Physical multimorbidity and depression: A mediation analysis of influential factors among 34,129 adults aged ≥50 years from low- and middle-income countries
Abstract
Background
There is a scarcity of literature on the association between physical multimorbidity (i.e., ≥2 chronic physical conditions) and depression among older adults, especially from low- and middle-income countries (LMICs). In addition, the mediators in this association are largely unknown. Therefore, we aimed to examine this association among adults aged ≥50 years from six LMICs (China, Ghana, India, Mexico, Russia, and South Africa), and to identify potential mediators.
Methods
Cross-sectional, nationally representative data from the Study on Global Ageing and Adult Health were analyzed. Depression was defined as past-12 months DSM-IV depression or receiving depression treatment in the last 12 months. Information on 11 chronic physical conditions were obtained. Multivariable logistic regression and mediation analyses were conducted.
Results
Data on 34,129 individuals aged ≥50 years were analyzed [mean (SD) age 62.4 (16.0) years; maximum 114 years; 52.1% females]. Compared to no chronic conditions, 2, 3, 4, and ≥5 chronic conditions were associated with 2.55 (95% CI = 1.90–3.42), 3.12 (95% CI = 2.25–4.34), 5.68 (95% CI = 4.02–8.03), and 8.39 (95% CI = 5.87–12.00) times higher odds for depression. Pain/discomfort (% mediated 39.0%), sleep/energy (33.2%), mobility (27.5%), cognition (13.8%), perceived stress (7.3%), disability (6.7%), loneliness (5.5%), and food insecurity (1.5%) were found to be significant mediators in the association between physical multimorbidity and depression.
Conclusions
Older adults with physical multimorbidity are at increased odds of depression in LMICs. Future studies should assess whether addressing the identified potential mediators in people with physical multimorbidity can lead to reduction in depression in this population.
1 INTRODUCTION
Approximately 3.8% of the global population is affected by depression, with this figure being 5.7% among adults older than 60 years (World Health Organization, 2021). Moreover, more than 80% of the depression burden is among people living in low- and middle-income countries (LMICs) (CORDIS| European Commission, 2021). Although there are effective treatments for mental disorders, more than 75% of people in LMICs receive no treatment (Evans-Lacko et al., 2018). In addition, late-life depression is an important issue due to rapid aging occurring particularly in LMICs, and the fact that late-life depression is associated with greater risk of morbidity, suicide, increased use of hospital and outpatient medical services, and worse quality of life (Blazer, 2003). Given the high prevalence of late-life depression and its associated negative health outcomes, and the limited availability of treatment especially in LMICs, it is important to identify risk factors of late-life depression in LMICs to inform targeted interventions.
One potentially important but understudied risk factor is that of physical multimorbidity, which may be defined as the presence of two or more long-term physical health conditions (NICE| The National Institute for Health and Care Excellence, 2018). Physical multimorbidity is highly prevalent in older people (Divo et al., 2014) and this is likely to be increasing in LMICs due to changes in lifestyle and urbanization. Physical multimorbidity can feasibly be associated with depression via factors such as lower levels of physical activity, loneliness, suffering due to symptoms (e.g., disability, pain, and mobility limitations), poverty, or inflammation (Lee & Giuliani, 2019; Schuch et al., 2017). However, while there are some studies on physical multimorbidity and depression, most of the studies have been conducted in single high-income countries, and community-based studies focusing on the older population of LMICs are scarce, while there are no multi-country studies from LMICs which have focused solely on the older population (Read et al., 2017). The previous multi-country studies on this topic from LMICs focused on all individuals aged ≥18 years, despite the fact that multimorbidity is much more highly prevalent in the older population, and did not conduct analyses to identify the factors that can potentially mediate the association between physical multimorbidity and depression (Arokiasamy et al., 2015; Moussavi et al., 2007; Stubbs et al., 2017). It is important to identify potential mediators as such factors can provide information for targeted interventions to reduce depression among those with physical multimorbidity.
