ascertainment was the Community Epidemiology Program “EPICOM”. In particular, EPICOM program was promoted by the Centro de Epidemiologia Comunitaria y Medicina Tropical (CECOMET), a nonprofit Organization that aims to promote Health and wellbeing in tropical countries. According to this program, all the rural communities have been screened by trained CHWs trough an epidemiological survey focusing on child, reproductive and maternal health, infectious disease prevention, particularly Neglected Tropical Diseases, epilepsy, and hypertension.19 Furthermore, the following additional sources were also considered: PWE already known because previously identified by the CHWs and/or GPs working in the study areas who had already received a diagnosis of epilepsy or were already taking Anti-Seizures-Medication (ASM); PWE who were identified by previous neuroepidemiological surveys carried out by our group in the same areas.4, 7, 13 All PWE identified by the different sources were evaluated by a neurologist in order to confirm the diagnosis.
2.3 Epilepsy definition
According to the ILAE definition, epilepsy was clinically defined as a “condition characterized by recurrent (two or more) epileptic seizures, unprovoked by any immediate identified cause.”.20-22 We defined TC seizures as “episodes characterized by loss of consciousness lasting more than 1 minute, presence of tonic movements (such as generalized stiffening) and/or clonic movements (such as thrashing about) and at least one of the followings: (1) sphincter disturbance (i.e., loss of urine or stool during the fit); (2) muscle soreness after the fit; (3) fit injury (tongue biting, head cut); (4) froth coming out of the mouth; and (5) falling”.23
EATCS were classified as generalized TC or as focal onset with secondary generalization according to the simplified clinical classification of seizure type.22 We considered active EATCS people with at least one seizure within 2 years at the time of the enrollment, regardless of ASMs treatment.22 We defined people with lifetime EACS those having experienced at least two convulsive seizures in their life, before the prevalence day (30th June 2018).
2.4 CT scan examination
All PWE identified were invited to undergo brain CT scan. CT scans were performed in a private center located in Santa Cruz de la Sierra where a multislice computed tomography (CT) imaging was used. Patients who underwent CT scan were transported from their community to Santa Cruz by car. For safety reasons, intravenous contrast administration was not performed. In 2020, due to COVID-19 emergency safety measures, mobility was forbidden and CT scan examinations were interrupted. Consequently, not all PWE identified performed the CT scan examination.
2.5 Diagnosis of NCC
According to the revised version of the Del Brutto diagnostic criteria for NCC24 diagnosis of NCC was based on the presence of absolute criteria, neuroimaging criteria (major confirmatory and minor), and clinical/exposure criteria (major and minor). Diagnosis of definitive or probable NCC was sought accordingly.
2.6 Statistical analysis
Data were analyzed using STATA 15 software packages (version 15.0). Data cleaning was performed before the data analysis considering both range and consistency checks. Quantitative variables were described using mean and standard deviation (SD). The frequency comparisons were done with the chi-square test. In case of not normal distribution, appropriate nonparametric tests were performed. Prevalence was based on the number of patients living in the study area who fulfilled the diagnostic criteria on prevalence day (30th June 2018). Age- and sex-specific prevalence were estimated for both lifetime EATCS cases. Confidence intervals (CIs) for estimates were calculated assuming a Poisson distribution.
2.7 Ethics
The study had the approval of the Bolivian Neurological Society institutional review board (IRB). Informed consent was obtained from all the patients involved in the study.
3 RESULTS
3.1 Prevalence of epilepsy
Overall, 22 rural communities with a total population of 12 852 (6512 men, 50.7%) have been involved in the study. Distribution of the study population is shown in Figure 1. The mean population for each community was 643 ± 475, ranging from 48 to 1676 inhabitants.
