Innate responses of B cells
Abstract
In this review, we describe the non-antibody-mediated functions of B cells within the immune system. In addition to antibody production, B cells also present antigen to T cells, programme T cell differentiation and regulate effector T cell responses and much of this is mediated by the cytokines they make. We focus on the potential of B cells to perform these functions simply as a result of activation via ‘innate’ receptors (e.g. Toll-like receptors) and often independently of BCR ligation. We feel an appreciation of these broad and often antigen-nonspecific functions is important at a time when there is an increasing use of B cell depletion as a therapy for autoimmune disease.
Abbreviations:
-
- CIA:
-
collagen-induced arthritis
-
- PRR:
-
pattern recognition receptors
Introduction
B cells are best known as antibody producing cells. Antibodies are a first line defence against infection and most vaccines work because they elicit a protective antibody response. However, there is darker side to antibody production if the B cells have a BCR specificity that reacts with components of self. The autoantibodies they make can then precipitate the panoply of inflammatory responses leading to the whole range of autoimmune diseases. It is perhaps not surprising, therefore, that clinicians wishing to alleviate symptoms and possibly treat the cause of autoimmune diseases in man should identify B cell depletion as an attractive therapy. The biological reagent (e.g. Rituximab), binding to the B cell-specific molecule CD20, already existed and was tried and tested in the treatment of non-Hodgkins lymphomas 1. The results of B cell depletion in treating a number of diseases have been more than promising 2–4 and so far the predicted drawbacks have not materialised. The most obvious potential side effect is that the patient becomes immuno-compromised and, therefore, susceptible to infection. The audit of B cell-depleted patients does not indicate any increased rate of infection, however, it is early days and much of the data derive from lymphoma patients. Still, it may be that the observed maintenance of circulating antibodies specific for previous infections or vaccinations provides sufficient protection 5. However, if we are to deplete B cells from people over long periods, we should be aware of the many non-antibody related functions of B cells and the potential ensuing effects if the B cell compartment is ablated. In this short review, we will demonstrate that B cell function in vivo is much more complex and diverse than simply making antibodies. B cells present antigen to T cells and then via mechanisms that involve both co-stimulation and cytokine production, they influence T cell differentiation and then, finally regulate the T cell response.
B cell activation
As part of the adaptive immune system B cells carry somatically re-arranged receptors (BCR) that they use to recognise, bind and internalise specific antigen. In most B cells this means that they have a single specificity for antigen and can respond only to that antigen by initiating a signal transduced into the cell via BCR-associated molecules such as CD79α and β. However, B cells can also be activated by a range of stimuli, independently of the BCR. For mouse B cells the classic mitogenic stimulus is lipopolysaccharide (LPS) 6, that we now know activates cells via a complex binding to LPS-binding protein (LBP), CD14 and Toll-like receptor (TLR) 4 7. Thus, LPS activation is a paradigm for the non-antigen-specific activation of B cells via innate receptors. Recently, it has become clear that B cells express most TLR and can respond to a variety of TLR ligands 8, 9, such as TLR2, TLR3, TLR5, TLR7 and TLR9. Their response to these stimuli can be to proliferate, to differentiate into antibody secreting cells, to become more efficient antigen-presenting cells (APC), or to secrete cytokines. Clearly, the responses of B cells to antigens in their environment are not solely mediated through the BCR. Crucially, B cells, as with all other APC, can respond to broad classes of antigen (pathogen) via innate, pattern recognition receptors (PRR) and as a result influence immune activation in the vicinity. This means that the response of the one of the major lymphocyte populations in secondary lymphoid tissues (up to 50% of cells) to pathogens expressing combinations of PRR ligands is initially driven, not by Ag-specific stimuli, but rather by the activation of PRR.
