Physical activity as a prognostic factor of pain intensity and disability in patients with low back pain: A systematic review
Abstract
Background and objective
Identifying factors that influence the course of low back pain (LBP) is important to help clinicians to identify those patients at higher risk of non-recovery. The objective of this systematic review was to investigate the prognostic role of physical activity in the course of LBP.
Databases and data treatment
Literature searches were conducted in five electronic databases from their inception to February 2018. Prospective cohort studies investigating the influence of any type of physical activity in people with LBP were considered eligible. The primary outcomes were pain intensity and disability. Two independent reviewers extracted the data and assessed the methodological quality of the included studies. Results were stratified according to participants’ symptoms duration at baseline.
Results
Twelve studies were considered eligible for this review. Of these, six included patients with chronic LBP, four studies did not specify the patients’ duration of symptoms, one study included patients with acute LBP, and one study included patients with subacute LBP. Included studies were heterogeneous in terms of physical activity assessment, outcomes, follow-up duration, and statistical methods, therefore, pooling of results was not performed. We found limited evidence to support the prognostic role of physical activity in the course of LBP.
Conclusions
Our review identified limited evidence supporting physical activity as a prognostic factor in LBP. Future cohort studies are needed to clarify the strength and importance of this association.
Significance
Despite recent research in the area, this systematic review shows that there is low quality evidence that physical activity may not be a prognostic factor for predicting pain and disability in patients with LBP.
1 INTRODUCTION
Low back pain (LBP) is the leading cause of years lived with disability, imposing an enormous economic burden on individuals and society (Vos et al., 2012). Although most patients with LBP have a favourable prognosis and improve after a few weeks (Menezes Costa et al., 2012), about 15% of patients do not recover and develop chronic symptoms (i.e. pain lasting for more than three months) (Freburger et al., 2009; Shmagel, Foley, & Ibrahim, 2016). Patients with chronic LBP are responsible for a substantial proportion of health care costs related to LBP due to health care provider visits, medical comorbidities and absence from work (Depont et al., 2010; Ekman, Jönhagen, Hunsche, & Jönsson, 2005; Gore, Sadosky, Stacey, Tai, & Leslie, 2012; Shmagel et al., 2016). Identifying factors that influence the course of LBP is important to advise patients about their condition, inform the development of new treatment strategies and, consequently, reduce the LBP burden on health care systems and individuals.
Physical activity is thought to play an important role in the prognosis of LBP but its influence may vary according to the duration of symptoms. Considering that individuals with acute LBP present favourable prognosis after six weeks (Menezes Costa et al., 2012), there might not be enough time for them to show great changes in the overall physical activity levels. In contrast, individuals with chronic LBP have worse prognosis with a slow recovery (Menezes Costa et al., 2012) being more likely to experience physical deconditioning. Thus, we argue that the physical activity levels may have a greater impact on the prognosis of patients with chronic LBP when compared to patients with acute LBP. However, there is a lack of studies investigating which factors may influence or mediate this association in people with acute LBP and chronic LBP. In fact, a previous review conducted by Hendrick et al. (2011) found limited evidence due to the lack of observational cohort studies specifically designed to investigate the role of physical activity as a prognostic factor. Hence, the importance of physical activity in predicting the course of LBP remains unknown.
Perhaps reflected by the emerging initiatives (Lobelo, Stoutenberg, & Hutber, 2014; O'Keeffe, Maher, & O'Sullivan, 2017; Parra, Bradford, Clark, Racette, & Deusinger, 2017) for promoting physical activity among patients with musculoskeletal pain, the number of publication on this area has increased since the publication of the earlier review (Hendrick et al., 2011). The objective of this review was to investigate the role of physical activity as a prognostic factor in the course of LBP. Understanding the prediction role of different forms of physical activity on prognosis of patients with LBP may help clinicians to identify those patients with worse prognosis as well as better inform patients about their likely prognosis.
2 METHODS
We conducted a systematic review investigating the role of physical activity as a prognostic factor for LBP. The protocol of this systematic review was registered a priori in PROSPERO (CRD42018086099) (Oliveira, Elkins, et al., 2018). In addition, this review conforms with the meta-analysis of observational studies in epidemiology (MOOSE) guidelines (Stroup et al., 2000).