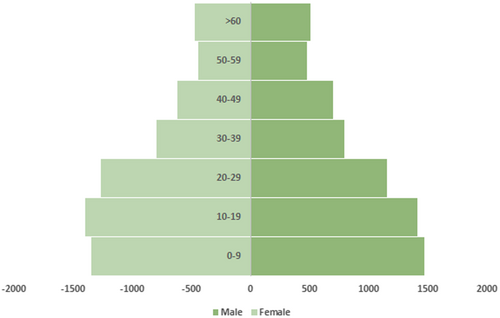
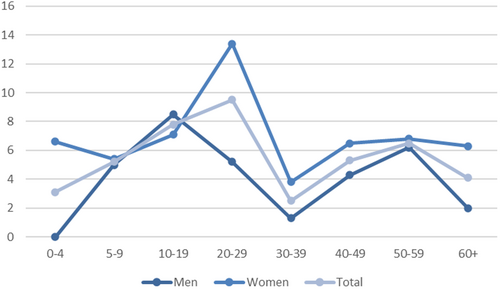
At the end of the screening, 87 subjects were identified. Of these, for 6 the diagnosis of epilepsy was not confirmed while 3 could not be traced. In the end, 78 PWE (30 men, 38.4%; mean age 25.4 ± 16.4 years; mean age at onset 12.7 ± 13.2 years, ranging from 0 to 59) with EATCS were identified giving a crude prevalence of 6.1/1000 (95% CI: 4.7–7.3). Prevalence rate among women was 7.6/1000 (95% CI: 5.6–9.7), while it was significantly lower among men 4.6/1000 (95% CI: 3.0–6.2) (P-value 0.02); age-specific prevalence showed a bimodal distribution with a first peak in the group aged 20–29 (9.5/1000) and a second in the group aged 50–59 (6.5/1000) as shown in Table 1 and Figure 2. Considering the seizures classification, out of the 78 subjects, 62 (84.9%) had TC seizures, 11 (15.1%) had focal with secondary generalization and 5 were unknown. Detailed clinical history was available for 55 PWE (70.5%), who were present in the communities during the survey, thus a direct interview was carried out. 14 (25.4%) out of 55 PWE did not have any seizures during the last 2 years and were considered with no active epilepsy. Out of the 41 PWE with active epilepsy (at least one seizure during the last 2 years), 31 (75.6%) were taking ASMs.
| Men | Women | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Population | Cases | Prevalence | Population | Cases | Prevalence | Population | Cases | Prevalence | |
| 0–4 | 665 | – | – | 608 | 4 | 6.6 | 1273 | 4 | 3.1 |
| 5–9 | 802 | 4 | 5.0 | 742 | 4 | 5.4 | 1544 | 8 | 5.2 |
| 10–19 | 1408 | 12 | 8.5 | 1398 | 10 | 7.1 | 2806 | 22 | 7.8 |
| 20–29 | 1157 | 6 | 5.2 | 1265 | 17 | 13.4 | 2422 | 23 | 9.5 |
| 30–39 | 794 | 1 | 1.3 | 794 | 3 | 3.8 | 1588 | 4 | 2.5 |
| 40–49 | 701 | 3 | 4.3 | 618 | 4 | 6.5 | 1319 | 7 | 5.3 |
| 50–59 | 481 | 3 | 6.2 | 441 | 3 | 6.8 | 922 | 6 | 6.5 |
| 60+ | 504 | 1 | 2.0 | 474 | 3 | 6.3 | 978 | 4 | 4.1 |
| Total | 6512 | 30 | 4.6 | 6340 | 48 | 7.6 | 12 852 | 78 | 6.1 |
3.2 Neurocysticercosis
Due to COVID-19 emergency safety measures, mobility was forbidden and CT scan examination were interrupted in 2020. Consequently, not all PWE identified during the screening performed the CT scan examination. Out of the 78 PWE, only 36 (46.1%) underwent a CT scan examination and one also MRI examination. Out of these 36 PWE, 8 (22.2%) fulfilled the revised diagnostic criteria24 for definitive or probable NCC. Seven out of 8 subjects were males with a mean age of 35.2 ± 21.7 years. In particular, 6 (75%) presented calcifications (one single and five multiple calcifications), while two were classified as viable cysts. Considering these two cases, one underwent MRI examination demonstrating a scolex within a cystic lesion (“hole-with-dot” imaging), thus fulfilling the absolute criteria; the other underwent just CT scan examination showing viable cysts along with calcified lesions. All NCC patients presented TC seizures (five focal with secondary generalization and two generalized tonic–clonic) and the majority were late-onset epilepsy with a mean age at onset of 22.5 ± 15.5 years. All patients received ASMs and four out of six PWE with calcified NCC have not had any seizure for at least 2 years. Clinical characteristics and NCC diagnostic certainty are reported in Table 2.
| Sex | Age onset | Age | Seizures | Active epilepsy | Neuroimaging | Absolute criteria | Major neuroimaging | Minor clin/exp | NCC | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 40 | 52 | FSG | No | Multiple calcifications | − | + | ++ | Probable |
| 2 | M | 5 | 6 | FSG | No | Multiple calcifications | − | + | ++ | Probable |
| 3 | M | 35 | 54 | FSG | Yes | Viable cysts + calcifications | − | + | ++ | Probable |
| 4 | F | 3 | 23 | FSG | Yes | Multiple calcifications | − | + | ++ | Probable |
| 5 | M | 30 | 65 | TC | Yes | Multiple viable cystsa | + | + | ++ | Definitive |
| 6 | M | 12 | 15 | TC | No | Multiple calcifications | − | + | ++ | Probable |
| 7 | M | 40 | 47 | TC | No | Multiple calcifications | − | + | ++ | Probable |
| 8 | M | 15 | 20 | FSG | Yes | Single calcification | − | + | ++ | Probable |
- Abbreviations: Clin/Exp, clinical/exposure criteria, FSG, focal with secondary generalization; TC, tonic–clonic.
