Seizure-related injuries in people with epilepsy: A cohort study from Saudi Arabia
Abstract
Objectives
Patients with epilepsy have a high risk of accidents and injuries, resulting in minimized physical activity and social withdrawal. Therefore, we surveyed the prevalence and the types of injuries that patients with epilepsy may endure, and the factors that may increase the risk of injuries.
Methods
In this cohort study, adult and pediatric patients diagnosed with epilepsy (age ≥ 7 years) and a close family member (parents/guardian) attending the outpatient epilepsy clinics at King Fahd Medical City (Riyadh, Saudi Arabia) were interviewed by neurologists. They reviewed the patients' medical records and administered a structured questionnaire to identify and compare several variables, including injury frequency versus seizure type and seizure frequency, number of antiseizure medications used, medication compliance, and work and social limitations.
Results
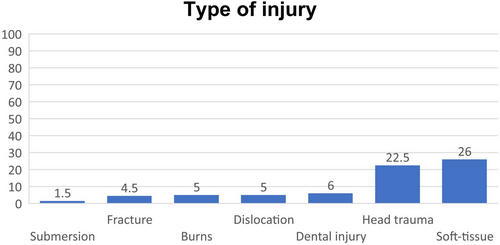
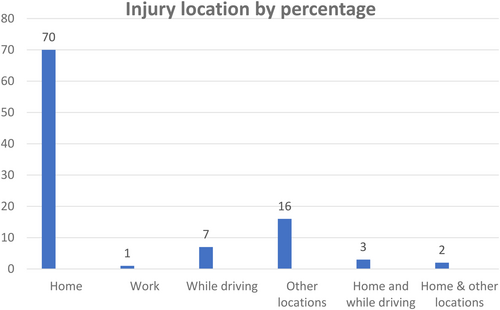
Out of 200 patients, 86 (43%) sustained injuries during an attack of their habitual seizures. Almost half of this group showed a tendency for recurrent injuries. The most common traumas were soft tissue injury (36.5%), head injury (32%), dental injury (8.5%), burns (7%), dislocation (7%), fractures (6.5%), and submersion (2%). Two-thirds of the patients had their injury at home. 64% of patients who had seizures for more than 10 years sustained multiple injuries (P = .003). Injury frequency was higher among patients with daily or monthly seizures (P = .03). 76% of patients who suffered injuries more than twice had generalised tonic-clonic seizures, and genetic generalised epilepsy was encountered more in injured patients (P = .02). Also, patients on polytherapy were more likely than those on monotherapy to have an injury (P = .003).
Significance
Two-fifths of the patients reported seizure-related injuries. The most common were soft-tissue injuries and head traumas, while homes were the most frequent site. In addition, longer epilepsy duration, generalized tonic-clonic seizures, and polytherapy were associated with a higher prevalence of injuries. Therefore, injury prevention strategies should be developed for PWE, especially for those at higher risk.
Key points
- We studied the injury type/frequency in adult and pediatric patients with epilepsy.
- Soft-tissue and head injuries were the most common in patients with epilepsy.
- Most injuries were domestic, and their frequency increased with epilepsy duration.
- Social withdrawal was common in patients with frequent convulsions and traumas.
- Injuries occurred more in patients on multiple anti-seizure medications and with a generalized type of convulsion.
- There is a relationship between injury risk and more frequent seizures, where daily, weekly, and monthly seizures correlated with a higher frequency of injuries than less frequent seizures.