2.1 Searches
Literature searches were conducted on 02 February 2018 in the following electronic databases from their inception: MEDLINE via OVID, EMBASE (www.embase.com), CINAHL via EBSCO, SPORTDiscus via EBSCO and Web of Science. We combined search terms related to physical activity (e.g. physical activity, exercise therapy, motor activity, walking, running), LBP (e.g. back pain, lumbago, backache, spinal pain) and longitudinal studies (e.g. prognostic studies, cohort). Additionally, we checked the reference lists of included studies and relevant systematic reviews in the field in order to identify additional relevant publications. The results were restricted to publications in English, Spanish and Portuguese. Supporting information Appendix 1 details the search strategy used in Medline.
Two independent reviewers (F.G.S. and T.M.H.) screened titles and abstracts retrieved by the search strategy. The records selected for full text screening were assessed by two independent reviewers (F.G.S. and T.M.H.) In case of disagreement, a third reviewer (R.Z.P.) was consulted to arbitrate.
2.2 Study selection
Prospective cohort studies investigating people with LBP from any setting were eligible. No restriction was applied regarding the follow-up duration. In addition, studies had to report data for at least one or more of the following outcomes at follow-up: pain intensity, disability and any measure of recovery. We excluded studies reporting secondary analysis from randomised controlled trials. In addition, we also excluded occupational studies because they may restrict the generalizability of our results.
We included studies recruiting adults aged 18 or more with nonspecific LBP, without restriction regarding symptom duration. Studies including participants with specific forms of LBP such as spinal canal stenosis, nerve root compromise, LBP related to pregnancy or surgical procedure, as well as serious underlying conditions related to LBP such as fracture and tumour were excluded. Studies that included a broad sample of people with LBP were included only if data for those with non-specific LBP was reported separately. Studies investigating general musculoskeletal disorders were excluded if data for people with nonspecific LBP was not provided separately.
Physical activity measured at baseline during an episode of LBP was considered the prognostic factor. We included physical activity levels measured by subjective (e.g. questionnaires and physical activity diary) and objective methods (e.g. accelerometer, pedometer, VO2). In addition, we included physical activity reported as frequency (e.g. once a week or twice a week), types of physical activity (e.g. leisure and incidental physical activity), and engaged or not engaged in any physical activity.
2.3 Data extraction and quality assessment
Two independent reviewers (C.B.O. and R.J.T.) performed the data extraction of the included studies using a standardized data extraction form as recommended by Cochrane (Higgins & Green, 2011). In case of disagreement, a third reviewer (R.Z.P.) arbitrated the discussion. We extracted the following information from the included studies: sample characteristics (e.g. size, source, symptoms duration, age, gender), inception time, duration of follow-up, physical activity measures, outcomes (i.e. pain intensity, disability, and recovery), confounders. When available, we extracted measures of association (e.g. Odds Ratio [OR] and beta coefficients) with their respective precision measures (e.g. 95% Confidence Intervals [CI]) as well as the raw data from each included study.
Two independent reviewers (C.B.O. and R.J.T.) assessed the methodological quality of the included studies using the Quality In Prognosis Studies (QUIPS) tool (Hayden, Windt, Cartwright, Cote, & Bombardier, 2013). In case of disagreement, a third reviewer (R.Z.P.) arbitrated the discussion. The QUIPS is a tool recommended by Cochrane to assess risk of bias in prognostic studies across six domains (Hayden et al., 2013): study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting. Considering the score in the items, each domain was judged as having low, moderate, or high risk of bias. An overall score was not calculated because this approach is not recommended by the developers of the tool (Hayden et al., 2013). The reviewers used a standardised form downloaded from the website of Cochrane Methods Prognosis (Supporting information Appendix 2) and received the same level of training on how to use the form a priori.
2.4 Data synthesis and analysis
We planned to calculate pooled estimates through meta-analysis using random effect models, however, this was not possible due to the heterogeneous type of measures for assessment of physical activity (subjective and objective methods), LBP outcomes, duration of symptoms (acute, subacute and chronic LBP), follow-up duration (three months to five years), and statistical analysis methods (linear regression, logistic regression, difference between groups). Therefore, we reported the quantitative results narratively using the estimates reported in the included studies according to symptoms duration (e.g. acute and sub-acute LBP, chronic LBP or LBP without specifying duration of symptoms).