Given this background, the aim of this study was to examine the association between physical multimorbidity and depression, as well as the potential mediators in this association, in a sample of 34,129 individuals aged ≥50 years from China, Ghana, India, Mexico, Russia, and South Africa. We hypothesized that those with physical multimorbidity will be at a significantly higher odds of depression compared to those without multimorbidity. We further hypothesized that unemployment, food insecurity, wealth quintiles, cognition, perceived stress, sleep/energy, pain/discomfort, mobility, physical activity, disability, loneliness, and social participation may be potential mediators in the physical multimorbidity/depression relationship.
2 METHODS
Data from the Study on Global Ageing and Adult Health (SAGE) were analyzed. Details of the survey (including the sampling procedure) can be found elsewhere (He et al., 2012; Kowal et al., 2012). Briefly, this survey was undertaken in China, Ghana, India, Mexico, Russia, and South Africa between 2007 and 2010. These countries broadly represent different geographical locations and levels of socioeconomic and demographic transition. Based on the World Bank classification at the time of the survey, Ghana was the only low-income country, and China and India were lower middle-income countries although China became an upper middle-income country in 2010. The remaining countries were upper middle-income countries. To obtain nationally representative samples, a multistage clustered sampling design method was used. The sample consisted of adults aged ≥18 years with oversampling of those aged ≥50 years. Trained interviewers conducted face-to-face interviews using a standard questionnaire. Standard translation procedures were undertaken to ensure comparability between countries. The survey response rates were: China 93%; Ghana 81%; India 68%; Mexico 53%; Russia 83%; and South Africa 75%. Sampling weights were constructed to adjust for the population structure as reported by the United Nations Statistical Division. Ethical approval was obtained from the WHO Ethical Review Committee and local ethics research review boards. Written informed consent was obtained from all participants.
2.1 Depression
Questions based on the World Mental Health Survey version of the Composite International Diagnostic Interview (Kessler & Üstün, 2004) were used for the endorsement of past 12-month DSM-IV depression using the same algorithm used in previous studies using the same data set (Garin et al., 2016; Koyanagi et al., 2014) (details provided in Table S1). Individuals who reported to have received treatment for depression in the past 12 months were also considered to have depression.
2.2 Chronic physical conditions and physical multimorbidity
We included all 11 chronic physical conditions (angina, arthritis, asthma, chronic back pain, chronic lung disease, diabetes, edentulism, hearing problems, hypertension, stroke, and visual impairment) for which data were available in the SAGE. Chronic back pain was defined as having had back pain every day during the last 30 days. Respondents who answered affirmatively to the question “Have you lost all of your natural teeth?” were considered to have edentulism. The participant was considered to have hearing problems if the interviewer observed this condition during the survey. Hypertension was defined as having at least one of the following: systolic blood pressure ≥140 mmHg; diastolic blood pressure ≥90 mmHg; or self-reported diagnosis. Visual impairment was defined as having severe/extreme difficulty in seeing and recognizing a person that the participant knows across the road (Freeman et al., 2013). Diabetes and stroke were solely based on lifetime self-reported diagnosis. For other conditions, the participant was considered to have the condition in the presence of either one of the following: self-reported diagnosis; or symptom-based diagnosis based on algorithms. We used these algorithms, which have been used in previous studies using the same data set, to detect undiagnosed cases (Arokiasamy et al., 2017; Garin et al., 2016). Specifically, the validated Rose questionnaire was used for angina (Rose, 1962), and other previously validated symptom-based algorithms were used for arthritis, asthma, and chronic lung disease (Arokiasamy et al., 2017). Further details on the definition of chronic physical conditions can be found in Table S2. Physical multimorbidity was defined as ≥2 chronic physical conditions, in line with previously used definitions (Garin et al., 2016).