1 INTRODUCTION
Epilepsy is a chronic disorder and one of the most common neurological diseases that affects approximately 50 million people worldwide.1 The prevalence of epilepsy in Saudi Arabia is 6.54 per 1000, which is similar to the prevalence described in most other societies.2 Patients with epilepsy are physically, mentally, emotionally, and socially affected.3-5
Epilepsy-related accidents cause approximately 5% of patients with epilepsy to visit the emergency department annually.6-8 Moreover, patients with epilepsy presumably have a high risk of accidents and injuries at home, at work, or while driving, which subsequently causes these patients to minimize physical activity and withdraw socially. Thus, seizure-related injuries extend beyond people with epilepsy (PWE) to affect their families, employers, and coworkers.9 The main risk is the transient loss of awareness and abnormal tone during convulsions or interictal epileptiform discharges.10 Moreover, these patients are prone to accidents because of multiple factors such as inadequate control of seizures, unfavorable reactions, sedative effects of antiseizure medications, and associated physical disabilities.11 Related comorbidities such as learning difficulties, depression, and other neuropsychiatric disorders are also frequent in patients with epilepsy and may increase the risk of seizure-related accidents.12
Most research worldwide has focused on the clinical and psychosocial burden of epilepsy with less of a focus on epilepsy accidents and injuries. The epidemiological data on the prevalence of seizure-related injuries have also been conflicting and diverse. Thus, the estimated prevalence of seizure-related injuries among PWE ranges between 0.6% and 47.3%.10, 13, 14
In Saudi Arabia, the impact of epilepsy on physical injury is unknown. Therefore, this study investigated the types of injuries sustained by adult and pediatric patients with epilepsy, the factors that increased the risk of injuries, and the clinical outcomes and limitations encountered by trauma. The aim is to improve the understanding of this population's actual risks and challenges and identify the means to improve the patient and family counseling effectiveness.
1.1 Study design and participants
This cohort study was conducted at King Fahd Medical City (Riyadh, Saudi Arabia) among patients with epilepsy between December 2020 and September 2021. In this study, we included 200 patients with epilepsy. The inclusion criteria were 7 years or older, a diagnosis of epilepsy, and the participant was a patient of the pediatric and adult epilepsy outpatient clinics at King Fahd Medical City. After the patients or their guardians/parents agreed to participate in this study, they were asked about seizure-related injuries that occurred 12 months prior to the last seizure.
1.2 Materials and methods
The Institutional Review Board approved our institute to survey the patients attending the outpatient epilepsy clinics after obtaining their informed consent, as the Institutional Ethical Committee required. Then, the data were collected by interviewing participants using a structured questionnaire and reviewing patient charts. The patients and accompanying relatives were interviewed using a questionnaire that gathered the following information: type, duration, and frequency of seizures; the number of antiseizure medications used; and medication compliance. In order to assess the physical injuries among patients with epilepsy, a developed semi-structured questionnaire from the literature review was used in this study.13-15 The responses on the questionnaire were the patients' self-reports, or responses by the patients' parents/guardians, of physical injuries that may have occurred in the previous 12 months prior to the last seizure that they believed were seizure related. They answered questions with “yes,” “no,” or “I do not know.” The questionnaire was used to determine five aspects of seizures: type of seizure-related injury, seizure frequency, the location where the injury occurred, outcomes of the injury, and seizure-related limitations. The type of injury was determined by using predefined options, which included eight types of injuries such as burns (including its location and cause), submersion, dislocations (including which joints), fracture (including which bone), head injury, soft-tissue injury, dental injury, and car accidents. This study defined seizure-related physical injury as one or more reported injuries such as abrasion, burn, dental injury, fracture and head injury, and dislocation. The frequency of injuries was assessed by asking the patients about the overall frequency of injuries during the previous 12 months with the options of “none,” “once,” “twice,” “three times or more,” and “unknown.”
Moreover, we asked the patients about the location where an injury occurred, such as home, work, driving, or other locations. The injury outcomes were assessed by asking the patients whether their injury required hospitalization, if an injury caused lifelong or short-term loss of functions, and whether this injury caused the patients to be absent from school or work. Finally, we assessed seizure-related limitations among the patients by asking them about their ability to drive and whether they had work or social limitations. The answers ranged from “not bothered” to “extremely bothered.”
1.3 Statistical analysis
This study compared several variables: the frequency of injuries to the type and frequency of seizures, number of antiseizure medications used, medication compliance, and work and social limitations. The data were analyzed using statistical analysis software R (developed by Ross Ihaka and Robert Gentleman in 1993; R Foundation in Vienna, Austria) and Minitab (developed by Barbara F. Ryan, Thomas A. Ryan Jr., and Brian L. Joiner in 1972 at the Pennsylvania State University, State College, PA, USA). The Pearson chi-square P-value with a 95% confidence level was used to determine the significance level of the variables.