- High quality—very confident that the true effect lies close to that of the estimate.
- Moderate quality—the true effect is likely to be close to the estimate, but there is a possibility that it is substantially different.
- Low quality—the true effect may be substantially different from the estimate.
- Very low quality—the true effect is likely to be substantially different from the estimate.
3 RESULTS
The search strategy retrieved 11,052 titles, excluding duplicates. After screening titles and abstracts, we evaluated 157 potentially eligible full-texts articles. Of these, we excluded 145 articles and the reasons for exclusions are provided in Supporting information Appendix 3. Finally, 12 studies (Bohman, Alfredsson, Hallqvist, Vingård, & Skillgate, 2013; Bousema, Verbunt, Seelen, Vlaeyen, & Knottnerus, 2007; Cecchi et al., 2014; Feitosa, Lopes, Bonfa, & Halpern, 2016; Hendrick et al., 2013; Huijnen et al., 2011; Hussain et al., 2016; Jacob, Baras, Zeev, & Epstein, 2004; Mortimer, Pernold, & Wiktorin, 2006; Nordeman, Thorselius, Gunnarsson, & Mannerkorpi, 2017; Pinto et al., 2014; Roffey et al., 2011) were included in this review (Figure 1).
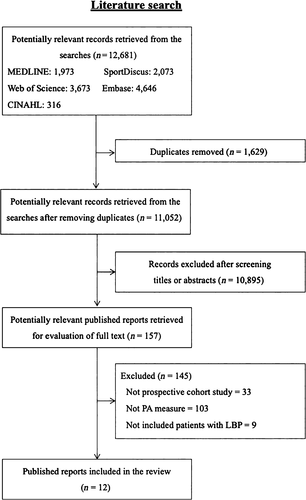
Abbreviations: LBP, low back pain; PA, physical activity
Table 1 provides the characteristics of the included studies. The sample size of included studies ranged from 46 to 4,074 participants with a mean age ranging from 37 to 70 years. The participants of the studies were recruited from general population (n = 3), primary care (n = 6), secondary care (n = 2) and tertiary care (n = 1). Six studies (Bohman et al., 2013; Cecchi et al., 2014; Feitosa et al., 2016; Huijnen et al., 2011; Nordeman et al., 2017; Pinto et al., 2014) included patients with chronic LBP, four studies (Hussain et al., 2016; Jacob et al., 2004; Mortimer et al., 2006; Roffey et al., 2011) did not specify the duration of symptoms, one study (Bousema et al., 2007) included patients with subacute LBP and one study (Hendrick et al., 2013) included patients with acute LBP. Regarding the outcome assessment, 10 studies (Cecchi et al., 2014; Feitosa et al., 2016; Hendrick et al., 2013; Huijnen et al., 2011; Hussain et al., 2016; Jacob et al., 2004; Mortimer et al., 2006; Nordeman et al., 2017; Pinto et al., 2014; Roffey et al., 2011) assessed disability, 6 studies (Feitosa et al., 2016; Hussain et al., 2016; Jacob et al., 2004; Mortimer et al., 2006; Pinto et al., 2014; Roffey et al., 2011) assessed pain intensity and 2 studies (Bohman et al., 2013; Bousema et al., 2007) used a measure of recovery. The follow-up assessment of the outcomes ranged from 3 months to 15 years. Most studies (n = 9) (Bohman et al., 2013; Cecchi et al., 2014; Feitosa et al., 2016; Hussain et al., 2016; Jacob et al., 2004; Mortimer et al., 2006; Nordeman et al., 2017; Pinto et al., 2014; Roffey et al., 2011) assessed physical activity through self-report measures (e.g. questionnaires or yes-or-no, Likert scale and open-ended questions) and three studies (Bousema et al., 2007; Hendrick et al., 2013; Huijnen et al., 2011) evaluated physical activity level using objective measures (e.g. accelerometer).
