Transvenous dual-chamber pacemaker after paediatric heart transplantation using left ventricle pacing through the coronary sinus
Abstract
A 12-year-old child with end-stage heart failure due to restrictive cardiomyopathy was submitted to orthotopic heart transplantation. Primary graft dysfunction required venous arterial extra-corporeal membrane oxygenation. Heart function normalized, but complete atrioventricular block remained after 3 weeks. A dual-chamber pacing with transvenous left ventricle pacing through the coronary sinus was performed. At 5-year follow-up, the patient is stable with the same pacing system and with preserved ventricular function.
Introduction
Although orthotopic heart transplantation is associated with cardiac denervation, it rarely requires post-operative permanent pacemaker because the restoration of sympathetic innervation is associated with improved responses of the heart rate and contractile function to exercise.1 Nevertheless, when present after 2 weeks, permanent complete atrioventricular block after transplant constitutes an indication for atrioventricular pacing, being the ventricular lead traditionally positioned in the right ventricle. Besides ventricular pacing being highly effective, it may induce abnormal electrical activation patterns, and the dyssynchronous pattern of ventricular activation is associated with structural ventricular remodelling and left ventricular dysfunction.2 As the degree of pacing-induced dyssynchrony varies amongst different pacing sites, the optimal site for pacing should aim at the prevention of mechanical dyssynchrony.
This case report describes the use of a coronary sinus lead designed for left ventricular pacing as the sole ventricular lead in a dual-chamber pacing system in a child with persistent complete atrioventricular block after heart transplant.
Case report
A 12-year-old female child with end-stage heart failure due to restrictive cardiomyopathy underwent orthotopic heart transplantation. Severe primary graft dysfunction was present during operation, requiring the use of venous arterial extra-corporeal membrane oxygenation. Heart function has completely recovered after 4 days, and her post-operative period was complicated by transient acute renal failure and complete atrioventricular block that lasted >3 weeks after the operation. In order to avoid left ventricle dyssynchrony and possible right ventricle lead damage due to multiple-rejection surveillance endomyocardial biopsies, a transvenous dual-chamber pacing using isolated left ventricle pacing through the coronary vein was indicated.
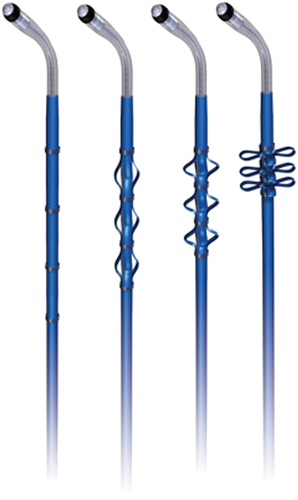
Under local anaesthesia and mild sedation, the left cephalic vein was cut down, and a guiding catheter was introduced into the subclavian vein and placed into the coronary sinus initially to perform a cardiac venogram (Figure 1). A unipolar steroid-eluting endocardial pacing lead with active fixation mechanism (Attain StarFix® 4195, Medtronic, Minneapolis, MN) was implanted into the anterior inter-ventricular vein branch (Figures 2 and 3). Measurements at implantation were as follows: threshold 2 V at 0.4 ms, R wave 6 mV, and impedance 300 Ω at 4.8 mA. A second bipolar steroid-eluting endocardial pacing lead with active fixation (2088T®, St. Jude Medical, Minneapolis, MN) was implanted at the right atrium.


Both leads were secured and connected to a rate-adaptive pacemaker (Accent DR®, St. Jude Medical, Minneapolis, MN) that was placed in a left infra-clavicle muscular pocket and programmed to VDD. The electrophysiological lead measurements were stable after the implant: ventricular threshold 1.5 V at 0.7 ms, R wave 4.5 mV, P wave 4.3 mV (bipolar), ventricular impedance 260 Ω, and estimated battery longevity 5 years.
The post-implant electrocardiogram showed right bundle branch block morphology-paced complexes (Figure 4), and the echocardiographic evaluation showed absence of atrioventricular, inter-ventricular, and intra-ventricular dyssynchronies. At 5-year follow-up, the patient remained in Functional Class I with the same pacing system and preserved ventricular function.

Discussion
The present report illustrates the use of dual pacing with left ventricular lead positioned transvenously through the coronary sinus after paediatric heart transplantation. The technique was feasible, safe, and effective at 5-year follow-up.
End-stage heart failure with dilated cardiomyopathy related to chronic isolated right ventricular pacing has been documented in children born with congenital complete atrioventricular block.3 In this regard, having a perspective of life-long pacing in children, the preservation of cardiac function during chronic ventricular pacing should be an important goal.
Right ventricular pacing is a simple option to this patient, but we also know the possible deleterious effect of inducible left bundle block mainly in young patients. In this particular population, the incidence of left ventricle dilatation and dysfunction can be 13.4%.3 For instance, a meta-analysis of cardiac resynchronization therapy in paediatric patients4 has shown that pre-existing pacing-related ventricular dyssynchrony related to previous right ventricular pacing occurs between 45% and 77%.
The decision of isolated left ventricle pacing instead of cardiac resynchronization therapy in this patient has several reasons: (i) deleterious effect of inducible left bundle branch block; (ii) recent history of primary graft dysfunction after heart transplantation; (iii) anatomic limitations of transvenous three leads positioned in a child; and (iv) possible equivalent clinical benefit to biventricular pacing.5 Liang and colleagues6 published a meta-analysis of controlled trials comparing biventricular to isolated left ventricle pacing. The type of pacing method did not correlate with better clinical status during midterm follow-up. However, there was a trend of biventricular pacing being superior in terms of preserving better left ventricle systolic function.
With respect to the technique of lead positioning, in older children, leads are often transvenously inserted and endocardially positioned at the right ventricle apex or septum, because it is technically safe, fast, and reliable; but a single-site left ventricle pacing might also be achieved safely by implantation of an active fixation lead via the coronary sinus. In this case, the coronary sinus lead dislocation was a concern. So we decided to use an active fixation left ventricle lead (Attain StarFix® 4195, Medtronic, Minneapolis, Minnesota), which found a 0.7% dislodgement rate over a mean follow-up period of 23 months.7
Isolated left ventricular pacing has been evaluated as an alternative to simultaneous or sequential biventricular pacing. Early experience confirmed comparable acute haemodynamic benefit of both left and biventricular pacing, and subsequent studies have demonstrated similar functional benefit and/or reverse remodelling of both strategies in patients with heart failure.5
In this specific patient, the only branch that fit an active fixation lead was the inter-ventricular branch. So we decided to try this pacing site, even acknowledging that it is not an ideal site. Despite that concern, we consider that a donor heart, which is a structural normal heart, may have a different behaviour when compared with a diseased one. That was proved to be effective, as it promoted a desirable depolarization (positive QRS in chest leads), with no mechanical dyssynchrony.
The His pacing certainly is a very good option in complete heart block after cardiac surgery. However, at the time of implant, we did not have the specific tools to utilize this technique.
In children with atrioventricular block and structurally normal hearts, the use of single left ventricle pacing as the preferred site for chronic ventricular pacing has been advocated,8 and small studies in children show that chronic left ventricle free-wall pacing may preserve ventricular function and dimensions comparable with those of healthy controls.9, 10 This is particularly important in paediatric heart transplant recipients because it may prolong graft function and patient survival.
In conclusion, dual-chamber pacing with transvenous left ventricle pacing through the coronary sinus is a viable and minimally invasive approach to complete atrioventricular block after paediatric heart transplantation, possibly minimizing the dyssynchronous pattern of ventricular activation due to right ventricle pacing.
Conflict of interest
None declared.