TLR activation of B cells and antibody secretion
The idea, mentioned above, that B cells when activated via TLR differentiate to become antibody-producing plasma cells (T-independent responses) is not a controversial one. However, in the last year or two, studies have been published, indicating that T-dependent antibody responses also require TLR activation of B cells 10, 11. The prevailing view prior to this had been that antigen-specific signals, through the BCR, in conjunction with help from T cells (CD40 ligand + cytokines) were sufficient for B cells to make antibodies to T-dependent antigens. The fact that T-dependent antibody responses are impaired in mice deficient in MyD88 (a TLR signalling adaptor protein) was thought to be due to a failure of T cell priming in association with dendritic cells (DC). Now, Pasare and Medzhitov 10 have suggested that MyD88-signalling is required also in B cells. This conclusion has not been met with universal approval. Nemazee and colleagues 12 have produced equally puzzling data to indicate that T-dependent antibody responses proceed quite normally in MyD88/TRIF double knockout mice that cannot transduce any TLR signal. They propose that PRR stimuli other than TLR are at work. The truth may lie somewhere in between, with particular subclasses of antibody being more or less dependent on TLR signals to B cells. For instance, several papers show that switching to the IgG2a isotype (IgG2c in C57BL/6 mice) is determined by and may require TLR9 signalling 13–15. Our own data on this from chimeras in which the B cell compartment is MyD88-deficient, also show that the IgG2a response to a variety of antigens is severely impaired and interestingly so is the IgM response (TB and DG, unpublished data), while all other IgG subclass responses are normal. TLR-mediated IL-6 production may be a significant driver of the IgM response 16.
TLR have been proposed to sustain long-lived serum antibody responses by stimulating (intermittently) differentiation of memory B cells into the long-lived bone marrow plasma cell pool 17. Again, this is controversial as it circumvents the need for T cell help for antibody secretion, with the attendant check on production of autoantibodies by somatically mutated, self-reactive memory cells. An alternative explanation may be provided by the observation of Dörner, Radbruch and colleagues 18, 19 that the antigen-nonspecific plasma cells seen on boosting are the result of mobilization of plasma cells from the bone marrow and not the bystander activation of memory cells. The absolute need for T cell help in the initiation of autoantibody production has also been called into question by Marshak-Rothstein 20 and Shlomchik 21 who have shown that co-ligation of BCR and TLR by autoantigen (e.g. DNA or RNA containing complexes) can cause autoantibody to be made, which in turn enhances delivery of Ab-autoAg complexes to TLR-containing processing compartment in plasmacytoid DC 22. This will initiate autoreactive T cell activation and so amplify the autoantibody response. Interestingly, the development of autoimmunity (lupus), including autoantibodies in BAFF-transgenic mice proceeds in the absence of any T cells 23.
B cells as APC in vivo
The dogma that most B cells possess just a single antigen-specificity has led to the notion that B cells are only effective APC for the antigen to which their BCR binds. This is largely true in vitro when B cells are given a protein antigen for which they have no BCR specificity; they present it very poorly, especially in comparison to DC 24. On the other hand they are just as efficient as DC when their BCR recognises the antigen 24. This has led to the perception that B cells do not contribute as APC in primary responses, as there are too few antigen-specific B cells available. The role of B cells in priming T cells has long been controversial with data from B cell-deficient mice both for 25–27 and against 28, 29. Recently, data have appeared suggesting that B cells may contribute surprisingly early. First, bone marrow chimeric mice, in which the B cell compartment lacks MHC class II, exhibit an impairment of T cell activation that can be seen at very early time points (day 3) following immunization 30. Secondly, in studies using an mAb to detect specific peptide-MHC class II complex on the surface of APC, the appearance of presumably immunogenic material on B cells is within hours 31 or even minutes 32 after intradermal injection of the antigen. Pape et al. 32 go on to show that follicular B cells acquire soluble antigen diffusing from the subcapsular sinus in lymph nodes draining sites of immunization, in a process that does not require intermediary DC. This stimulates them to move to the follicular-T zone border where cognate interaction with T cells occurs 32. The groups of Batista 33 and Cyster 34 have since shown that particulate (bacterial) antigens 33 and immune complexes 34 are also picked up by B cells in the region of the subcapsular sinus. In the spleen, marginal zone B cells have long been implicated in this process 35–37; there are B cells in lymph nodes that resemble marginal zone B cells 38. It may also be significant that marginal zone B cells are demonstrably the most efficient B cell APC 39. None of this usurps the role of DC in initial priming of T cells; naive B cells are still generally thought of as tolerogenic in their interaction with naive T cells 40, 41. However, it does suggest that very soon after infection/immunization (within hours, not days), B cells are actively contributing to the antigen-presenting/T cell programming activity.