| Study, author (year) | Participants | Setting/Country | Pain duration | Physical activity measure | Outcomes | Confounders | Follow-up |
|---|---|---|---|---|---|---|---|
| Bohman et al. (2013) | 1836 participants (M: 632/F: 1,204). Mean age (SD): 56 years (14) | General population/Sweden | Chronic LBP (i.e. pain lasting for more than 6 months) | Self-report measure—a single question to classify the patients in sedentary, low, moderate and high physically active | Recovery (i.e. without back pain lasting for 7 days or more, during the latest 5-year period) | Physical activity, BMI, age and neck pain for men and PA, BMI and age for women | 5 years |
| Bousema et al. (2007) | 106 participants (M: 58/F: 46). Median age (IQR) 37.0 years (32.0 to 44.8 years) | Primary care/Netherlands | Subacute LBP (i.e. four to seven weeks after pain onset) | Accelerometer (Total sum counts/day) | Recovery (i.e. persons without back pain or those who were free of complaints for more than three weeks) | Without adjustment | 1 year |
| Cecchi et al. (2014) | 211 participants (M: 64/F: 147). Mean age (SD) 70.4 years (11.9) | Secondary care/Italy | Chronic LBP (i.e. pain lasting for more than 6 months) | Self-report measure—the practice of physical activity (i.e. yes/no) | Disability (i.e. RMDQ) | All significant variables were included in the final model including demographic, social and clinical variables | 1 year |
| Feitosa et al. (2016) | 113 participants (M: 32/F: 81). Mean age (SD) 53.0 years (12.2) | Primary care/Brazil | Chronic LBP (i.e. pain lasting for more than 3 months) | Self-report measure—the practice of physical activity (i.e. yes/no) | Disability (i.e. RMDQ) and pain intensity (i.e. NRS 0-10) | Not adjusted. Only statistically significant variables were retained in the final models | 3 months |
| Hendrick et al. (2013) | 101 participants (M: 50/F: 51). Mean age (SD) 37.8 years (14.6) | Primary care/New Zealand | Acute LBP (i.e. pain lasting less than 6 weeks) | Accelerometer (i.e. vector magnitude, counts per hour, counts per week) | Disability (i.e. RMDQ) | Sex, occupation, BMI, as well as baseline levels of pain, depression, anxiety, emotional distress and fear avoidance and activity levels prior to the onset of LBP | 3 months |
| Huijnen et al. (2011) | 84 patients with LBP (M: 45/F: 39). Mean age (SD) 47.5 years (10.5) | Primary care/Netherlands | Chronic LBP (i.e. pain lasting for more than 3 months) | Accelerometer (i.e. daily uptime, activity-related style, fluctuations in activity) and self-report questionnaire (i.e. BPAQ) | Disability (i.e. RMDQ) | Age, gender, pain duration, mean pain intensity | 6 months |
| Hussain et al. (2016) | 4,074 patients with LBP (M: 1,794/F: 2,280). Mean age (95% CI) of 48.2 (47.8 to 48.5) | General population/Australia | Patients with LBP without specifying duration of symptom | Self-report measure (i.e. Active Australia Survey to measure the time spent in walking, moderate intensity and vigorous intensity activity | Chronic Pain Grade Questionnaire (CPGQ) was used to measure disability (0-6) and pain intensity (0-100) | Age, education, smoking status, dietary guideline index score, and body mass index | 15 years |
| Jacob et al. (2004) | 555 participants (M: 235/F: 320). Mean age (SD) 45.0 years (10.6) | General population/Israel | LBP during the previous month without specifying duration of symptom (yes/no) | Self-report measure (i.e. BPAQ) | Disability (i.e. RMDQ) and pain intensity (i.e. VAS 0-100) | Not adjusted. All independent variables with a statistically significant association were included in multivariate the model | 1 year |
| Mortimer et al. (2006) | 459 participants (M: 202/F: 257). 262 participants with 20 to 44 years | Primary care/Sweden | LBP without specifying duration of symptoms | Type and duration of exercise to calculate the energy expenditure expressed as MET | Disability and pain intensity measured using six questions proposed by Von Korff et al. | Not adjusted | 5 years |
