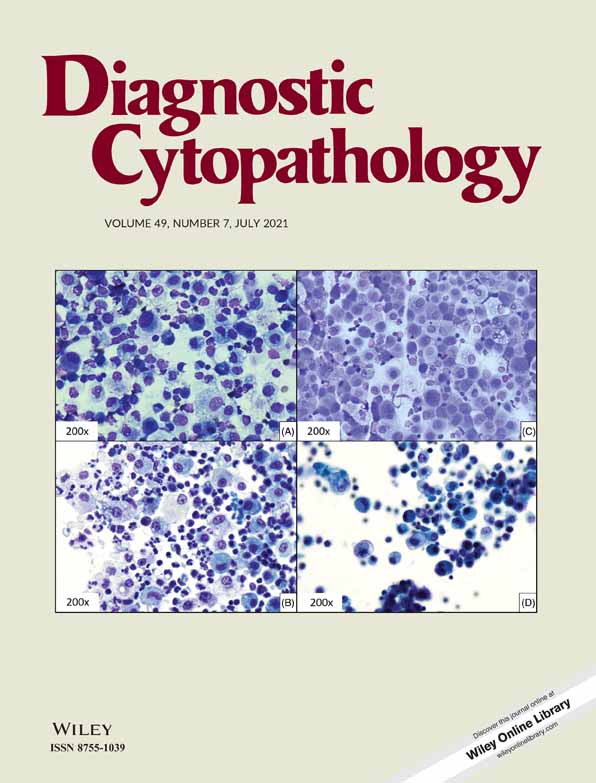
Cytomorphometry and morphology analysis of human papillomavirus type 16 in liquid-based cervical cytology samples
Abstract
Background
Human papillomavirus (HPV) is the main causal factor of cervical carcinoma. HPV 16 is one of the most prominent oncogenic types. We aimed to evaluate the cytomorphometric and morphological alterations caused by HPV 16 in liquid-based cytology (LBC).
Methods
The Cobas 4800 HPV system was used for the detecting and typing HPV DNA in cervical specimens. In this study, 30 HPV 16 positive and 30 HPV 16 negative cervical samples were evaluated for micronuclei (MN), nonclassical cytologic abnormalities, and the nuclear-to-cytoplasmic ratio. Nuclear and cellular areas were evaluated using image analysis software and the nuclear-to-cytoplasm ratio was calculated. All analyses were performed blinded to the patients' HPV status. Statistical evaluation was carried out using the χ2 and Fisher test; P-values < .05 were considered significant.
Results
The frequencies of micronucleated cells and koilocytes were higher in the HPV 16 infected group (P < .05). Cells with perinuclear halo in control group were higher than the HPV 16 infected group (P < .05). The mean nuclear-to-cytoplasm ratio in HPV 16 patients was higher than the control value, but the difference was not statistically significant.
Conclusion
LBC can be used to detect morphological and morphometric changes. HPV 16 induces the formation of MN and koilocytosis. The evaluation of MN could provide additional information in monitoring genomic instability and of koilocytes could provide information about damage to the cytoskeleton filaments in HPV infection. Further studies are needed to investigate the effects of HPV-18 and other high-risk HPV types on the cell size and nucleus-to-cytoplasm ratio.
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared.