The practice gap in heart failure—the elephant in the room
Introduction
The recent publication of the 2016 European Society of Cardiology (ESC) Guidelines on the diagnosis and treatment of acute and chronic heart failure (HF)1 underlines the significant progress that has been made in the management of this syndrome in recent years. This very worthy publication outlines the many available and well-proven therapeutic options that are now available to effectively treat patients with HF, especially those with reduced ejection fraction.
However, despite this good news story, there remains a fundamental challenge in HF not given detailed discussion in the recent guidelines: namely, what is the optimal structure from which to direct these important therapeutic options outlined in the guidelines? The ESC Guidelines do recognize the importance of this issue by giving the recommendation that HF patients should have access to multidisciplinary disease management programmes and encourage “a ‘seamless’ system of care that embraces both the community and hospital throughout the health care journey”. Previously, the ESC Heart Failure Association Committee published on standards for delivering HF care.2 However, as outlined by international data, there are major challenges in implementing this vision. These deficiencies stem predominantly, in our opinion, from one central fundamental problem: a lack of cohesive interaction between primary care, where HF care should be centred, and specialist cardiologist input for advice and involvement on aspects of management at critical phases of the life cycle of a HF patient. Emergency department visits and hospitalizations continue to remain the major expenditures in HF care3 and strategies to aid in community management of HF and optimization of therapeutic strategies are required. Unless we address this deficiency many patients with HF will never see the benefits of strategies outlined in the guideline document and the gap between guidelines and practice will remain an insurmountable challenge.
Lack of specialist input to heart failure care?
Several data sets over the last 15 years indicate that a significant proportion of patients with possible or definite HF might not receive timely specialist input to their diagnosis and care.
In the early 2000s, publications suggested that only one-third of those with a clinical diagnosis of HF had echocardiography or further referral4 and this has not changed significantly in a more recent study.5 A publication this year from the Netherlands6 showed that 31% of the confirmed HF patient cohort of 434 people were managed solely within the primary care structure, as defined by no cardiology contact with the patient within an 18-month period. These data demonstrate that failure of onward referral to a specialist service for confirmation of diagnosis and the definition of investigations needed and therapeutic plan remains a significant problem. This may relate to difficulty in accessing diagnostic and specialist services from the community and the older multimorbid nature of these patients, which may lead to a reluctance to refer to multiple specialists. Studies have shown that patients discharged after initial management in a specialized HF clinic can be discharged to primary care for long-term follow-up with regard to maintaining guideline adherence and patient adherence7, 8 but it is not clear what is the best method to ensure that such patients have access to new therapies or new innovations in HF care.
What are the consequences?
The lack of specialist involvement in the confirmation of the diagnosis of HF and the onward definition of a care plan has been shown to result in significant ‘practice gaps’ in care with downstream clinical consequences. First, a failure to refer will compromise the accuracy of the suspected diagnosis of HF leading to incorrect treatment and failure to explore other diagnoses in those who do not have HF. Incomplete investigation and in particular the documented failure to perform echocardiography in many patients with suspected HF leads to a failure to phenotype HF as reduced or preserved ejection fraction (HRrEF or HFpEF, respectively), or indeed the newly defined HF with mid-range ejection fraction. Given the significantly different evidence bases for disease-modifying medications in these distinct HF subtypes this phenotyping as well as exploration of aetiology of HF is essential. In addition, a recent survey indicates a complete lack of comfort among general practitioners in managing HFpEF, underlining the need to involve this population in a shared care strategy,9 and other work has demonstrated that the prevalence of diastolic dysfunction is on the rise in older adults and is currently higher than that of systolic dysfunction,10 leading to the need for us to address this area urgently.
Other published work has underlined that general practitioner-alone directed care4 and non-cardiovascular specialist directed care11 results in less than optimal use of disease management pharmacological strategies in patients with HFrEF, and indeed will likely also reduce the use of proven effective devices, such as prophylactic implantable cardioverter defibrillator and cardiac resynchronization therapy. Appropriate education of patients and family members in necessary self-care strategies for day-to-day management of HF is essential but unlikely to happen outside structured disease management programmes. Therefore, it is clear that non-referral to specialist services is frequent and that the consequences are far reaching and compromise outcomes. However, given the increasing numbers of patients with HF and the difficulties of this patient group in accessing care what, if any, are the most practical solutions to this problem?
