Hypothetical dysfunction of the epithelial sodium channel may justify neurohumoral blockade in coronavirus disease 2019
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a recently emerged beta coronavirus pathogen, which was discovered in late 2019, and accounts for the coronavirus disease 2019 (COVID-19) pandemic. The infection presents a great threat to the clinical outcome, especially when the patient suffers from pre-existing cardiac conditions. Both cardiovascular (CV) risk factors and established CV diseases increase the vulnerability of patients to COVID-19 and the severity of the disease, while negatively influencing survival.
In general, increased cardiac stress due to hypoxaemia caused by respiratory failure as well as acute cardiac injury in response to the myocardial infection and systemic inflammation leading to massive cytokine release could all play an important role in disease progression.1 However, it still remains elusive how SARS-CoV-2 is able to present such a negative impact on the CV system. Thus, new insights into the molecular mechanisms in COVID-19 may enhance the better understanding of the disease course, thereby enabling the development of further therapeutic approaches.
The role of the renin–angiotensin–aldosterone system in coronavirus disease 2019
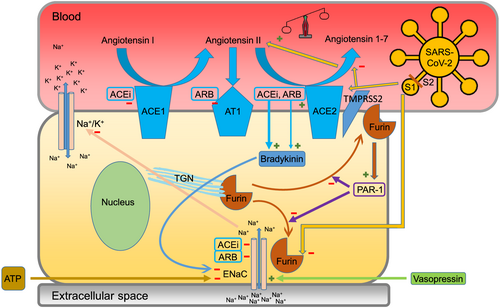
As SARS-CoV-2 utilizes a member of the renin–angiotensin–aldosterone system (RAAS), the cell surface protein angiotensin-converting enzyme 2 (ACE2) for viral entry,2 the in-depth understanding of the disease pathophysiology requires focusing on the RAAS. ACE2 is widely present in human cells, mainly in the pulmonary alveoli, the kidneys, the gastrointestinal tract, and the heart.3 The primary role of ACE2 is the inactivation of angiotensin II via hydrolysis, which degrades into the potent vasodilator heptapeptide angiotensin 1–7. This molecule exerts well-known protective effects on the CV system and also participates in bradykinin metabolism.4
Recently, a controversy has arisen regarding SARS-CoV-2-infected patients' RAAS-inhibiting co-treatments. On the one hand, the utilization of ACE2 by SARS-CoV-2 leads to the down-regulation and dysfunction of this receptor, thereby increasing the concentration of angiotensin II, along with its detrimental effects on the CV system via increased afterload, fibrotic remodelling, and cardiomyocyte hypertrophy. In this regard, RAAS inhibitors reducing angiotensin II levels may be beneficiary. On the other hand, RAAS inhibitors also cause the overexpression of ACE25; hence, they can potentially increase the severity of SARS-CoV-2 infection. In fact, current data support the idea that the use of RAAS inhibitors in COVID-19 seems to be safe without an apparent detrimental effect on the clinical outcome.6 Moreover, a study-level meta-analysis from China even showed a mortality benefit of hypertensive patients treated with RAAS compared with non-RAAS inhibitors.7 The intricate balance between ACE2 down-regulation by the viral infection and ACE2 up-regulation due to RAAS inhibition could, in theory, explain the above findings. Yet, no definitive pathomechanism has been confirmed so far, and the recommendation of major CV societies for the continuation of RAAS inhibitors in SARS-CoV-2-infected patients remains mostly empirical. Overall, to uncover possible RAAS-related pathways in COVID-19, one must take into account a complex, multifactorial regulation influenced by the viral infection, the inhibitory medication taken, along with prior CV conditions, and altered neurohumoral responses.