| Nordeman et al. (2017) | 123 women with chronic LBP. Mean age (SD): 45 (10) | Primary Care/Sweden | Chronic LBP (i.e. more than 12 weeks of LBP) | Self-report measure—Total number of hours spent for light, moderate and vigorous activities | Disability (i.e. RMDQ) | Adjusted by age | 2 years |
| Pinto et al. (2014) | 793 participants (M: 341/F: 452). Mean age (95% CI) 45.6 years (44.6 to 46.6 years) | Secondary care/Denmark | Chronic LBP | Self-report measure—a single question to determine leisure time physical activity, sedentary, light, moderate or vigorous physical activity | Disability (i.e. RMDQ), leg pain intensity (average of the current, worst and typical pain intensity using the NRS 0-10) back pain intensity (i.e. average of the current, worst and typical pain intensity using NRS 0-10) | All independent variables with a statistically significant association were included in multivariate the model | 1 year |
| Roffey et al. (2011) | 46 participants (M: 9/F: 37). Mean age (SD) 50.1 years (12.9) | Tertiary care/Canada | LBP with any duration of symptoms | Self-report measure for physical activity at work and leisure time (i.e. 5-point Likert scale, where 1 was “inactive” and 5 was defined as “very active”) | Disability (i.e. ODI) and pain intensity (i.e. NPS 0-10) | The study reported only univariate analysis without adjustment | 1 year |
- Abbreviations: BPAQ, Beacke physical activity questionnaire; CI, confidence interval; F, female; IQR, interquartile range; LBP, low back pain; M, men; MET, metabolic equivalent; NPS, numerical pain scale; NRS, numerical rating scale; ODI, Oswestry disability index; RMDQ, Roland Morris disability questionnaire; SD, standard deviation; VAS, visual analogue scale.
Table 2 details the methodological quality of the included studies using the QUIPS tool. Most included studies were judged as having low risk of bias in the domains regarding prognostic factor measurement (9 out of 12 studies, 75%), study participation (10 out of 12 studies, 83%) and outcome measurement (12 out of 12 studies, 100%). In contrast, most included studies had moderate or high risk of bias in the domains regarding study attrition (9 out of 12 studies, 75%), study confounding (7 out of 12 studies, 58%%) and statistical analysis and reporting (5 out of 12 studies, 42%). The most common methodological flaws were failure to report the characteristics of the participants who dropped out (i.e. study attrition), not accounting for confounders in the study design and analysis (i.e. study confounding) and providing insufficient data to assess the adequacy of the analysis (i.e. statistical analysis and reporting).
| Study name | Study participation | Study attrition | Prognostic factor measurement | Outcome measurement | Study confounding | Statistical analysis and reporting |
|---|---|---|---|---|---|---|
| Bohman et al. (2013) | Low | Moderate | Low | Low | Low | Low |
| Bousema et al. (2007) | Low | Low | Low | Low | High | Moderate |
| Cecchi et al. (2014) | Low | Moderate | Moderate | Low | Low | Low |
| Feitosa et al. (2016) | Low | Moderate | Moderate | Low | High | Moderate |
| Hendrick et al. (2013) | Low | Moderate | Low | Low | Low | Low |
| Huijnen et al. (2011) | Low | Low | Low | Low | Moderate | Low |
| Hussain et al. (2016) | Low | High | Low | Low | Low | Low |
| Jacob et al. (2004) | Low | Moderate | Low | Low | Moderate | Low |
| Mortimer et al. (2006) | High | High | Moderate | Low | Moderate | Moderate |
| Nordeman et al. (2017) | Moderate | Moderate | Low | Low | Moderate | Moderate |
| Pinto et al. (2014) | Low | Moderate | Low | Low | Low | Low |
| Roffey et al. (2011) | Low | Low | Low | Low | Moderate | Moderate |
The association between physical activity and clinical outcomes were reported using regression coefficient, correlation coefficient, odds ratio, mean difference or p-values (Table 3). For acute LBP, only one study (Hendrick et al., 2013) reported no association between physical activity measured objectively with an accelerometer and disability at three-month follow-up. Similarly, one study in people with subacute LBP (Bousema et al., 2007) reported no association between physical activity levels measured with an accelerometer and recovery at 1-year follow-up.