- a MRI examination demonstrating a scolex within a cystic lesion.
4 DISCUSSION
Epilepsy is a global health issue affecting patients without distinction of age, race, and socioeconomic class. By 2016, it was estimated that 45.9 million patients were living with active epilepsy worldwide. This condition is twice as common in low- and middle-income countries as it is in the developed world25 and it has been estimated that 6.3 million people were living with active epilepsy in LAC.26
The main aim of the present survey was to reevaluate the prevalence of EATCS and frequency of NCC among PWE in the Bolivian Chaco, using a population-based study design, after around 30 years. Indeed, NCC is endemic in most of the world and it accounts for approximately 30% of cases of epilepsy in endemic areas.14 Our survey confirmed the high prevalence of EATCS (6.1/1000) in this rural area and also that, after almost 30 years, NCC still plays a central role accounting of more than 20% of cases.
4.1 Prevalence of EATCS
According to a previous epidemiological survey carried out by our group in 1994, lifetime prevalence of epilepsy in the rural areas of the Bolivian Chaco was 12.3./1000 and 11.1/1000 for active epilepsy,3 rates close to those reported in LAC in recent metanalyses.27, 28 However, as highlighted by the WHO,29, 30 in a rural setting the detection of EATCS by trained CHWs represents the main priority since TC seizures are associated with higher comorbidity, injury, and mortality than nonconvulsive epilepsy and are easier to recognize. Thus, in agreement with the WHO guideline,29, 30 during the last two decades, our activities in the rural area of the Bolivian Chaco have been focused just on EATCS.5, 6, 8, 9, 11-13
In particular, we carried out different epidemiological surveys3, 4, 7, 13 using rigorous methodological approaches based on two-stage or three-stage designs and validated screening instruments in order to detect PWE. In the present survey we used different sources for the case ascertainment and the main source was the Community Epidemiology Program “EPICOM”.19 In particular, EPICOM replicates a larger Community Epidemiology Program promoted by the Centro de Epidemiologia Comunitaria y Medicina Tropical (CECOMET) in a similar rural context in Ecuador. This latter program has been implemented in Ecuador over almost 40 years with the main purpose of demonstrating how bottom-up strategies should be developed and maintained, with program centered on the real needs of the communities with CHWs as principal actors. Indeed CHWs, in close collaboration with medical and nursing personnel, may assure effective care for different diseases including classical infectious conditions as well as chronic noncommunicable diseases such as epilepsy.19 The Community Epidemiology Program underlines the critical importance of a direct participation of community members to assure effective health care in peripheral areas of LMIC. Although in our survey we did not apply a formal epidemiological study design (e.g., two- or three-stage designs), it should be noted that the prevalence obtained is close to those obtained in other recent surveys4, 13 carried out by our research group in the Chaco region. In particular, in a large survey involving a population of about 19 000 inhabitants and using a three-stage design, we found a lifetime prevalence of EATCS of 7.2/1000.4 Close results were also reported in a more recent survey carried out in the Isozo area of the Cordillera Province in which a similar three-stage design was adopted and where the prevalence of EATCS was 5.8/1000.13 Furthermore, it should be noted that the distribution of the age-specific prevalence reported in the present study is close to those reported in the previous studies, showing a bimodal distribution with a first peak in the group aged 20–29 years and a second in the group aged 50–59 years. On the bases of these evidences, even if a different methodological approach was used, the accuracy of the estimated prevalence sounds to be suitable. At any rate, it should be underlined that the different activities carried out by our group over the time5, 6, 8, 9, 11-13 have increased the level of knowledge and awareness about epilepsy in this region, thus leading to an increased chance for PWE to be identified and treated. Indeed, almost all PWE identified during the survey were already known and regularly followed up, as also demonstrated by the low TG recorded. As a matter of fact, the TG was only 25% when considering PWE with active epilepsy. Concerning the type of seizures almost all PWE presented epilepsy with TC seizures, in agreement with the activities carried out by our group that, as reported, were mainly directed toward EATCS in agreement with the WHO recommendations.29, 30
4.2 Neurocysticercosis
Taenia solium taeniasis/cysticercosis is endemic in Central and South America, sub-Saharan Africa, Indian Ocean, and large regions of Asia14 and in these regions, the infection is a frequent cause of neurological morbidity. The variable number, stage, and localization of the infecting parasites, added to the inflammatory response of the host, configure a wide array of possible symptoms that include most neurological manifestations. Among these, the most frequent are seizures in parenchymal NCC and headache and intracranial hypertension in extraparenchymal NCC (ventricles or subarachnoid spaces). Seizures in NCC result from a focal lesion associated with inflammation and tissue alterations, but seizures may persist for years also after the parasite has calcified. In endemic regions NCC is the most frequent cause of acquired seizures and epilepsy, accounting for 30% of seizure disorders.14