The spike protein of severe acute respiratory syndrome coronavirus 2 and the critical furin-mediated cleavage
Severe acute respiratory syndrome coronavirus 2 is an enveloped, single-stranded ribonucleic acid pathogen. Its entry into the host cell is mediated by the viral spike glycoprotein protruding from the lipid envelope. The spike protein is built up from two subunits, S1 and S2, which form homotrimers. The surface S1 subunit docks the human ACE2 receptor, as this subunit is the head of the projection and forms the receptor-binding domain. Thereafter, the genetic material of the virus can reach the host cell via two different pathways. In the endocytic pathway, the transmembrane S2 is required for the fusion of the viral and host cell membranes to form an endosome.2 In the direct membrane fusion pathway, the co-presence of the serine protease TMPRSS2 is also important, as it performs spike protein priming. SARS-CoV-2 has a human-specific recognition site between S1 and S2 for furin, which is a protease used to proceed with the cleavage in both the endocytic and the membrane fusion pathways.8 Furin cycles between the intracellular trans-Golgi network and the plasma membrane via an endosomal pathway.9 Alterations in furin expression as well as changes influencing its activity or localization create the basis for various disorders.10
The role of the epithelial sodium channel
The epithelial sodium channel (ENaC) is a transmembrane ion channel highly selective for sodium. Its primary effect is sodium reabsorption in the nephrons, colon, and lungs. It regulates cellular and extracellular osmolality via ion distribution, and consequently, it takes part in blood pressure homeostasis as well. The expression and activity of ENaC are regulated, among others, by the RAAS member aldosterone and also by furin.11 Without furin-mediated cleavage, a reduced effectivity of ENaC has been described. ENaC dysfunction can be better understood by studying one of the genetic disorders caused by the mutation of the genes encoding ENaC subunits. This condition is called multisystem pseudohypoaldosteronism (PHA), causing salt wasting and the lack of pharmacological response to aldosterone. Patients suffering from PHA have symptoms caused by severe hyponatraemia, hyperkalaemia, dehydration, and acidosis. It is an important observation that PHA presents with elevated renin and aldosterone levels. In addition, the dysregulation of ENaC activity leads to lower intracellular sodium concentrations, followed by insufficient Na+/K+-ATPase activity and, subsequently, an increase in serum potassium levels. Besides the epithelium, ENaC was also identified on non-epithelial sites, such as vascular smooth muscle and endothelial cells, with implications for regulating vascular tone. Furthermore, the expression of ENaC in platelets suggests its participation in thrombocyte activation as well.12
Extended regulatory network
As components of the RAAS, both angiotensin II and aldosterone up-regulate ENaC expression; at the same time, RAAS inhibitors negatively influence this effect. Moreover, RAAS inhibition results in elevated bradykinin levels, thereby interfering with the kallikrein–kinin system. Bradykinin counterbalances RAAS activation through B2 receptors. These are expressed in smooth muscle cells and vascular endothelial and kidney epithelial cells. When activated, they induce vasodilation via stimulating NO synthesis, while also reducing the probability of ENaC opening, thereby down-regulating its function.4 Importantly, ENaC is not exclusively controlled by the RAAS and furin. Previously, various aldosterone-independent pathways have been studied. Without aldosterone, the expression of ENaC may alone reach 30%. Vasopressin has also been identified as an important regulator. The level of vasopressin is controlled by plasma osmolality, and when elevated, vasopressin up-regulates ENaC expression. The complexity of ENaC regulation is further increased by extracellular adenosine triphosphate (ATP), which can reduce the probability of ENaC opening. Upon cardiac injury, when a huge amount of extracellular ATP becomes available, the role of this pathway may become decisive.13
Furin deficiency as a potential trigger for epithelial sodium channel dysfunction and renin–angiotensin–aldosterone system activation in patients infected with severe acute respiratory syndrome coronavirus 2
It was previously shown that the S1/S2 cleavage site of the SARS-CoV-2 spike protein is homologous to a peptide site of the ENaC, namely, the α-subunit extracellular domain. Furthermore, the cleavage of both the virus and ENaC are carried out at the cell membrane level. Therefore, in cells where ENaC and ACE2 are both presented (such as the alveolar epithelial cell), a competition may be present for furin-mediated cleavage upon SARS-CoV-2 infection.14 Interestingly, the tissue distributions of ENaC and ACE2 share similar sites, including nephron tubules, the lungs, the colon epithelium, and the vascular endothelium. Accordingly, a possible reduction of accessible furin during SARS-CoV-2 infection was proposed, leaving the activation of ENaC incomplete. This may have a negative effect on first-line pulmonary epithelial cells, leading to severe disturbance in ionic and fluid homeostasis, which could explain the rapid deterioration of patients with COVID-19. Besides this proposed competition, furin expression and activity may also be down-regulated during SARS-CoV-2 infection via a mechanism depending on the protease-activated receptor 1 (PAR1). Upon viral infection, PAR1 can directly block the proteolytic activity of furin by inhibiting its mobility towards the membrane-bound locus.15
Considering the potential deficit of the cellular furin pool during SARS-CoV-2 infection, we propose that the dysfunction of ENaC and consequent changes in electrolyte and fluid homeostasis certainly trigger and accelerate the activation of the RAAS (Figure 1). Therefore, this systemic neurohumoral response can justify RAAS inhibitors being favourable in COVID-19.
Conclusions and future perspectives
Our hypothesis of RAAS up-regulation due to ENaC disorder upon SARS-CoV-2 infection may contribute to a better understanding of the severe cardiopulmonary complications of the disease. The dysregulation of extracellular sodium levels and altered osmolality can culminate into hypovolaemia and, consequently, a generalized neurohumoral response activating the RAAS. Furthermore, the co-expression of ENaC and ACE2 on cardiac endothelial cells may enhance further deleterious CV effects in SARS-CoV-2 infection. This setting constitutes the basis for the advantageous effects of RAAS inhibition in COVID-19. Importantly, future investigations must provide proof of the current concept, by applying furin and renin measurements in different subgroups of patients suffering from COVID-19. Furthermore, basic research experiments may also contribute to fundamentally support or reject the current hypothesis.
Conflict of interest
None declared.
Funding
Not applicable.