Potential solutions
The preferred health care delivery model for patients would have timely HF specialist involvement from the outset to confirm or rule out the initial diagnosis and, if confirmed, to establish an agreed investigative and therapeutic plan with the family practitioner. Subsequent to this, the patient should have access to a structured HF care programme in the community. Through this, and with the use of clinical decision support systems based in electronic health records, those who would benefit from new interventions based on the change in their condition or new guidelines would be highlighted and the specialist could interact with the family physician at such intervals to update the care strategy where necessary. We believe that given the increasing numbers of patients involved and the older multimorbid nature of this patient group that a structure such as this is required so that the patient's care will reflect not only advances in care but also the changing impact of any attendant co-morbidities and their therapies. From the outset of this strategy the patient and next of kin should be well-schooled in matters of self-care—a process that also requires updating at intervals.
The first step in developing this approach is for societies and organizations charged with advocating for the care of patients with HF and those involved in providing direction in primary care to issue firm guidance on care structure and specialist involvement in this condition. The major international society guidelines do not, in our opinion, emphasize this sufficiently at present. One exception is the recent publication by the National Institute for Health and Clinical Excellence (NICE) in the UK on timelines for specialist involvement in the diagnosis of new onset HF in the community.12 We believe that although timelines for access to diagnostics and specialist review may challenge many systems, modelling studies have suggested that a 6-month earlier diagnosis in HFrEF is associated with an increase in survival of 6 months over a 5-year period13 and therefore that guidance must be given on timelines for access to these vital services.
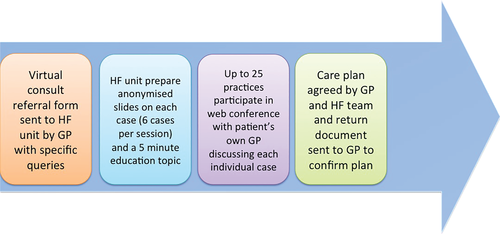
Even with advocacy in place there will be challenges in implementing this universal shared-care approach to HF. These will include insufficient cardiologists and primary care physicians in some jurisdictions, geographical remoteness in certain regions, a lack of structured HF care in primary care and, in some countries, a less than ideal link between primary and secondary care. All of these problems are surmountable. Strategies involving novel care delivery methods such as eHealth developments could potentially overcome many of these issues in an effective manner. We have recently deployed a primary care physician–specialist on line, providing real-time interaction to discuss patient's problems in HF. This application, which we refer to as Virtual Consultation, can host at one sitting up to 25 family physician practices, enabling specific case discussion but also a dissemination of practical tips in HF care (Figure 1). This strategy offers an alternative to standard clinical assessment, can provide the general practitioner with all the information that he/she requires, reduce need for onward direct referral and thereby can reduce ‘unnecessary’ travel for the patient and family—a very meaningful bonus for this type of interaction given the age and frailty of many patients with HF. This intervention also provides a user-friendly method to update the care strategy for a patient without necessarily requiring the patient to travel. Similar initiatives in other disease areas have had impressive results on disease management.14 This study showed that patients with hepatitis C infection can be managed as effectively in primary care, using a virtual consult model, as those at an academic medical centre in terms of sustained virological response.
In summary, despite the continued impressive advances in the therapeutic management of HF, the structure of care for a significant cohort of patients remains suboptimal from the outset. We believe that guidelines must now also give prominence to the structure of care as well as therapeutics in order to ensure that patients can realize the benefits of the advances in HF care seen in recent decades. This work focuses on the newly diagnosed and stable patient with HF but similar initiatives are likely to be applicable in terms of the recently discharged patient, for patient and carer education and in palliative care. Supported by strong advocacy from International Cardiology and Family Practice professional bodies, and enabled by modern health care delivery structures, we need to initiate strategies to bridge this ‘practice gap’.
Conflict of interest: none declared.