| Study name | Predictor | Outcomes | Results | p | + | 0 | − |
|---|---|---|---|---|---|---|---|
| Acute and subacute LBP | |||||||
| Outcome: disability | |||||||
| Hendrick et al. | RT3 | RMDQ (0-24) | β 0.00 (95% CI: −0.00 to 0.00). | 0.20 | 0 | ||
| PAAE | RMDQ (0-24) | β 0.005 (95% CI: −0.15 to 0.026) | 0.59 | 0 | |||
| Outcome: Recovery | |||||||
| Bousema et al. | Counts per minute | Recovery (yes-or-no) | PA did not differ significantly over one year | 0.58 | 0 | ||
| LBP with any duration of symptoms | |||||||
| Outcome: Pain intensity | |||||||
| Hussain et al. | PA Time in men (Low intensity LBP compared to no LBP) | CPGQ (0-100) | OR 1.01 (95% CI: 0.8 to 1.2) | 0.92 | 0 | ||
| PA Time in men (High intensity LBP compared to no LBP) | CPGQ (0-100) | OR 1.24 (95% CI: 0.93 to 1.67) | 0.15 | 0 | |||
| PA Time in women (Low intensity LBP compared to no LBP) | CPGQ (0-100) | OR 0.95 (95% CI: 0.77 to 1.17) | 0.63 | 0 | |||
| PA Time in women (High intensity LBP compared to no LBP) | CPGQ (0-100) | OR 0.97 (95% CI: 0.74 to 1.26) | 0.83 | 0 | |||
| Mortimer et al. | Exercise Intensity in METs | Questions proposed by Von Korff et al. | There were no differences between groups considering exercise’ intensity | 0 | |||
| Roffey et al. | Leisure time PA | NPS (0-10) | The authors provided only the p-value | 0.59 | 0 | ||
| Work PA | NPS (0-10) | The authors provided only the p-value | 0.57 | 0 | |||
| Leisure time PA | NPS (0-10) | The authors provided only the p-value | 0.38 | 0 | |||
| Work PA | NPS (0-10) | The authors provided only the p-value | 0.56 | 0 | |||
| Outcome: Disability | |||||||
| Hussain et al. | PA Time in men (Low disability LBP compared to no disability) | CPGQ (0-6) | OR 1.10 (95% CI: 0.82 to 1.43) | 0.47 | 0 | ||
| PA Time in men (High disability LBP compared to no disability) | CPGQ (0-6) | OR 1.19 (95% CI: 0.85 to 1.65) | 0.31 | 0 | |||
| PA Time in women (Low disability LBP compared to no disability) | CPGQ (0-6) | OR 1.15 (95% CI: 0.9 to 1.47) | 0.26 | 0 | |||
| PA Time in women (High disability LBP compared to no disability) | CPGQ (0-6) | OR 1.04 (95% CI: 0.79 to 1.37) | 0.38 | 0 | |||
| Jacob et al. | Baecke | RMDQ (0-24) | “Care-seeking, physical activity, and demographic variables were not independent predictors of any of the secondary outcomes.” | – | 0 | ||
| Mortimer et al. | Exercise Intensity in METs | Questions proposed by Von Korff et al. | There were no differences between groups considering exercise’ intensity | – | 0 | ||
| Roffey et al. | Leisure time PA | ODI (0-100) | The authors provided only the p-value | 0.28 | 0 | ||
| Work PA | ODI (0-100) | The authors provided only the p-value | 0.36 | 0 | |||
| Leisure time PA | ODI (0-100) | The authors provided only the p-value | 0.96 | 0 | |||
| Work PA | ODI (0-100) | The authors provided only the p-value | 0.49 | 0 | |||
| Chronic LBP | |||||||
| Outcome: Pain intensity | |||||||
| Feitosa et al. | The practice of physical activity (i.e. yes/no) | NRS (0-10) | 4.15 (SE: 8.25) | 0.615 | 0 | ||
| Pinto et al. | Light activity versus sedentary | NRS (0-10) | β −0.2 (95% CI: −1.1 to −0.3) | 0.49 | 0 | ||
| MVPA versus sedentary | NRS (0-10) | β: −0.6 (95% CI: −1.0 to −0.1) | 0.03 | – | |||
| Outcome: Disability | |||||||
| Cecchi et al. | The practice of physical activity (i.e. yes/no) | RMDQ (0-24) | The authors provided the OR only for the independent predictors with p < 0.05. | 0.76 | 0 | ||
| Feitosa et al. | The practice of physical activity (i.e. yes/no) | RMDQ (0-24) | 7.18 (SE: 6.62) | 0.278 | 0 | ||
| Huijnen et al. | Daily Uptime | RMDQ (0-24) | β = −0.16 (95% CI: −0.20 to 0.002) | 0.12 | 0 | ||
| Activity-related style* | RMDQ (0-24) | β = −0.12 (95% CI: −1.36 to 0.40) | 0.28 | 0 | |||