2.3 Mediators
The potential mediators (i.e., unemployment [engaged in paid work ≥2 days in last 7 days: Y/N], food insecurity, wealth quintiles based in country-specific income, cognition, perceived stress, sleep/energy, pain/discomfort, mobility, physical activity, disability, loneliness, social participation) were selected based on previous literature suggesting the possibility that they can be the result of physical multimorbidity, and a cause of depression (Baghaei et al., 2021; Friedland & McColl, 1992; Gan et al., 2016; Hoebel et al., 2017; Mikkelsen et al., 2010; Nakad et al., 2020; Pathirana & Jackson, 2018; Robb et al., 2020; Schuch et al., 2017; Sheng et al., 2017; Sindi et al., 2020; Stickley et al., 2019; Vancampfort et al., 2017; Wiegner et al., 2015).
Although physical activity may also be conceptualized as a confounder, since our measure of physical activity was on current levels of physical activity, which is highly likely to be influenced by symptoms or sequalae of physical diseases, we considered this to be a mediator in our study. Food insecurity was defined with the use of the two following questions: “In the last 12 months, how often did you ever eat less than you felt you should because there wasn't enough food?” and “In the last 12 months, were you ever hungry, but didn't eat because you couldn't afford enough food?” Both questions had as answer options: every month (coded = 1); almost every month (coded = 2); some months, but not every month (coded = 3); only in 1 or 2 months (coded = 4); never (coded = 5). Those who answered 5 to both items were categorized as food secure, while others were food insecure (Schrock et al., 2017). Cognition, perceived stress, sleep/energy, pain/discomfort, and mobility were assessed with two questions each. The actual questions can be found in Table S3. Each item was scored on a five-point scale ranging from “none” to “extreme/cannot do” except for the two items on perceived stress which ranged from “never” to “very often.” For each separate health status, we used factor analysis with polychoric correlations to obtain a factor score which was later converted to scores ranging from 0 to 100 with higher values representing worse health function (Schrock et al., 2017). Level of physical activity was assessed with the Global Physical Activity Questionnaire (Bull et al., 2009). Those scoring <150 min/week were classified as having low levels of physical activity (World Health Organization, 2010). Disability was assessed with six questions on the level of difficulty in conducting standard basic activities of daily living (ADL) in the past 30 days (washing whole body, getting dressed, moving around inside home, eating, getting up from lying down, and using the toilet). Those who answered severe or extreme/cannot do to any of the six questions were considered to have disability (Koyanagi et al., 2015). Loneliness was assessed with the question “Did you feel lonely for much of the day yesterday?” with answer options “yes” or “no.” Following a previous SAGE publication (Ma et al., 2021), a social participation scale was created based on nine questions on the participant's involvement in community activities in the past 12 months (e.g., attended religious services, club, society, union etc.) with answer options “never (coded = 1),” “once or twice per year (coded = 2),” “once or twice per month (coded = 3),” “once or twice per week (coded = 4),” and “daily (coded = 5).” The answers to these questions were summed and converted to a scale ranging from 0 to 100 with higher scores indicating higher levels of social participation.
2.4 Control variables
The selection of control variables was based on past literature and included age, sex, years of education received, marital status, and smoking (Arokiasamy et al., 2015).
2.5 Statistical analysis
The statistical analysis was done with Stata 14.2 (Stata Corp LP). The analysis was restricted to those aged ≥50 years. The difference in sample characteristics were tested by Chi-squared tests and Student's t-tests for categorical and continuous variables, respectively. Multivariable logistic regression analysis was conducted to assess the association between number of chronic conditions (exposure) and depression (outcome). These analyses were also stratified by age groups (i.e., 50–64, ≥65 years). Furthermore, test of trend was conducted by including the number of chronic conditions in the model as a continuous variable rather than a categorical variable. We also conducted analysis with the individual chronic conditions as the exposure variable including all 11 chronic conditions simultaneously in the model. To assess the between country-heterogeneity in the association between physical multimorbidity (i.e., ≥2 chronic conditions) and depression, we conducted country-wise analysis and calculated the Higgin's I2, which represents the degree of heterogeneity that is not explained by sampling error with values of 25%, 50%, and 75% often being considered as low, moderate, and high levels of heterogeneity (Higgins et al., 2003). An overall estimate was obtained based on country-wise estimates by meta-analysis with random effects.
