Self-esteem and peer-perceived social status in early adolescence and prediction of eating pathology in young adulthood
Funding information: Netherlands Organization for Scientific Research, Grant numbers: GB-MW 940-38-011, 100-001-004, 60-60600-97-118, 261-98-710, GB-MaGW 480-01-006, GB-MaGW 480-07-001, GB-MaGW 452-04-314, GB-MaGW 452-06-004, 175.010.2003.005, 481-08-013, 481-11-001, NWO Vici 016.130.002, NWO Gravitation 024.001.003; the Ministry of Justice and Security (the Netherlands); European Science Foundation, Grant number: EuroSTRESS project FP-006; Biobanking and Biomolecular Resources Research Infrastructure, Grant number: BBMRI-NL (CP 32); the Gratama foundation; the Jan Dekker foundation; the participating universities; and Accare Centre for Child and Adolescent Psychiatry
Abstract
Objective
Self-esteem is implied as a factor in the development of eating disorders. In adolescence peers have an increasing influence. Support for the role of self-esteem in eating disorders is ambiguous and little is known about the influence of social status as judged by others. The present study investigates whether self-esteem and peer status in early adolescence are associated with eating pathology in young adulthood.
Method
This study is part of TRAILS, a longitudinal cohort study on mental health and social development from preadolescence into adulthood. At age 11, participants completed the Self-Perception Profile for Children, assessing global self-esteem and self-perceptions regarding social acceptance, physical appearance, and academic competence. At age 13, peer status among classmates was assessed regarding likeability, physical attractiveness, academic performance, and popularity in a subsample of 1,007 participants. The Eating Disorder Diagnostic Scale was administered at age 22. The present study included peer-nominated participants with completed measures of self-perception at age 11 and eating pathology at age 22 (N = 732; 57.8% female).
Results
In a combined model, self-perceived physical attractiveness at age 11 and peer popularity at age 13 were inversely correlated with eating pathology at 22 years, while likeability by peers at age 13 was positively related to eating pathology.
Discussion
Both self-perceptions and peer status in early adolescence are significant predictors of eating pathology in young adults. Specific measures of self-esteem and peer-perceived status may be more relevant to the prediction of eating pathology than a global measure of self-esteem.
1 INTRODUCTION
Although eating disorders do occur in persons of middle and older age, disordered eating behaviors and eating disorders usually develop in adolescence (Hoek, 2016; Mangweth-Matzek, & Hoek, 2017; Smink, van Hoeken, & Hoek, 2012). The adverse effects on both mental and physical health are unequivocal (Field et al., 2012). Uncovering risk factors for eating pathology may offer clues for prevention. This study aims to disentangle the respective roles of global self-esteem, specific self-perceptions and peer-perceptions during early adolescence in the prediction of young adult eating pathology.
Low self-esteem is a relatively well-established, albeit nonspecific, risk factor for eating pathology (Allen, Byrne, Forbes, & Oddy, 2009; Allen, Byrne, Oddy, Schmidt, & Crosby, 2014; Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Micali et al., 2015; Pearson et al., 2017). Although a review by Stice (2002) indicated that high self-esteem is a protective factor against eating pathology, a recent review by Stice (2016) found no clear evidence for the protective role of self-esteem in eating disorders.
Reflecting the increased importance of peers in adolescence, self-esteem in this period is to a great extent shaped by social comparison with, and social support from, peers (Mann, Hosman, Schaalma, & de Vries, 2004). Hence, we consider self-esteem as an important factor to take into account when looking at how adolescents perceive themselves in relation to their peers (self-perceptions), how adolescents are perceived by their peers (peer-perceptions) and the respective roles of these perceptions in eating disorders. In doing so, we focus on perceptions in three important domains in adolescence: social standing, academic competence, and physical attractiveness.
Only a few studies examined the association between social standing and weight-related behaviors and cognitions. Self-perceived low social status has been linked to a range of mental disorders (Scott et al., 2014), including eating disorders (e.g., Troop, Andrews, Hiskey, & Treasure, 2014). In contrast to self-perceived social status, little is known about social status as perceived by others and its potential role in the onset of eating pathology. Graham, Eich, Kephart, & Peterson (2000) found that adolescents who are well-liked by peers, as assessed with peer nominations, are more satisfied with their bodies. This is in line with a longitudinal study (Rancourt & Prinstein, 2010) showing that, when controlled for baseline cognitions, well-liked early adolescents had fewer negative body-related cognitions after 11 months than disliked adolescents. On the other hand, likeability and negative body-related cognitions at baseline showed a negligible correlation in Rancourt's study, and Wang, Houshyar, & Prinstein (2006) found no association between adolescents’ likeability and body size or dieting behavior either. Lieberman, Gauvin, Bukowski, & White (2001) found that girls who received more friendship nominations were even more likely to exhibit disordered eating behaviors and displayed lower body esteem. Hence, the evidence is rather mixed.