2 RESULTS
2.1 Patients' characteristics
Two-hundred patients with epilepsy were enrolled in this study. The mean age was 23 years (standard deviation [SD], 14.3 years; range, 7-60 years), 51% of patients were 19-40 years old, and 25% were 13-18 years old. Moreover, 54.5% of patients were males, and 45.5% were females. Furthermore, 139 (70%) patients were adults, and 61 (30%) patients were children. Forty-six percent of the patients were single, and 20% were married. Thirty-one percent of the sample were children. With regard to the educational level of the participants, 27% had graduated from high school, and 26% had a bachelor's degree. The etiology of epilepsy was as follows: 33% of patients had symptomatic epilepsy (11.5%, injured group; 21.5%, noninjured group), 36.5% of patients had genetic generalized epilepsy (19.5%, injured; 17%, noninjured), and 30.5% of patients had seizures of unknown etiology (12%, injured; 18.5%, noninjured) (Table 1). The duration of epilepsy was <1 year in 5% of patients, 1-5 years in 34% of patients, 6-10 years in 28% of patients, and >10 years in 34% of patients. The frequency of seizures during the previous year was monthly in 33% of patients and daily in 17% of patients; however, 26% were seizure-free during the last year.
| Epilepsy etiology | Injured count | Noninjured count | P value |
|---|---|---|---|
| Genetic | 39 | 34 | .02* |
| Unknown | 24 | 37 | .48 |
| Other | |||
| Structural | 23 | 43 | .1 |
| Immune | |||
| Infection | |||
| Metabolic | |||
| Seizure type | |||
| Tonic–clonic seizures (generalized-onset or focal to bilateral) | 49 | 39 | .001* |
| Myoclonic seizure | 4 | 5 | .92 |
| Absence | 0 | 3 | .45 |
| Atonic | 3 | 2 | .43 |
| Focal impaired awareness | 24 | 47 | .05 |
| Focal aware | 5 | 14 | .12 |
| Other | 1 | 4 | .29 |
| No. of ASMs | |||
| Monotherapy | 24 | 55 | .0036* |
| Polytherapy | 62 | 59 | |
- *Statistical significance.
- Abbreviation: ASMs, antiseizure medications.
Based on the seizure classification, 105 (53%) patients had generalized seizures; of these patients, 44% had generalized tonic–clonic or focal to bilateral tonic–clonic seizures, 5% had myoclonic seizures, 2.5% had atonic seizures, and 1.5% had typical absence seizures. However, 90 (46%) patients had focal seizures (36%, focal impaired awareness seizures; 10%, focal aware seizures). About antiseizure drug use, 79 (39.5%) patients were on monotherapy (32%, injured; 48%, noninjured) and 121 (60.5%) patients were on two or more medications (72%, injured; 52%, noninjured) (Table 1).
2.2 Injury prevalence and types
Among 200 patients, 86 (43%) patients sustained injuries during an attack of their habitual seizures: 18 (21%) patients were children and 68 (79%) patients were adults. In addition, 44 (51%) patients (43% adult and 8% pediatric patients) sustained an injury at least once; 11 (13%) patients (7% adult; 6% pediatric patients) sustained an injury two times; and 31 (36%) patients (29%, adult; 7%, pediatric patients) sustained an injury three times or more (Figure 1).
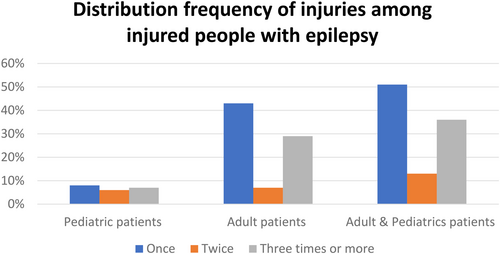
The most common traumas were soft-tissue injury (36.5%) and head injury (32%). Other injury types were dental injuries (8.5% of patients), burns (7%), and dislocation (7%). Moreover, 6.5% of patients experienced fractures, and 2% of patients experienced submersion. Among the adult patients, 43% responded that they drive, and 8% responded that they were involved in traffic accidents (Figure 2). Most patients (70%) had accidents at home (i.e., domestic trauma), whereas 16% had accidents in other locations such as streets, school, or work, and 7% had accidents while driving (Figure 3).
2.3 Factors associated with physical injury
- The injury frequency was low among patients who had seizures for <1 year (P < .001): 78% of these patients did not sustain any injury. However, 64% of patients who had seizures for >10 years reported sustaining multiple injuries (P = .003).