How can this be if frequencies of antigen-specific B cells are so low? Several possibilities spring to mind. (i) Antigen-specific or cross-reactive B cells exist at higher frequencies than we currently appreciate. (ii) The lymphoid organs (especially the lymph nodes) are designed to allow the antigen-specific cellular interactions at very low frequency for the production of antibody responses (proposed by Jenkins and colleagues 32). (iii) B cells can take up and present antigen via receptors other than the BCR. Thus, antigens that carry PRR (e.g. TLR) may be more effectively taken up by B cells. Antigen-nonspecific B cells have been shown, in vivo, to acquire soluble protein, process and present it 42. Furthermore, TLR ligands on the same particle and in the same endocytic compartment of APC enable efficient presentation to and activation of CD4 T cells 43. This evidence does not address whether this is related to enhanced Ag uptake, however, TLR11 and/or associated molecules do seem to be involved in the uptake of the Toxoplasma gondii antigen, profilin 44. Interestingly, the recent demonstration of antigen capture by B cells in the subcapsule of lymph nodes and subsequent transport to the follicle is an antigen-nonspecific process, requiring the B cells to express complement receptor 2 (CR2); however, there is no indication that the antigen is taken up, processed and presented to T cells 34. The basis in physiological reality of these possibilities needs much more investigation. We have not considered here B cell presentation in the establishment and perpetuation of autoimmune disease; unfortunately it is beyond the scope of this brief review; see the reviews 5, 45 for a proper treatment of the topic.
B cell cytokines and T cell programming
B cells, like other APC, have a programming function in T cell differentiation and this is mediated by the secretion of cytokines. B cells are known to make a wide range of cytokines 46, 47. Lund and colleagues 46 have characterised cytokine-secreting B cells into subsets similar to Th1 and Th2, so-called Be1 (making IFN-γ and IL-12) and Be2 (making IL-4) (Be = B effector); both subsets make IL-2, IL-6 and IL-10 46. The cytokine production by B cells, however, needs to be distinguished as either “primary” or “secondary”. Primary production is elicited by primary stimuli, such as TLR, while secondary production requires the interaction of activated B cells with activated helper T cells. For instance, we can find no primary stimuli that elicit IL-4 production by B cells; however, if they are allowed to interact with IL-4-secreting, activated Th2 cells, they too will begin to make IL-4 48. In vivo this may be important for the establishment of Th2 immunity during infection 49. We have found that TLR ligands are the most potent stimuli for production of cytokine by B cells and that this can be augmented by T cell-derived costimuli such as CD40L 8. Although B cells do make cytokines when both BCR and CD40 are stimulated, we find that the cross-linking of BCR on TLR-activated B cells is often an inhibitor of cytokine production 8.
Several models have provided evidence for the programming role of B cells in the development of Th2 responses 50, 51. The basis of this might be related to IL-4 production 48, to delivery of co-stimuli such as OX40L 26, 52 or ICOSL 53, 54 or their production of IL-10 (down-regulating Th1 responses) 47. The role of B cells in the induction of other types of response has received less attention. In relation to Th1 differentiation, B cells make very little IL-12; on a per cell basis, they make 1000-fold less than DC 8, although one could argue that this might be important if large numbers of B cells are making it after polyclonal activation. B cells also make IFN-γ in response to combinations of TLR ligands (e.g. TLR2, 4 and 9), but not to single stimuli 8. It has been noted by Mastroeni and colleagues 55 that B cell-deficient mice do not mount protective Th1 responses to Salmonella typhimurium. Th1 development is also impaired in chimeras in which B cells do not express MyD88 and so is related to the TLR-mediated activation of B cells; however, it does not require them to make IFN-γ (TB and DG, unpublished observations). B cells make significant amounts of IL-6 in response to a variety of stimuli and exhibit TGFβ message, although the stimuli required for secretion of active TGFβ have not been defined. Any role for B cells delivering these two cytokines in Th17 generation 56 remains to be investigated.
B cells are not homogenous and there are differences in the propensity of different subsets to make cytokines. In relation to subsets, IL-10 has been most intensively studied. B1 B cells were the first to be recognised as IL-10 producers 57 and this is reflected in the role of neonatal CD5+ B cells in dampening acute inflammation in new born mice, by producing IL-10 58, 59. In adult mice, we find that marginal zone (MZ) B cells and B1 cells produce most IL-10 in response to TLR ligands (TLR2, 4 and 9), while, in comparison, follicular cells make very little 8, an observation supported by other labs 60. Other workers have suggested that transitional T2 B cells are the main IL-10 producers 61, although how this fits with their transient, differentiating nature is unclear. Interestingly, in our hands, a dichotomy in cytokine production exists as MZ B cells make IL-10 and no IFN-γ, while follicular B cells make IFN-γ but no IL-10 8.