In addition to likeability, we also examine the role of peer-perceived popularity, which emerges in adolescence as a distinct concept of social standing in the peer group (Cillessen & Rose, 2005). Whereas likeability indicates the extent to which adolescents are seen as nice and friendly by their peers, popularity captures those adolescents who are seen as powerful, influential, and attractive for affiliation without being necessarily well-liked in the peer group (Dijkstra, Cillessen, Lindenberg, & Veenstra, 2010). In a cross-sectional study among 17-year-old males and females, high peer popularity was associated with more dieting behaviors and a body shape that fits the current ideals for men (muscular) and women (thin) (Wang et al., 2006). Rancourt & Prinstein (2010) found that more popular adolescents were at greater risk of developing negative weight-related behaviors and cognitions than less popular peers. Other research showed that obese adolescents are less popular and more often socially rejected, viewed as less attractive, and labelled as ‘stupid’ or ‘lazy’ (Puhl & Latner, 2007). Neumark-Sztainer et al. (2002) found that both under- and overweight youth were bothered by being teased about their weight, and that in overweight youth in particular weight-teasing was associated with binge eating behavior. Hence, adolescents at both ends of the popularity continuum may be vulnerable for developing eating pathology, driven by status concerns and related stress within the peer group.
To our knowledge, there are no studies on eating disorder pathology in relation to the domains of academic competence and physical attractiveness (Feingold, 1992). Nevertheless, both academic competence and physical attractiveness constitute two important aspects in adolescence (Steinberg & Monahan, 2007). As adolescents spend a great amount of time in the presence of peers in school, social comparison regarding academic competence is inherently related to adolescents’ life. Adolescence is characterized by biological maturation and the initiation of sexual and romantic relationships. Social comparison on physical attractiveness is a natural part of this developmental phase. Hence, the three domains of social standing, academic competence, and physical attractiveness together cover important aspects of adolescents’ lives, steering their confidence and potentially affecting their susceptibility to develop eating disorders over time.
In the present study, we investigated associations between early adolescent self-esteem, self- and peer perceptions, and eating pathology in young adulthood. We hypothesized that low self-esteem and low self-perceptions and peer perceptions in the domains of social standing, academic competence, and physical attractiveness in early adolescence would predict eating pathology in early adulthood. Both low and high popularity are inherently stressful and adolescents at both ends of the popularity continuum may be vulnerable for developing eating pathology. Thus a U-shaped relation between peer-perceived popularity and eating pathology was expected.
2 METHODS
2.1 Study population
This study used a subsample of the Dutch prospective cohort study TRAILS (TRacking Adolescents’ Individual Lives Survey), which follows a community sample from early adolescence into young adulthood. The cohort has been extensively described elsewhere (Oldehinkel et al., 2015). In 2001, 2,230 children (mean age 11.1 years, SD = 0.6) from the north of the Netherlands, selected through community registers and through their schools, enrolled in the study. The cohort includes predominantly Caucasian children from five municipalities in both urban and rural areas. Follow-up assessments took place bi- or triennially (second assessment wave (T2): n = 2,149, response 96.4%, mean age 13.6 years, SD = 0.5; third assessment wave (T3): n = 1,816, response 81.4%, mean age 16.3 years, SD = 0.7; fourth assessment wave (T4): n = 1,881, response 84.3%, mean age 19.1 years, SD = 0.6; and fifth assessment wave (T5): n = 1,782, response 79.9%, mean age 22.3 years, SD = 0.7). The proportion of female participants ranged from 50.8% (T1) to 52.7% (T5). Informed consent was obtained from the parent(s) or guardian of the participants at T1-T3, and at T4 and T5 from the participants themselves. The Central Committee on Research Involving Human Subjects approved the study.
This study addressed TRAILS participants who had T2 peer nominations (N = 1,007; 46.9% of all T2 participants). At T2, classroom social status on several domains was assessed by means of peer nominations in classes with at least three TRAILS participants (Dijkstra et al., 2010). Peer nominations were obtained in 172 classes (72 first grade and 100 second grade of secondary education) at 34 schools. The school classes were more or less equally distributed across educational levels: 60 low, 53 middle, and 59 high education. The mean number of students in each participating school class was 18.4 (SD = 6.0, range 7–30). All students received a questionnaire (see Heading 2.2.1—Peer status) and a list of their classmates, and could nominate an unlimited number of classmates for every question. A total of 3,312 adolescents nominated their classmates, which yielded peer nominations for 1,007 TRAILS participants (51.3% female). The analyses in the present study included peer-nominated participants for whom completed measures of self-esteem (T1) and eating pathology (T5) were available, resulting in a final study sample of 732 participants (72.7% of those with peer nominations; 57.8% female) (Figure 1).
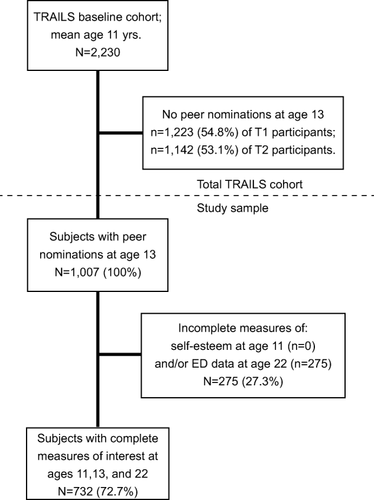
Inclusion of participants in the present study investigating adolescent self-perception, peer status, and risk of eating pathology
Compared to the remainder of the total TRAILS cohort (see Table 1), the study sample had a lower age-standardized body mass index (BMI; see Heading 2.2.3—Eating pathology) at T1, and more eating pathology at T5. Furthermore, they had higher self-esteem regarding social acceptance, academic competence and global self-esteem at T1. They were also somewhat younger at T2 and T5. Within the TRAILS subsample with peer nominations at T2, those with complete self-esteem (T1) and eating pathology (T5) measure were more often nominated for good looks and being a good learner, and less often for being popular by peers than those without complete study data.
| Mean (SD) | Difference | ||
|---|---|---|---|
| Variables | Study subsamplea | Remainder of TRAILS cohort | t-test (p-value) |
| Age | |||
| T1 | 11.09 (0.57) | 11.12 (0.55) | −1.286 (.199) |
| T2 | 13.47 (0.51) | 13.62 (0.53) | −6.011 (<.001) |
| T5 | 22.22 (0.65) | 22.34 (0.64) | −3.701 (<.001) |
| BMIb | |||
| T1 | −0.03 (1.05) | 0.08 (1.22) | −2.115 (.035) |
| T2 | −0.24 (1.05) | −0.22 (1.36) | −0.217 (.829) |
| T5 | 23.63 (4.16) | 23.79 (4.20) | −0.787 (.432) |
| T1 Self esteemc | |||
| Social acceptance | 3.10 (0.55) | 3.04 (0.60) | 2.504 (.012) |
| Physical appearance | 3.14 (0.61) | 3.11 (0.67) | 1.118 (.264) |
| Academic competence | 2.93 (0.50) | 2.85 (0.55) | 3.204 (.001) |
| Global self esteem | 3.37 (0.52) | 3.31 (0.56) | 2.172 (.030) |
| T2 Peer statusd | |||
| Likeability | 0.56 (0.20) | 0.55 (0.22) | 0.817 (.414) |
| Physical attractiveness | 0.21 (0.21) | 0.17 (0.18) | 3.115 (.002) |
| Academic performance | 0.33 (0.26) | 0.25 (0.24) | 4.441 (<.001) |
| Popularity | 0.10 (0.12) | 0.12 (0.14) | −2.451 (.014) |
| Eating pathologye | |||
| T5 | 11.25 (13.34) | 9.00 (12.85) | 3.408 (p < .001) |
- a Note Study subsample subjects (n = 732) are selected on the basis of the availability of peer nominations by classmates at the second assessment wave (T2; n = 1,007), and within this group those who have completed measures of self-esteem at the first assessment wave (T1) and of eating pathology at the fifth assessment wave (T5). N per variable may be lower than that for total N at assessment wave due to missing data in the larger TRAILS cohort, e.g., for BMI. Note that T2 peer status variables were only assessed in a subsample (n = 1,007) of the total TRAILS cohort; thus, n for the remainder of TRAILS subjects that had peer nominations but were not included in the present study is lower (n = 275) than that for other variables.
- b BMI: T1 and T2: z-score standardized for age according to WHO growth reference data for 5 to 19-year olds (de Onis et al., 2007; WHO, 2007). T5: absolute BMI (kg/m2).
- c T1 Self-esteem scales: Self-Perception Profile for Children (SPPC, Harter, 1982); scale scores could range between 1 (low self-esteem) and 4 (high self-esteem).
- d T2 Peer status: number of received nominations by classmates divided by total number of classmates; scores could range between 0 (no nominations) and 1 (nominated by all classmates).
- e Eating pathology: T5 standardized composite sum score of the Eating Disorder Diagnostic Scale (EDDS, Krabbenborg et al., 2012; Stice et al., 2000). Sum scores could range between 0 and 100.
2.2 Measures
2.2.1 Peer status
At T2 students could nominate their classmates on a total of eighteen topics, of which four were selected for this study. These concerned questions regarding likeability (‘Which classmates do you like?’), physical attractiveness (‘Who are good-looking?’), academic competence (‘Who are good at learning?’) and popularity (‘Whom do others want to be associated with?’). With regard to the latter, students were asked whom they thought others wanted to associate with, in order to disentangle personal preference from social impact. This measure of popularity shows similar associations with behaviors such as aggression, and characteristics such as physical attractiveness, as do other measures of popularity (most prominently: ‘who is popular’) (Dijkstra et al., 2009, 2010). The number of received nominations was divided by the number of classmates, yielding a proportion score ranging from 0 (no nominations) to 1 (nominated by all classmates).
2.2.2 Self-perception
The Self-Perception Profile for Children (SPPC, Harter, 1982) was administered at T1. The SPPC assesses children's general feelings of self-worth and self-esteem in five specific domains (academic competence, social acceptance, athletic competence, physical appearance, and behavioral conduct). Higher scores indicate higher self-esteem. The SPPC has been shown to have good reliability and validity: in a study by Muris et al. (2003) the test–retest stability of the SPPC over a 4-week interval was good: all intraclass correlation coefficients were .84 or higher. Furthermore, the SPPC correlated in a theoretically meaningful way with child-, parent-, and teacher-reports of psychopathology and personality (Muris et al., 2003). For this study, we focused on SPPC domains that corresponded with the peer-status domains under study, that is, academic competence, social acceptance and physical appearance, and on global self-esteem. Cronbach's alpha ranged from 0.71 to 0.81 for these SPPC scales.