- Seizure frequency was monthly in 33% of patients (38%, injured; 46%, noninjured), weekly in 13% of patients (13%, injured; 20%, noninjured), and daily in 17% of patients (23%, injured; 20%, noninjured). However, 26% of patients (19% injured; 46% noninjured) had not experienced seizures for >1 year. Injury frequency was higher among patients with daily and monthly convulsions than those with annual seizures or who were seizure-free for >1 year (P = .03).
- We also found that 76% of patients who sustained injuries more than twice had generalized tonic–clonic seizures or focal to bilateral tonic–clonic seizures, whereas 27% of patients who sustained an injury only once had focal impaired awareness seizures.
- Using chi-square analysis, 56%-60% of patients with generalized tonic–clonic seizures or focal to bilateral tonic–clonic seizures sustained injuries (P < .001). However, 74% of patients who had focal aware seizures did not sustain any injury. Most (44%) surveyed patients denied experiencing an aura before their seizures, whereas a smaller proportion (26%) always sensed a warning in advance. We could not find an association between aura and trauma or between aura and a higher incidence of injuries.
- A chi-square test of independence was performed to examine the relation between injury and the number of antiseizure medications. Sixty-nine percent of patients on a single medication did not sustain any injuries, whereas 51% of patients on polytherapy sustained injuries. The relation between these variables was significant (P = .0036). The patients on polytherapy were more likely than those on monotherapy to have an injury. However, the patients on polytherapy experienced more daily and monthly seizures (P = .04), which could be the reason for the increased tendency to have injuries in this group (Table 2).
- Moreover, medication compliance was not correlated with injury frequency. Eighty-four percent of patients strictly adhered to antiseizure medications, whereas 11% missed some doses and 3% had poor adherence.
- Moreover, our data revealed that 81.5% of male patients had at least one injury, whereas 93.8% of female patients had injuries. No relationship existed between injury versus no injury and sex (P = .395) or between injury frequency and sex (P = .54).
- The results indicated that genetic generalized epilepsy is more common in patients with seizure-related injury than in noninjured groups (P = .02) (Table 1).
- Fifty percent of injuries were reported by patients 19-40 years old, whereas 24% of injuries were reported in children <12 years old.
| No. of ASMs | Injured | Noninjured | Sz frequency | Injured | Noninjured | P-value |
|---|---|---|---|---|---|---|
| Monotherapy | 24 | 55 | Daily | 2 | 5 | .91 |
| Weekly | 1 | 5 | .44 | |||
| Monthly | 7 | 18 | .75 | |||
| Annually | 6 | 3 | .01 | |||
| Seizure-free for more than a year | 10 | 22 | .88 | |||
| Two or more drugs (polytherapy) | 62 | 59 | Daily | 19 | 9 | .04* |
| Weekly | 10 | 8 | .69 | |||
| Monthly | 25 | 13 | .03* | |||
| Annually | 4 | 13 | .01* | |||
| Seizure-free for more than a year | 6 | 14 | .03* |
- *Significant value.
- Abbreviation: ASMs, antiseizure medications.
2.4 Counseling of patients with epilepsy
Seizure triggers such as poor compliance with antiseizure medications, sleep deprivation, and stress are part of the counseling process for patients with epilepsy during regular outpatient visits. The patients and their attending family members were asked whether they were counseled in previous clinic visits to the epilepsy clinic. Seventy-six percent of patients had received counseling about various aspects of seizures, including medication compliance, stress, and fatigue. In addition, 23% of patients were counseled about epilepsy precautions such as avoiding taking baths and taking showers instead, avoiding driving unless the patient is seizure-free for at least 6 months, and avoiding using sharp objects such as knives.
3 DISCUSSION
In this study, we surveyed the injuries that adult and pediatric patients with epilepsy may endure, the factors that may increase the risk of injuries, the clinical outcomes, and the limitations the patients may encounter because of traumas. We found the most common injuries were soft-tissue injuries and head trauma. Most injuries occurred at home; injury frequency increased with increasing duration of epilepsy; risk of injury was associated with the number of antiseizure medications used, generalized tonic–clonic seizures, and focal to bilateral tonic–clonic seizures; and social withdrawal was common among patients with frequent convulsions and injury.