According to the revised Del Brutto criteria, prevalence of NCC in this population-based cohort of PWE was 22.2%, but the majority of patients (75%) presented only single or multiple calcifications. In agreement with literature data, the majority presented late-onset focal seizures with secondary generalizations.14, 17 This rate is slightly lower than the proportion reported in a previous survey carried out in 199417 in which, according to the Del Brutto criteria proposed in 2001,16 prevalence of NCC among PWE was 27.3%. Furthermore, a slightly higher proportion of calcified NCC was observed (75% vs 58%).17
4.3 Limitations
We are aware that several limits should be considered in interpreting our results. First, due to the COVID-19 lockdown, the study was interrupted in 2020 and only 46% of the whole sample was able to perform the CT scan. Furthermore, as in the previous survey, due to safety reasons, CT scan was performed without contrast injection, thus it is possible that some cases were not identified, leading to an underestimation. Finally, due to COVID restrictions limiting healthcare activities outside emergency services, also serological assay analysis was not performed. Nonetheless, it should be noted that the revised Del Brutto criteria are largely centered on neuroimaging and the diagnosis can be sought also in absence of serological assay, if one major neuroimaging criteria and two minor clinical/exposure criteria, such as in our case, are present.24 However, due to the lack of the serological assessment, for the majority of subjects we were not able to achieve a diagnosis of definitive NCC, thus the level of certainty was only probable. At any rate, regardless of the possible limitations, is should be noted that the prevalence reported in our sample is close to that expected on the basis of literature evidence27 as well as to the prevalence reported in our previous survey.17 Indeed, according to a recent meta-analysis in LAC the proportion of NCC diagnosis among people living with epilepsy was 17.4.27 Considering the clinical characteristics, in agreement with literature, almost all cases presented adult-onset focal seizures with secondary generalization. Furthermore, 75% were calcified NCC and among these six cases, four were classified as not active epilepsy.
To the best of our knowledge, this is the first study reassessing the prevalence of NCC among PWE after 30 years, in the same rural area and using a population-based design. While taking into consideration all the possible limits, mainly related to the COVID-19 lockdown, our survey demonstrated that NCC is still endemic in the Bolivian Chaco and that about 22% of epilepsy cases in this region may be attributable to NCC, a proportion close to that reported almost 30 years ago. As well known, endemicity of T. solium require the coexistence of domestic pig raising and poor sanitary conditions and the development and urbanization result in the disappearance of these conditions. However, sustained poor living conditions and domestic pig raising are the norm in most developing countries where development may take decades or even never occur. In these settings, active intervention programs to eliminate or to control T. solium transmission must be planned. As a matter of fact, a decrease in transmission and morbidity was reported in Salama, Honduras following a sustained health education and control program,31 and more recently, a large elimination program demonstrated elimination of transmission by using a combination of human and porcine mass chemotherapy, pig vaccines, and stool coproantigen case confirmation.32 However, cysticercosis continues to be a neglected disease and no systematic efforts toward its elimination through active intervention have been enacted anywhere.14
AUTHOR CONTRIBUTIONS
Alessandra Nicoletti conceived and designed the study, collected and analyzed data, and wrote the first draft of the manuscript; Calogero Edoardo Cicero, Valeria Todaro, and Chiara Colli collected and analyzed data; Estela Vilte, Elizabeth Blanca Crespo Gomez collected data; Francesco Cosmi, Mariella Anselmi, Cintia Caicedo, Walter Mario Camargo, Alessandro Bartoloni critically revised the article, Loretta Giuliano conceived and designed the study, collected and analyzed data and critically revised the article; all authors read and approved the final draft of the manuscript.
ACKNOWLEDGMENTS
We are grateful to Father Tarcisio Dino Ciabatti, coordinator of the agreement between the Ministerio de Salud y Deportes and the Vicariato Apostólico de Camiri, for his encouragement and cooperation; to Francesco Cosmi and the other workers of “Convenio de Salud” of Camiri for their support and invaluable help; and the local health authorities and the Asamblea del Pueblo Guaraní for their encouragement and cooperation.
CONFLICT OF INTEREST STATEMENT
None of the authors has any conflicts of interest to disclose.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.