2.2.3 Eating pathology
Eating pathology was measured at T5 by means of the validated Dutch translation of the Eating Disorder Diagnostic Scale (EDDS), a 22-item self-report questionnaire that generates DSM-IV diagnoses of anorexia nervosa (AN), bulimia nervosa (BN) and binge-eating disorder (BED), and an overall symptom composite score (Krabbenborg et al., 2012; Stice, Fisher, & Martinez, 2004; Stice, Telch, & Rizvi, 2000). For this study we focused on the EDDS standardized composite score, which was constructed by summing standardized item scores, excluding items regarding height, weight, and use of birth control. The composite score could range between 0 and 100. It indicates the level of eating pathology, not the specific type of eating problems, and has been shown to have satisfactory internal consistency (Stice et al., 2004). In a study using the Dutch translation of the EDDS, the mean (SD) standardized composite score in a nonclinical group (n = 45) of female university students without eating disorder diagnoses was 7.24 (6.63), the two-week test–retest reliability was 0.81 for female eating disorder patients (n = 59) and 0.69 for the healthy controls, and it showed a high correlation with the symptom composite score of the eating disorder examination (r = .85, p < .001) (Krabbenborg et al., 2012). In the same study a cut-off score of 16.5 represented the optimal sensitivity–specificity trade-off (sensitivity 0.88, specificity 0.91) for the standardized EDDS composite score.
The prediction T5 eating pathology by T1 and T2 variables may be confounded by the presence of eating pathology at T1 and/or T2. At T1 (age 11) and T2 (age 13) eating pathology was not assessed as such. To check for potential eating problems at T1 and T2, we looked at indicators for core features of eating disorders: compensatory behaviors for overeating and distorted body image (American Psychiatric Association, 2000). Overeating accompanied by compensatory behaviors was indicated by the combination of item scores ‘very true’ or ‘often true’ on T1 and T2 youth self-report (YSR) and child behavior checklist (CBCL) (Achenbach & Rescorla, 2001) items Overeating (YSR and CBCL item 53), and vomiting (YSR item 56g). YSR and CBCL items have moderate to good test–retest reliability (Achenbach & Rescorla, 2001). Distorted body image was operationalized as an incongruence between self-reported and objective body weight: item scores ‘very true’ or ‘often true’ on T1 and T2 self-reported Overweight (YSR item 55) were combined with T1, respectively T2, objective below average weight (a BMI z-score < 0). No information on self-reported underweight was available to check for an incongruence in objectively overweight subjects. For T1 and T2, BMI WHO growth reference data for 5–19 year olds were used, resulting in age-standardized BMI z-scores per gender (de Onis et al., 2007; WHO, 2007). At 19 years a BMI z-score of >1 corresponds to an absolute BMI of 25 kg/m2 (cut-off for overweight) and a z-score of >2 to a BMI of 30 kg/m2 (cut-off for obesity); a BMI z-score of −1 corresponds with an absolute BMI of 18.7 in females and 19.6 in males, a BMI z-score of −2 to a BMI of 16.5 in females (DSM-5: moderate underweight) and 17.6 in males (DSM-5: mild underweight), and a BMI z-score of −3 to a BMI of 14.7 in females (DSM-5: extreme underweight) and 15.9 in males (DSM-5: severe underweight).
2.3 Statistical analysis
All variables used in the study were examined for normality of distribution. For descriptive purposes, means of all variables used in the study were calculated per gender and differences between genders were tested with t-tests. To answer the study questions, (multiple) linear regression models were used to predict T5 (age 22) eating pathology (EDDS standardized composite score) by the following variables: (a) T1 (age 11) SPPC global self-esteem; (b) T1 SPPC global self-esteem and specific self–perception scores; (c) T2 (age 13) peer status nominations, including quadratic terms to assess a U-shaped relation; and (d) T1 SPPC self-esteem measures and T2 peer status nominations combined. Gender and T1 and/or T2 eating pathology proxy measures were treated as covariates to correct for potential confounding in all regression analyses. To examine if gender moderated the results (e.g., Micali et al., 2015), we added an interaction term for each predictor variable (predictor X gender), and tested whether this significantly increased the explained variance by means of an F-test. When the F-test was nonsignificant, the interaction term was dropped. The significance threshold was set at 0.05.
3 RESULTS
3.1 Descriptive statistics
Table 2 shows descriptive statistics of the variables used in this study for females and males. At T5 (age 22) the mean standardized eating pathology composite score was 11.25 (SD = 13.34), with a minimum of 0 and a maximum of 73.93. Females had significantly higher T5 eating pathology scores than men. At T5, 29.4% of the subjects reported eating unusually large amounts of food, of whom 33.0% (9.7% of total) experienced a loss of control; 12.6% reported some form of compensatory behavior (vomiting, using laxatives or diuretics, fasting, or engaging in excessive exercise) to prevent weight gain or counteract effects of overeating on average once a week or more over the past 3 months. At T5, 0.7% of the subjects had a BMI < 17.5, 3.3% a BMI < 18.5, 26.3% a BMI ≥ 25.0, and 6.7% a BMI ≥ 30.0.