In the past several years, many studies have investigated and analyzed the risk of injury among patients with epilepsy and have categorized these accidents as “fatal” or “nonfatal.” Examples of nonfatal accidents are fractures, abrasions, mild-to-moderate contusions, and minor burns.16-22 Epilepsy-related accidents cause approximately 5% of patients with epilepsy to visit the emergency department annually.8 A widely known fact is that PWE are at increased risk for accidental injury compared to the general population. In contrast, conflicting reports exist in the literature, and some reports have shown a similar risk of injury. The contradictory results are because of several factors such as population type used in the study, the definition of epilepsy used in the study, the accuracy of injury reporting, study design, and length of the observation period.
The injury data were based on the patients' recall of injuries sustained in the previous 12 months. Our data revealed that 44% of interviewed patients had suffered injuries: 10% were children and 34% were adults. In 2002, a European cohort study15 showed that nearly one-fourth of patients with epilepsy experienced traumas secondary to seizures and that the most common accidents were contusions and wounds. Other injuries included sprains, burns, fractures, abrasions, and brain contusions, but only 3% of patients required hospital admission.15 Our study showed that the most common injuries in the adult and pediatric populations were soft-tissue injuries such as contusions and lacerations (36.5%). Moreover, head injuries were one of the most documented accidents, with an incidence of 32%. These injuries were more common in adults (69%) than in children (31%). Most reported head traumas were mild and were considered an expected outcome of seizures.3
No significant difference was found in the seizure-related injury between patients with focal epilepsy and idiopathic epilepsy (IGE) despite the higher frequency of Generalized Tonic-Clonic seizures (GTCS) in patients with IGE.15 However, our data revealed that injuries were more common in patients with genetic generalized epilepsy than other causes of epilepsy (P = .02).
Burns was among the most severe injuries, especially domestic traumas, sustained by patients with epilepsy.16, 23, 24 The burns occur in 38% of patients, and 5%-10% of patients may require hospitalization.25 However, the incidence of burns was low in our study population, with only 7% of patients sustaining burns. Furthermore, all patients who sustained burns were adults.
Fractures in patients with epilepsy could result from a seizure attack or because of the side effects of antiseizure medications.26-28 A previous study34 demonstrated that 11% of all epilepsy-related accidents resulted in fractures but revealed no significant difference in the frequency of fractures between the epileptic and nonepileptic groups. Antiseizure medications also affect bone metabolism and sometimes lead to osteomalacia, increasing the risk of fractures. In addition, some antiseizure drugs have sedative effects that can cause an imbalance and subsequently increase the risk of falls and fractures.11 However, we observed that fractures were among the less common types of traumas. Only 6.5% of our patients experienced fractures, and most (99%) patients with fractures were adults.
Shoulder dislocation is another type of bone injury observed in patients with epilepsy. It should be suspected if a patient complains of pain or limitation in shoulder movement after convulsions.29, 30 Shoulder dislocation is more frequent in patients with generalized tonic–clonic seizures and prolonged generalized epilepsy.3 Only 7% of our study population experienced dislocations; none of these patients were children. Dental injuries were less frequent, with an incidence of 8.5% (84% adults and 16% children), and submersion was the least reported accident (2%).
Seizure-related accidents can occur anywhere but most commonly happen at home, with an incidence of 7% and 11% among patients with epilepsy at 1 year and 2 years, respectively.11, 13 By contrast, the incidence is only 3% and 5% in a control group at 1 year and 2 years.15Moreover, most patients who sustain domestic traumas that necessitated hospitalization are females.16, 23 These findings are consistent with our study's findings, indicating that most injuries happened at home (70%). Other common locations of injuries included roads (traffic accidents) and workplaces.11 Traffic accidents sometimes are underestimated because patients with epilepsy underreport accidents.11, 31-33 Moreover, 54% of drivers with epilepsy involved in car crashes are unauthorized to drive.29 Saudi Arabia does not have specific regulations or laws that regulate driving policies for patients with epilepsy. Our study showed that approximately 26% of patients with epilepsy who drive were involved in car crashes.