B cells and regulation
B cells make both IL-10 and TGFβ and thus could conceivably be involved in the development of one of the regulatory T cell subsets. Dealing first with CD25+ FoxP3+ Tregs: the data in this area are limited, fragmentary and often contradictory; for instance in B cell–deficient mice there is no alteration in the numbers or function of CD25+ FoxP3+ Treg 62, while in Rituximab/B cell-depleted patients the numbers of these cells rise 63. In some disease models evidence points to a positive role for B cells in the Treg control of colitis 64 and of EAE 65, in anterior chamber (of the eye) immune deviation (ACAID) 66 and in transplant tolerance 67. In this last example, the authors raise the possibility that B cells render T cells (potential effectors) unresponsive and so, receptive to suppression by donor-specific Tregs. Thus, the involvement of B cells in Treg function is not necessarily an inductive one, but might involve a collaboration bringing about regulation or, recruitment of Treg to sites of inflammation, e.g. CNS 65. It should be remembered that each model has its own idiosyncrasies; for instance, in the NOD thyroiditis model, B cell-deficient mice are resistant to disease induction and the role of B cells in Treg function seems to be negative. It is proposed that B cells sustain a persistent presentation of autoantigen (in B cell-sufficient NOD mice) that renders effector T cells resistant to suppression by Tregs 62.
As discussed above the presentation of antigen by naive/resting B cells is thought to render naive T cells tolerant 40, 41. Recent data suggest that this tolerance may result from the generation of Tregs 68, 69 with an unusual phenotype, (CD25+, CD62L+ and FoxP3–) 69. During the in vitro culture with naive T cells, the B cells make IL-10 although this is not required for the development of this Treg population 69. It will be interesting to know if TGFβ is involved as small resting B cells express this cytokine 47. In contrast, several slightly older studies, showed that B cell-derived IL-10 was crucial for the resolution of EAE 70, the delayed progression of inflammatory bowel disease 71, and the prevention of induction of collagen-induced arthritis (CIA) 72. In all these cases the B cells involved were activated and consequently produced IL-10. How this B cell-derived IL-10 production mediates these effects has not been determined but the induction of a Treg population seems most likely.
In relation to this, Gray et al. 73 have recently linked the immune suppressive activity of apoptotic cells on the development of CIA, with IL-10 production by B cells. The injection of apoptotic cells prevented development of CIA, a protection that was dependent on both B cells and on IL-10 73. A dissection of the cell interactions indicated that apoptotic cells had a direct effect on B cells, which augmented their IL-10 production, which in turn caused the differentiation of a population of IL-10-producing T cells. B cells it seems induce Tr1 cells. It is worth noting that in these experiments the amount of IL-10 made by B cells (stimulated via TLR + apoptotic cells) is of a similar magnitude to that made by the effector T cells and thus the B cell-derived IL-10 is also likely to have effects independent of Tr1 cells. The unexpected link between B cell regulation and apoptotic cells raises the question of whether the recognition of apoptosis during inflammation is a common feature in triggering a resolving B cell cytokine response.
Concluding remarks
We are only beginning to understand the mechanisms by which B cells modulate T cell responses. At one extreme we may come to accept that innate (TLR?), non-BCR-mediated activation of B cells gives them the potential to be a dominant APC population following infection with organisms that carry TLR ligands. At the very least we can be certain that TLR-mediated cytokine production by B cells both drives T cell differentiation and regulates its excesses (inflammation). We have highlighted here the many non-antibody-mediated functions of B cells and have focused mainly on their positive roles (see summary in Fig. 1). In the light of these lessons, one might be reluctant to ablate B cells from patients, but in autoimmune disease the balance is dramatically tipped towards the very deleterious effects of B cell autoantibody production and/or autoantigen presentation and, therefore, such drastic action is certainly warranted. However, these patients need to be followed carefully as they may well tell us a more complete story of the way that B cells contribute in the round to immune responses and their modulation.
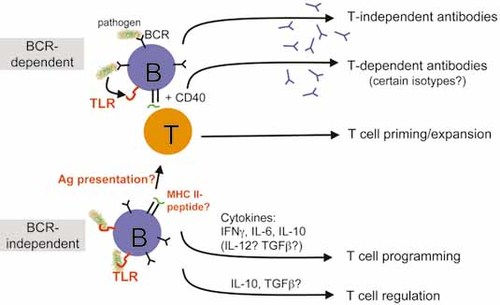
Roles of TLR in B cell responses. TLR activation alone can lead to antigen/BCR-independent antibody production, but most meaningful T-independent antibody responses in vivo involve Ag recognition by BCR. Note also that while cytokine production by B cells can be BCR independent, it may be enhanced by CD40 or modulated/altered by BCR signals.
Appendix
Conflict of interest: The authors declare no financial or commercial conflicts of interest.