Mediation analysis was conducted to gain an understanding of the extent to which various factors may explain the association between physical multimorbidity and depression in the overall sample and samples stratified by age groups. We used the khb (Karlson Holm Breen) command in Stata (Breen et al., 2013) for the mediation analysis. This method can be applied in logistic regression models and decomposes the total effect (i.e., unadjusted for the mediator) of a variable into direct (i.e., effect of multimorbidity on depression adjusted for the mediator) and indirect effects (i.e., mediational effect). Confidence intervals were calculated with the delta method. Using the khb command, the percentage of the main association explained by the mediator can also be calculated (mediated percentage). The mediated percentage is the percent attenuation in the log odds of physical multimorbidity after the inclusion of the potential mediator in the model, compared to the model without the mediator. Each potential mediator was included in the model individually.
All regression analyses including the mediation analysis were adjusted for age, sex, education, marital status, smoking, and country except for the country-stratified analyses which were not adjusted for country. Adjustment for country was done by including dummy variables for each country in the model as in previous SAGE publications (Koyanagi et al., 2014, 2018). The sample weighting and the complex study design were considered in all analyses. Results from the regression analyses are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The level of statistical significance was set at p < .05.
3 RESULTS
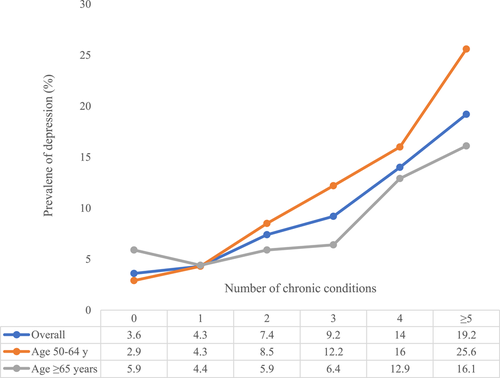
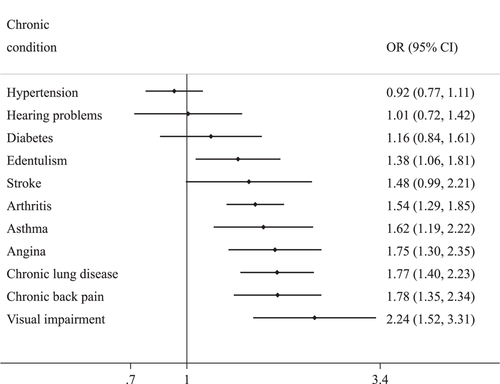
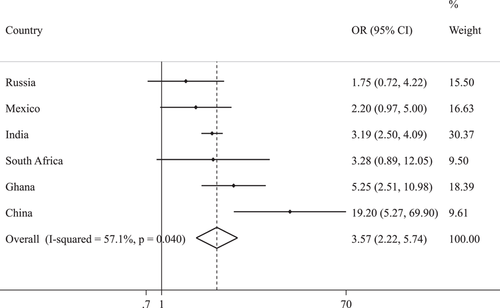
The sample included 34,129 individuals aged ≥50 years (China n = 13,175; Ghana n = 4305; India n = 6560; Mexico n = 2313; Russia n = 3938; South Africa n = 3838) with a mean (SD) age of 62.4 (16.0) years (maximum 114 years) and 52.1% were females. The prevalence of physical multimorbidity (i.e., ≥2 chronic conditions) and depression were 45.5% and 6.6%, respectively. The sample characteristics are shown in Table 1. Physical multimorbidity and depression were both associated with higher prevalence of female sex, marital status of separated/divorced/widowed, unemployment, food insecurity, lower levels of wealth, disability, and loneliness, while health status (i.e., cognition, perceived stress, sleep/energy, pain/discomfort, mobility) was also worse. The most highly prevalent pairs or chronic conditions were that of arthritis and hypertension (18.7%), and angina and hypertension (12.4%) (Figure S1). A linear increase in the prevalence of depression was observed with increasing number of chronic conditions for the overall sample and those aged 50–64 years (Figure 1). For those aged ≥65 years, the prevalence of depression increased sharply with 4 or more chronic conditions. In terms of individual chronic conditions, edentulism, arthritis, asthma, angina, chronic lung disease, chronic back pain, and visual