| Females | Males | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | Difference | |
| Variables | n = 423a | n = 309a | t-test (two-sided p-value) |
| Age | |||
| T1 | 11.08 (0.57) | 11.10 (0.57) | −0.268 (.789) |
| T2 | 13.46 (0.54) | 13.48 (0.50) | −0.398 (.691) |
| T5 | 22.16 (0.65) | 22.30 (0.63) | −2.788 (.005) |
| BMIb | |||
| T1 | −0.00 (1.04) | −0.07 (1.07) | 0.838 (.402) |
| T2 | −0.18 (1.02) | −0.33 (1.10) | 1.893 (.059) |
| T5 | 23.86 (4.70) | 23.31 (3.24) | 1.878 (.061) |
| Self-esteem at age 11c | |||
| Social acceptance | 3.10 (0.57) | 3.11 (0.54) | −0.234 (.815) |
| Physical appearance | 3.06 (0.63) | 3.24 (0.57) | −3.908 (<.001) |
| Academic competence | 2.90 (0.49) | 2.97 (0.51) | −1.834 (.067) |
| Global self-esteem | 3.34 (0.53) | 3.40 (0.49) | −1.753 (.080) |
| Peer status at age 13d | |||
| Likeability | 0.56 (0.20) | 0.56 (0.20) | 0.525 (.600) |
| Physical attractiveness | 0.27 (0.23) | 0.12 (0.14) | 10.784 (<.001) |
| Academic performance | 0.34 (0.26) | 0.31 (0.26) | 1.861 (.063) |
| Popularity | 0.10 (0.12) | 0.09 (0.13) | 0.770 (.441) |
| Eating pathologye | |||
| T5 | 14.84 (15.01) | 6.35 (8.48) | 9.706 (p < .001) |
- a Note N for those with complete data on self-esteem, peer status, and eating pathology variables. For T1 BMI: female n = 417, male n = 303; for T2 BMI: female n = 409, male n = 301. For T1 Eating problems: female n = 420, male n = 305; for T2 Eating problems: female n = 416, male n = 300. All other variables: female n = 423, male n = 309.
- b BMI: T1 and T2: z-score standardized for age according to WHO growth reference data for 5 to 19-year olds (de Onis et al., 2007; WHO, 2007); T5: absolute BMI (kg/m2).
- c Self-esteem: Self-Perception Profile for Children (SPPC, Harter, 1982); scores could range between 1 (low self-esteem) and 4 (high self-esteem).
- d Peer status: number of received nominations by classmates divided by total number of classmates; scores could range between 0 (no nominations) and 1 (nominated by all classmates).
- e Eating pathology: T5 standardized composite sum score of the Eating Disorder Diagnostic Scale (EDDS, Krabbenborg et al., 2012; Stice et al., 2000). Sum scores could range between 0 and 100.
Females displayed lower self-esteem regarding physical appearance, but were more often nominated for physical attractiveness by their classmates than males.
3.1.1 Comparison of T1 and T2 eating and weight problems and T5 eating pathology
The T1 and T2 variables overweight combined with vomiting and distorted body image were included in the study to correct the analyses on T5 eating pathology and T1 self-perceptions and T2 peer nominations for potential confounding by T1 and/or T2 eating pathology. A distorted body image (self-perceived overweight when underweight) was found in two subjects at T1 (age 11) and in four other subjects at T2 (age 13). At ages 11 and 13 no subjects displayed perceived overweight in combination with vomiting. EDDS eating pathology scores at T5 (age 22) were significantly elevated in the two 11-year olds with distorted body image (M = 34.35, SD = 16.75) compared to those without (M = 11.24, SD = 13.36); t(713)=2.442, p = .015. No significant difference in T5 EDDS score was found between the four 13-year olds with distorted body image (M = 13.60, SD = 7.12) compared to those without (M = 11.03, SD = 13.23); t(705)=0.387, p = .699. T1 and T2 distorted body image (yes/no) was included as a covariate in the regression analyses.
3.2 Prediction of eating pathology
Table 3 shows the results of standardized regression analyses for the prediction of T5 eating pathology by the four self-esteem domains and the four peer-status domains, corrected for main effects of gender (significant in all models) and T1/T2 distorted body image. In preliminary analyses no interaction effects of gender with any of the predictors were found, and thus the interaction terms were dropped.