| Nordeman et al. | Leisure time physical activity instrument | RMDQ (0-24) | r = −0.11 | 0.24 | 0 | ||
| Pinto et al. | Light activity versus sedentary | RMDQ (0-24) | β −2.5 (95% CI: −7.1 to 2.1) | 0.28 | 0 | ||
| MVPA versus sedentary | β −8.7 (95% CI: −14.2 to −3.1) | 0.002 | – | ||||
| Outcome: Recovery | |||||||
| Bohman et al. | Low versus sedentary in men | Recovery (yes-or-no) | RR: 1.01 (95% CI: 0.69 to 1.47) | NR | 0 | ||
| Moderate versus sedentary in men | Recovery (yes-or-no) | RR: 1.06 (95% CI: 0.66 to 1.71) | NR | 0 | |||
| High versus sedentary in men | Recovery (yes-or-no) | RR: 1.03 (95% CI: 0.60 to 1.75) | NR | 0 | |||
| Low versus sedentary in women | Recovery (yes-or-no) | RR: 1.46 (95% CI: 1.06 to 2.01) | NR | + | |||
| Moderate versus sedentary in women | Recovery (yes-or-no) | RR: 1.50 (95% CI: 1.02 to 2.21) | NR | + | |||
| High versus sedentary in women | Recovery (yes-or-no | RR: 1.66 (95% CI: 1.07 to 2.55) | NR | + | |||
- Abbreviations: LBP, low back pain; OR, odds ratio; PA, physical activity; PAEE, physical activity energy expenditure; SE, standard error.
- “+”—significant and positive association (i.e. harmful association for pain intensity and disability, but protective association for recovery).
- “0”—non-significant association.
- “−”—significant and negative association (i.e. protective association for pain intensity and disability, but harmful association for recovery).
- * Activity-related style contains activity mean, fluctuations act and daily uptime.
For chronic LBP, one study (Feitosa et al., 2016; Pinto et al., 2014) reported an association between self-reported physical activity and pain intensity (report size of effect here) and one study showed no association (Pinto et al., 2014). Five studies (Cecchi et al., 2014; Feitosa et al., 2016; Huijnen et al., 2011; Nordeman et al., 2017; Pinto et al., 2014) reported the association between physical activity and disability in patients with chronic LBP; four reported non-significant associations and one study (Pinto et al., 2014) a significant association (report size of association). One study (Bohman et al., 2013) investigated the association of physical activity and recovery as the outcome and reported a significant association of physical activity with being recovered in women but not in men with chronic LBP.
For patients with mixed duration of symptoms, none of the four included studies (Hussain et al., 2016; Jacob et al., 2004; Mortimer et al., 2006; Roffey et al., 2011) reported a statistically significant association of physical activity with pain intensity or disability.
According to the GRADE approach, the overall quality of evidence for pain intensity, disability, and recovery was low, downgraded for phase of investigation and inconsistency (Table 4).
| Outcome | Number of participants | Number of studies | Number of cohorts | Estimates | GRADE | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| + | 0 | − | Phase | Study limitation | Inconsistency | Indirecteness | Imprecicision | Publications bias | Rating quality | ||||
| Pain intensity | 6,040 | 6 | 6 | 0 | 5 | 1 | X | √ | X | √ | √ | √ | Low |
| Disability | 6,559 | 10 | 10 | 0 | 9 | 1 | X | √ | X | √ | √ | √ | Low |
| Recovery | 1,942 | 2 | 2 | 1 | 1 | 0 | X | √ | X | √ | √ | √ | Low |
- “+”, significant and positive association (i.e. harmful association for pain intensity and disability, but protective association for recovery); “0”, non-significant association; “−”, significant and negative association (i.e. protective association for pain intensity and disability, but harmful association for recovery); X, serious limitations; √, no serious limitations.