impairment were associated with higher odds for depression (OR = 1.38–2.24) (Figure 2). In the overall sample, increasing number of chronic conditions was dose-dependently associated with higher odds for depression (Table 2). For example, ≥5 chronic conditions (vs. no conditions) was associated with 8.39 (95% CI = 5.87–12.00) higher odds for depression. Similar trends with higher ORs were found for those aged 50–64 years, but only ≥4 chronic conditions were significantly associated with depression among those aged ≥65 years. Country-wise analysis showed that there is a moderate level of heterogeneity (I2 = 57.1%) in the association between physical multimorbidity and depression with the overall estimate based on a meta-analysis being OR = 3.29 (95% CI = 2.66–4.07) (Figure 3). Mediation analysis showed that pain/discomfort (% mediated 39.0%), sleep/energy (33.2%), and mobility (27.5%) explained the largest proportion of the association between physical multimorbidity and depression, followed by cognition (13.8%), perceived stress (7.3%), disability (6.7%), loneliness (5.5%), and food insecurity (1.5%) in the overall sample (Table S4). Among those aged ≥65 years, the mediated percentage was much higher for all these mediators. For example, this figure was 65.5%, 48.3%, and 42.3% for pain/discomfort, sleep/energy, and mobility, respectively. Unemployment, wealth, physical activity, and social participation were not significant mediators.
| Multimorbidity | Depression | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Overall | No | Yes | p-value | No | Yes | p-value | |
| Age (years) | Mean (SD) | 62.4 (16.0) | 60.2 (14.3) | 65.0 (16.8) | <.001 | 62.3 (16.0) | 63.0 (15.5) | .131 |
| Sex | Female | 52.1 | 47.6 | 57.3 | <.001 | 51.5 | 60.4 | <.001 |
| Male | 47.9 | 52.4 | 42.7 | 48.5 | 39.6 | |||
| Education (years) | 6.0 (8.9) | 6.1 (9.1) | 5.9 (8.9) | .271 | 6.1 (8.9) | 3.8 (7.7) | <.001 | |
| Marital status | Married/cohabiting | 75.5 | 80.9 | 69.0 | <.001 | 76.1 | 68.8 | <.001 |
| Never married | 1.8 | 1.6 | 1.8 | 1.8 | 1.2 | |||
| Separated/divorced/widowed | 22.8 | 17.4 | 29.2 | 22.2 | 30.0 | |||
| Smoking | Never | 58.6 | 57.0 | 59.9 | <.001 | 59.3 | 48.3 | <.001 |
| Current | 34.9 | 37.7 | 32.1 | 34.2 | 44.4 | |||
| Past | 6.6 | 5.4 | 8.0 | 6.5 | 7.3 | |||
| Unemployed | No | 42.7 | 50.5 | 33.0 | <.001 | 43.3 | 33.7 | <.001 |
| Yes | 57.3 | 49.5 | 67.0 | 56.7 | 66.3 | |||
| Food insecurity | No | 88.2 | 89.8 | 85.9 | <.001 | 89.2 | 73.5 | <.001 |
| Yes | 11.8 | 10.2 | 14.1 | 10.8 | 26.5 | |||
| Wealth | Poorest | 17.1 | 16.2 | 18.3 | .005 | 16.6 | 23.4 | <.001 |
| Poorer | 19.0 | 18.2 | 19.9 | 18.8 | 22.1 | |||
| Middle | 19.5 | 19.1 | 19.7 | 19.5 | 19.5 | |||
| Richer | 21.3 | 21.5 | 21.0 | 21.5 | 19.9 | |||
| Richest | 23.1 | 25.1 | 21.0 | 23.7 | 15.1 | |||
| Cognitiona | Mean (SD) | 30.6 (46.1) | 25.3 (44.1) | 36.9 (46.7) | <.001 | 29.3 (45.5) | 49.1 (42.3) | <.001 |
| Perceived stressa | Mean (SD) | 40.1 (41.0) | 37.3 (40.8) | 43.7 (41.1) | <.001 | 39.1 (40.5) | 54.3 (40.0) | <.001 |
| Sleep/energya | Mean (SD) | 27.4 (45.2) | 20.0 (41.3) | 36.6 (45.4) | <.001 | 25.8 (44.2) | 50.3 (40.6) | <.001 |