| Prediction of T5 eating pathologya | Unstandardized coefficient B | 95% confidence interval for B | Standardized coefficient β | t-test (two-sided p-value) | R2 |
|---|---|---|---|---|---|
|
Prediction by T1 global self-esteemb (model F(3, 711) = 30.134, p < .001) |
|||||
| T1 Global self-esteem | −2.232 | −4.069; –0.394 | −0.084 | −2.384 (.017) | .113 |
|
Prediction by T1 global and specific self-esteem domainsb (model F(6, 708) = 16.919, p < .001) |
|||||
| T1 social acceptance | −1.192 | −3.065; 0.680 | −0.049 | −1.250 (.212) | .125 |
| T1 physical appearance | −3.305 | −5.527; –1.082 | −0.149 | −2.919 (.004) | |
| T1 academic performance | 0.126 | −1.839; 2.090 | 0.005 | 0.125 (.900) | |
| T1 global self-esteem | 1.059 | −1.720; 3.839 | 0.040 | 0.748 (.455) | |
|
Prediction by T2 peer status domainsc (model (F(6, 700) = 15.121, p < .001) |
|||||
| T2 Likeability | 6.371 | 0.969; 11.773 | 0.095 | 2.315 (.021) | .115 |
| T2 Physical attractiveness | −5.789 | −11.915; 0.337 | −0.092 | −1.885 (.064) | |
| T2 Academic performance | 1.002 | −2.539; 4.544 | 0.020 | 0.556 (.579) | |
| T2 Popularity | −8.930 | −17.650; –0.211 | −0.084 | −2.011 (.045) | |
|
Prediction by combination of T1 Self-esteem domains and T2 peer status domainsd (model F(11, 680)=10.216, p<.001) |
|||||
| T1 Social acceptance | −0.546 | −2.525; 1.433 | −0.023 | −0.541 (.588) | .142 |
| T1 Physical appearance | −3.065 | −5.323; –0.807 | −0.138 | −2.665 (.008) | |
| T1 Academic performance | 0.136 | −1.894; 2.167 | 0.005 | 0.132 (.895) | |
| T1 Global self-esteem | 0.215 | −2.561; 2.990 | 0.008 | 0.152 (.879) | |
| T2 Likeability | 5.609 | 0.062; 11.156 | 0.083 | 1.986 (.047) | |
| T2 Physical attractiveness | −5.251 | −11.426; 0.924 | −0.083 | −1.670 (.095) | |
| T2 Academic performance | 1.780 | −1.859; 5.419 | 0.036 | 0.961 (.337) | |
| T2 Popularity | −10.788 | −19.565; –2.011 | −0.101 | −2.413 (.016) | |
- a T5 eating pathology: standardized composite sum score of the Eating Disorder Diagnostic Scale (EDDS, Krabbenborg et al., 2012; Stice et al., 2000). Bold: p < .05Mean ages: T1 11.01 years, T2 12.38 years, T5 21.03 years.
- b T1 self-esteem and self-perception scales: Self-Perception Profile for Children (SPPC, Harter, 1982); model corrected for gender and T1 distorted body image effects.
- c T2 Peer status: number of received nominations by classmates divided by total number of classmates; model corrected for gender and T2 distorted body image effects.
- d Variables see above; model corrected for gender, and for T1 and T2 distorted body image effects.
In the first model, global self-esteem at age 11 (T1) was a significant predictor with a negative relationship to eating pathology at age 22 (T5) after correcting for gender and T1 distorted body image effects. One SD increase in T1 global self-esteem decreased the T5 eating pathology score by 2.2 points.
In the second model, combining SPPC domains of self-esteem at age 11 (T1), self-esteem regarding physical appearance was a significant predictor, with a negative relationship to eating pathology at age 22 (T5) after correcting for gender and T1 body image distortion effects. One SD increase in T1 self-esteem regarding physical appearance decreased the T5 eating pathology score by 3.3 points. The other domains of self-esteem at age 11 in the model, including global self-esteem, did not have significant predictive value regarding eating pathology at age 22.
In the third model, combining domains of peer status at age 13 (T2), peer likeability was a significant predictor with a positive relationship to eating pathology at age 22 (T5), and peer popularity was a significant predictor with a negative relationship to T5 eating pathology, after correcting for gender and for T2 body image distortion effects. One SD increase in T2 peer likeability increased the T5 eating pathology score by 6.4 points, and one SD increase in T2 peer popularity decreased the T5 eating pathology score by 8.9 points. The other domains of peer status at age 13 in the model did not have significant predictive value regarding eating pathology at age 22. No evidence was found for a U-shaped relation and quadratic terms were dropped.
In the final model, combining all T1 self-esteem and T2 peer status domains, self-esteem regarding physical appearance at age 11 and peer popularity at age 13 were significant predictors with a negative relationship to eating pathology at age 22 (T5), while peer likeability at age 13 was positively related to T5 eating pathology, after correcting for effects of gender and distorted body image at ages 11 and 13. T5 eating pathology scores decreased by 3.1 points with one SD increase in T1 self-esteem regarding physical appearance, and by 10.8 points with one SD increase in T2 peer popularity, and it increased by 5.6 points with one SD increase in T2 peer likeability. The other domains of self-esteem at age 11 and of peer status at age 13 in the combined model did not have significant predictive value regarding eating pathology at age 22.
4 DISCUSSION
This study investigated whether self-esteem and peer status domains in early adolescence—self-esteem at age 11 and peer status at age 13—are associated with the level of eating pathology in young adulthood (age 22). Data were drawn from a cohort study which follows a large community sample from early adolescence into adulthood. We hypothesized that low global self-esteem and low self-perceptions and peer perceptions in the domains of social standing, academic competence, and physical attractiveness in early adolescence would predict eating pathology in early adulthood. Both low and high popularity are inherently stressful and adolescents at both ends of the popularity continuum may be vulnerable for developing eating pathology; thus a U-shaped relation between peer-perceived popularity and eating pathology was expected.
In a model combining measures of self-esteem assessed at age 11 and of peer-status assessed at age 13, controlling for gender and for distorted body image at ages 11 and 13, we found that self-perceived physical appearance at age 11 and peer-perceived likeability and popularity at age 13 were related to eating pathology at 22 years. The significant unstandardized regression coefficients in the combined model are of considerable size (between −10.79 and +5.61) with regard to the mean eating pathology score of 11.25 at age 22. Thus, self-perception of physical appearance at age 11 and peer popularity at age 13 one SD or more below average, and peer likeability at age 13 one SD or more above average could relate to an EDDS score at age 22 above the cut-off of 16.5 reported by Krabbenborg et al. (2012). However, whether this cut-off score can be generalized to our findings is not certain: in our general population cohort study an average EDDS standardized composite score of 11.25 (SD =13.34) was found (n = 732), whereas Krabbenborg et al. (2012) reported an average EDDS standardized composite score of 7.24 (SD =6.63) for their nonclinical female sample, selected for absence of eating disorder diagnoses (n = 45).