In a previous retrospective study, nearly 50% of patients with generalized tonic–clonic seizures had major traumas and injuries. Seizure frequency was the only independent predictor of epilepsy-related accidents.13 Other studies15 indicate that seizure type and recurrence were the most common risk factors for sustaining seizure-related injuries. The most frequent seizure type associated with head injuries were atonic seizures and generalized tonic–clonic seizures.34 Hospital admission is required in 1.7%-11% of total cases of head traumas.22, 35, 36
Seizure frequency and type were not the only predictors of epilepsy-related accidents in this analysis. The number of antiseizure medications was also a potential predictor of injury. Approximately 72% of patients with seizure-related traumas were on polytherapy (P = .003) compared to 52% of noninjured patients with epilepsy. However, this may be due to a higher frequency of daily and monthly seizures in polytherapy patients, contributing to the high incidence of seizure-related injury (Table 2). Furthermore, injury frequency was higher among patients with daily, weekly, and monthly seizures than in patients who experienced less frequent seizure attacks (P = .001). We also found that 76% of patients who sustained injuries more than twice experienced tonic–clonic seizures (generalized onset or focal to bilateral) as the most common type of epilepsy, whereas 27% of patients who sustained injuries only once had focal impaired awareness seizures (P < .001). More than twice, patients who suffered injuries also had more discrete traumas: 89% sustained fractures, 75% sustained dental injuries, 58% sustained soft-tissue injuries, and 48% sustained head injuries. Moreover, the injury frequency increased as the epilepsy duration increased. The incidence of injury was low in patients who had epilepsy for <1 year (P < .001), whereas 64% of the patients who had epilepsy for >10 years had sustained injuries multiple times (P = .003). We did not find a relationship between the type of injury and the requirement for hospitalization or injury outcome (Table 3).
| Injury outcome | Count | Distribution of injury outcome |
|---|---|---|
| Lifelong effects such as permanent deficit | 2 | 2% |
| Short-term loss of function | 26 | 29% |
| No effect on function | 58 | 67% |
We also searched the social and work limitations among patients with epilepsy in the adult group and found no association between injuries and developing work restrictions. However, 38% of patients who reported social limitations had sustained injuries more than twice, and 62% of patients who had no social restraint had not suffered injuries (P = .01) (Table 4).
| Variable | Injured | Noninjured | |||
|---|---|---|---|---|---|
| Count | Percent | Count | Percent | ||
| Work limitation | Not bothered at all | 13 | 44% | 16 | 55% |
| Bothered | 7 | 86% | 1 | 14% | |
| Social limitation | Not bothered at all | 35 | 37% | 59 | 64% |
| Bothered | 33 | 73% | 12 | 27% | |
The treating physicians should counsel patients with epilepsy about seizure-related accidents and advise them about the required precautions to prevent traumas. In addition, the patients should be aware of the importance of compliance with antiseizure medications to keep their seizures under control, which is an essential step to reduce the risk of seizure-related accidents. Other guidelines included improving bone health by performing regular exercise and taking vitamin D supplements, particularly for high-risk patients, avoiding unsupervised bathing or cooking, and potential falls.30 Our survey also revealed that 91% of patients with monthly seizures were informed about sleep deprivation as a seizure trigger. In contrast, only 56% of patients with weekly seizures were informed about lack of sleep as a trigger.
3.1 Limitations
We relied on the respondents' recall of the information, mainly trauma 12 months from the last seizure; therefore, recollection bias could exist. Also, we could not find similar studies in Saudi Arabia or the Arab world to compare their findings with our findings. However, our study can be the opening step for future multicenter studies. This study was conducted in a referral population for a limited period. Thus, some aspects were not covered sufficiently in this study (e.g., risk of accidental death or SUDEP).
4 CONCLUSION
Two out of five of the participants reported physical injuries in our study. Soft-tissue injuries and head traumas were the most common injuries among PWE. Moreover, the injury frequency increased as the duration of epilepsy increased. Most of the traumas were at home. The factors associated with seizure-related injuries included polytherapy, generalised tonic-clonic seizures, and long periods of epilepsy. Thus, we suggest developing injury prevention strategies in PWE, especially for those at risk, and further studies exploring social and work limitations in this population are also needed.
ACKNOWLEDGMENTS
This work was accomplished by cooperating with the patients with epilepsy and their families at King Fahd Medical City (Riyadh, Saudi Arabia). Dr Hamhom and Dr AlKharisi interviewed the patients. Dr AlDosari and Dr Hameed revised the collected data among the adult patients, and Dr AlOtaibi revised it among the pediatric patients. Dr Alenizi and Dr Eskandrani helped to enter the data.
CONFLICT OF INTEREST
There are no conflicts of interests. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with these guidelines.