4 DISCUSSION
Our review demonstrated that there is low quality of evidence that physical activity may not be a prognostic factor for predicting pain, disability or recovery outcomes in LBP. We identified only two studies investigating the prognostic role of physical activity in acute and subacute LBP, showing no association of physical activity with clinical outcomes. For chronic LBP, most studies did not suggest that being more active was associated with less pain or disability or being recovered, but results were not consistent across all studies. Despite the limited number of studies including acute and subacute patients with LBP, the number of prospective cohort studies more than doubled (increased from four to 12 studies) since the previous review in this topic (Hendrick et al., 2011). However, the overall quality of evidence was low which suggests that further studies may impact our findings and makes difficult to reach definitive conclusions at present.
One strength of this review is the comprehensive search strategy conducted in five electronic databases. However, we could not exclude the possibility of missing studies because we restricted the publication languages to English, Spanish and Portuguese and used limited search terms for physical activity, due to the large number of records yielded. Another strength of this review is the use of the QUIPS tool recommended by the Cochrane Collaboration (Hayden et al., 2013) to assess risk of bias. The main limitation of this review was the use of different methods for measuring physical activity (e.g. single item, questionnaire, accelerometer) and statistical analysis methods (e.g. OR, beta coefficients or p-value of differences between groups) which contributed to the high heterogeneity among the included studies, and prevented us conducting meta-analyses.
Although it was not possible to draw any definitive conclusion regarding the association between physical activity and the course of LBP, our findings align with the results reported for chronic LBP in the previous review. Hendrick et al., (2011) found that physical activity did not predict pain intensity and disability in chronic LBP. However, there are important methodological differences between this review and previous one. First, the previous review (Hendrick et al., 2011) included not only prospective cohort studies (Bousema et al., 2007; Jacob et al., 2004; Mortimer et al., 2006; Oleske et al., 2006) but also randomized clinical trials. Patients agreeing to participate in a trial may have different characteristics to those taking part in observational studies due to treatment preferences (King et al., 2005, 1997) and symptom severity (Bedi et al., 2000). In fact, the results of secondary analysis of randomized clinical trials showed conflicting results for physical activity predicting clinical outcomes of patients with chronic LBP (Hurwitz, Morgenstern, & Chiao, 2005; Macedo et al., 2014). Second, the previous review did not account for duration of symptoms in the analyses. Although it was not possible to conduct a subgroup meta-analysis based on symptoms duration, we stratified the results for acute, subacute and chronic LBP. Finally, although the number of studies more than doubled compared to the previous review, there is still limited evidence supporting physical activity as a prognostic factor of the LBP.
The importance of physical activity among patients with LBP has been increasingly investigated in recent times (Morelhao et al., 2018; Oliveira, Franco, et al., 2018). However, the overall quality of evidence was low-quality evidence which suggests that better designed studies are still needed to draw definitive conclusions on this topic. Most studies included in this review measured the physical activity levels subjectively using single items or self-reported questionnaires. However, this method relies on the patient's report which might be subject to bias (e.g. recall and social desirability bias) (Adams et al., 2005; Janz, 2006). We would argue that future studies should measure physical activity levels using objective assessment method. In addition, our review identified only two studies recruiting patients with acute and subacute LBP. Future inception cohort studies investigating physical activity levels in patients with LBP with short duration of symptoms are warranted. Finally, future studies should consider addressing the methodological flaws frequently identified the included studies. Future studies would benefit from a better description of the patients lost to follow-up; better description of the use and measurement properties of confounders; adequate statistical methods; and improved clarity and completion of reporting.
5 CONCLUSION
There is low quality of evidence that physical may not be a prognostic factor for predicting pain and disability in patients with LBP as most studies demonstrated a lack of significant associations. Although the number of studies in the field has markedly increased, the overall quality of evidence is low which suggests that future studies may impact our findings. Future prospective cohort studies investigating and inception cohort and physical activity using objective measures in patients with LBP is needed to generate more precise estimates.
AUTHOR'S CONTRIBUTION
CBO and RJT drafted the manuscript. CBO, RJT, FGS, and TMH selected eligible studies from the systematic search as well as performed data extraction and ‘Risk of bias’ assessments of the included studies. MRF, MBP, PHF and RZP reviewed the systematic review methods and contributed with critical revision of the review for important intellectual content. All review authors participated in the interpretation of the results, reading and approving the final version of the manuscript.