In the combined model low global self-esteem, self- or peer-perceived academic competence, self-perceived social acceptance, or peer-perceived physical attractiveness did not predict early adulthood eating pathology. A significant relationship between low global self-esteem at age 11 and eating pathology at age 22 that was found when analyzed separately disappeared when combined with other, specific T1 self-esteem variables.
The specific self-esteem variable of self-perceived physical appearance at age 11 did emerge as one of the significant predictors. Negative body image is a very potent, well-supported risk factor for eating disorders (Jacobi et al., 2004), specifically for bulimic pathology (Stice, 2002, 2016). Risk factor research on eating disorders in relation to adolescence has a long tradition, e.g., Gralen, Levine, Smolak, & Murnen (1990) reported that in girls the nature of predictors of dieting and disordered eating shifted between 6th and 10th grade from concrete events (e.g., dating) to more abstract cognitions (e.g., body image). It is not surprising then that low self-esteem regarding physical appearance at age 11 poses a risk for the development of eating pathology. In a more extreme form this constitutes one of the core features of the eating disorders anorexia nervosa and bulimia nervosa: an overvaluation of weight and body shape, and a sense of self-esteem that is mainly—if not entirely—determined by weight and shape (Fairburn & Harrison, 2003). Although binge eating disorder is not by definition characterized by an overvaluation of weight and body shape, the shame and suffering from the binge eating episodes, and the often concordant obesity also pose a serious threat to the self-perceived physical attractiveness of adolescents with this disorder.
For global self-esteem the disappearing effect when combined with specific self-perception measures indicates that specific measures, in particular self-perceived physical appearance, may be more relevant to the prediction of eating pathology than a global measure of self-esteem. Seemingly contradictory results of previous self-esteem studies could be related to differences between these studies in the type of self-esteem measured. Even within specific scales items may map onto different self-esteem concepts. For example, within the SPPC domain of physical appearance there is a combination of appearance-related self-esteem (How happy are you with your looks?) and self-rated physical attractiveness (How attractive are you?), which are not identical concepts (Feingold, 1992). Our findings regarding the relevance of using specific over general measures of self-esteem in eating disorder research need to be confirmed in future studies. In doing so, it is important to carefully choose and evaluate the measurement instruments against concepts of self-esteem.
Low peer popularity at age 13 predicted eating pathology at age 22. Other studies found that higher peer popularity was associated with more dieting behaviors cross-sectionally (Wang et al., 2006) and with more negative body-related cognitions one year later (Rancourt & Prinstein, 2010). However, they did not measure eating pathology as such. We did not find evidence for a curvilinear relation between high peer popularity and eating pathology, and thus our hypothesis on this was not confirmed.
Contrary to our expectations, adolescents who were well-liked by their classmates at age 13 showed higher levels of eating pathology at age 22. Only one other study (Lieberman et al., 2001) found that well-liked adolescent girls displayed more disordered eating behaviors and had lower body esteem than less-liked ones. The authors argued that girls who are well-liked might achieve high social acceptance because they rely heavily on the opinions of peers for their own self-esteem and will go at length to be accepted. Girls whose self-esteem is dependent on other people's judgements, either real or perceived, will actively conform to peer-group values and expectations—the thin-body ideal—which may lead to body dissatisfaction and disordered eating behaviors (Fairweather-Schmidt & Wade, 2016; Ferreira, Marta-Simões, & Trindade, 2016; Lieberman et al., 2001). The thin-body ideal may be transmitted in a peer group through so-called ‘fat talk’. Engaging in fat talk is associated with both higher social acceptance—provided the peer-group norm is pro-fat talk—and increased correlates of disordered eating (Cruwys, Leverington, & Sheldon, 2016). Whether this process underlies the relationship between social acceptance and eating pathology in our study is a question for future research. Another question is whether high social acceptance is a risk factor for eating pathology per se or reflects an underlying (personality) characteristic associated with increased risk, such as high interpersonal sensitivity (Arcelus, Haslam, Farrow, & Meyer, 2013), socially prescribed perfectionism (Bardone-Cone et al., 2007), or externalized self-perceptions and self-esteem (Lieberman et al., 2001).
Our results indicate the value of combining in one design measures of self-esteem and peer status in studies on (early) adolescents who are in a developmental phase where social comparison is important. Taken together our findings sketch the image of an adolescent who is insecure or negative about her (or his) looks and is trying to please peers, for which she/he finds confirmation in lower popularity (not being seen by peers as influential and as a person of power they want to be associated with). This in turn may reinforce negative self-evaluations, creating a loop that could culminate in eating pathology—as we investigated—or in other mental health problems.
4.1 Strengths and limitations
To our knowledge, this is the first study on eating pathology examining the respective roles of self-esteem and two distinct forms of peer status (popularity and acceptance) simultaneously. Strengths of this study include its longitudinal and community-based design, a sample including both male and female adolescents, and a long follow-up period, stretching eleven years from early adolescence to young adulthood. Response rates remained relatively high throughout the subsequent assessment waves. Data before the peak age of incidence of eating disorders (Smink et al., 2012) were available, allowing us to make inferences on risk factors for eating pathology. Moreover, not only self-report data were used, but also objective measures, such as length and weight, and data from other informants (parents and peers). This is considered an important advance in eating disorder research (Stice, South, & Shaw, 2012).
To our knowledge, this is the first study that examined the role of peer status regarding physical attractiveness in the development of eating pathology. Studies using older samples of adolescent females (Colabianchi, Ievers-Landis, & Borawski, 2006) or female college students (Davis, Claridge, & Fox, 2000; Davis, Shuster, Dionne, & Claridge, 2001) found that higher objective ratings of physical attractiveness were correlated with higher levels of weight preoccupation cross-sectionally. Davis et al. (2000, 2001) used a narrow definition of physical attractiveness, exclusively rating facial attractiveness and not other factors such as weight, clothes or accessories; factors that may be of importance in peers’ judgements about attractiveness (Ashmore, Solomon, & Longo, 1996). In our study physical attractiveness was judged in a non-exclusive fashion. Also our nominations were provided by an average of seventeen classmates, while this was done by only one research assistant in two of the other studies (Colabianchi et al., 2006; Davis et al., 2000). Peer-group judgements of physical attractiveness reflect the daily social environment, which may be associated with other outcomes than fragmentary assessments by research assistants. Thus, the measure of peer-nominations for physical attractiveness we used probably increases reliability of the judgement.
There are several limitations to consider. The first concerns the fact that self-esteem and peer status measures were not assessed at the same measurement moment but two years apart. This hampers the possibility to draw conclusions on the temporal sequence of the influence of self- versus peer-perceptions during adolescence on young adult eating pathology. Thus we advise to include both types of measures simultaneously in future longitudinal studies, at least in adolescence.
A second limitation is a possible selection bias of the study sample compared to the rest of the total TRAILS cohort, namely those with peer nominations who had complete T1 self-esteem and T5 eating pathology data. The study sample had significantly higher (more positive) scores on almost all predictor variables, with the exception of appearance-related self-esteem and being liked by peers, which showed no difference, and peer popularity, which was lower in our sample. Differences in actual scores were small. Eating pathology scores at age 22 were significantly higher (on average 2 points) in the study sample, with large standard deviations. The observations on peer status data were restricted to those TRAILS participants with T2 peer nominations (n = 1,007) and thus the ‘remainder’ group with missing data was relatively small with regard to the other comparisons. Selective attrition of putative at-risk adolescents may have caused a restriction of range in specific self-esteem and peer-status variables, which in turn could have reduced the power to detect a significant correlation between those domains and later eating pathology. The main reduction of the sample, however, is attributable to the lack of peer nominations in the overarching study, which occurred because only classes with at least three TRAILS participants were included. This in itself is not expected to create bias relevant for our study. Differences in predictor variables between the study sample and the remainder of the TRAILS cohort are rather small (between 0.33% and 1.33% with regard to the maximum T1 self-esteem domain scores; T2 differences range between 4% and 8% but relate to the subsample with peer status data only). Thus, the consequences of selection bias are probably limited.
Third, since no T1 and T2 measures of eating pathology were available, we used combinations of YSR and CBCL items with BMI data as a proxy for the core features of eating pathology: compensatory behaviors and distorted body image. These indicators are narrow and thus probably under inclusive. Only six subjects scored positive for distorted body image at age 11 or 13.
A final limitation lies in the use of the (standardized) symptom composite score of the EDDS. This has the advantage of increased power over categorical outcomes (e.g., eating disorder diagnoses) but a drawback of this approach is that we cannot differentiate between eating disorder diagnoses, which may have different risk profiles. We believe that this might especially pertain to peer status. Though interpersonal difficulties are common in all eating disorders, specific patterns per eating disorder are discernable. For example, patients with restrictive eating pathology tend to avoid conflict, while patients with binge/purge pathology are more prone to conflict (Arcelus et al., 2013). These specific characteristics associated with different types of eating pathology might influence peer status differentially. Although the specific eating disorders may have specific risk factors, we consider the use of a general eating pathology outcome measure valid in the light of a transdiagnostic approach of eating disorders, which states that eating disorders share the same psychopathology, that is: an overvaluation of weight and shape (Fairburn & Cooper, 2011). Furthermore, eating pathology is a continuous construct; by using eating disorder diagnoses only, mild—but relevant—forms of eating pathology would be excluded in the analyses.
4.2 Conclusion
Negative evaluations of one's physical appearance at age 11, and being liked and not being popular in the eyes of peers at age 13 are associated with increased eating pathology at age 22.
ACKNOWLEDGEMENTS
The authors thank D. Raven (M.Sc.) for help with data management. This research is part of the TRacking Adolescents’ Individual Lives Survey (TRAILS). Participating centers of TRAILS include various departments of the University Medical Center Groningen and University of Groningen, the University of Utrecht, the Radboud Medical Center Nijmegen, and Parnassia Psychiatric Institute, all in the Netherlands. They are grateful to all adolescents, their parents, and teachers who participated in this research, and to everyone who worked on this project and made it possible.
CONFLICT OF INTEREST
None.