| Pain/discomforta | Mean (SD) | 30.3 (44.9) | 22.4 (42.0) | 39.9 (43.5) | <.001 | 28.6 (44.0) | 53.8 (37.8) | <.001 |
| Mobilitya | Mean (SD) | 32.6 (46.6) | 23.7 (41.8) | 43.4 (45.9) | <.001 | 31.1 (45.7) | 54.0 (43.4) | <.001 |
| Low physical activity | No | 76.5 | 80.2 | 72.6 | <.001 | 76.7 | 73.6 | .109 |
| Yes | 23.5 | 19.8 | 27.4 | 23.3 | 26.4 | |||
| Disability | No | 92.9 | 97.3 | 87.5 | <.001 | 94.1 | 75.2 | <.001 |
| Yes | 7.1 | 2.7 | 12.5 | 5.9 | 24.8 | |||
| Loneliness | No | 88.7 | 91.9 | 84.6 | <.001 | 90.2 | 67.5 | <.001 |
| Yes | 11.3 | 8.1 | 15.4 | 9.8 | 32.5 | |||
| Social participationb | Mean (SD) | 21.3 (23.3) | 22.7 (23.7) | 20.2 (22.8) | <.001 | 21.5 (23.2) | 22.0 (23.6) | .548 |
- Note: Data are % unless otherwise stated. Multimorbidity referred to ≥2 chronic conditions. p-value was calculated by Chi-squared tests and Student's t-tests for categorical and continuous variables, respectively.
- a Based on a scale ranging from 0 to 100 with higher scores representing worse health status.
- b Based on a scale ranging from 0 to 100 with higher scores representing higher levels of social participation.
| Age | ||||||
|---|---|---|---|---|---|---|
| No. of chronic conditions | Overall | 50–64 years | ≥65 years | |||
| 0 | 1.00 | 1.00 | 1.00 | |||
| 1 | 1.50* | (1.15, 1.96) | 1.84* | (1.17, 2.91) | 0.92 | (0.50, 1.69) |
| 2 | 2.55** | (1.90, 3.42) | 3.46** | (2.11, 5.67) | 1.29 | (0.75, 2.20) |
| 3 | 3.12** | (2.25, 4.34) | 5.00** | (3.26, 7.67) | 1.31 | (0.70, 2.45) |
| 4 | 5.68** | (4.02, 8.03) | 6.49** | (4.03, 10.44) | 3.49** | (2.11, 5.76) |
| ≥5 | 8.39** | (5.87, 12.00) | 12.55** | (6.36, 24.77) | 4.30** | (2.39, 7.72) |
- Note: Data are odds ratio (95% confidence interval). Models are adjusted for age, sex, education, marital status, smoking, and country. All regressions showed significant test for trend (p < 0.001).
- * p < .01
- ** p < .001.
4 DISCUSSION
4.1 Main findings
In this large sample of middle-aged to older adults from six LMICs, physical multimorbidity was associated with a substantially increased odds for depression with the odds increasing in a dose-dependent manner with increasing number of physical diseases. Specifically, compared to no chronic conditions, 2, 3, 4, and ≥5 chronic conditions were associated with significant 2.55–8.39 times higher odds for depression in the overall sample. Similar trends were found for those aged 50–64 years, but only ≥4 chronic conditions were significantly associated with depression among those aged ≥65 years. Indicators of poverty had very little influence in the association between physical multimorbidity and depression, but factors such as pain/discomfort, sleep/energy, and mobility were identified as particularly important potential mediators. To the best of our knowledge, this is the first multi-country community-based study on this topic with a specific focus on older adults from LMICs, which has quantified the degree to which various potential mediators may explain the association between physical multimorbidity and depression.
4.2 Interpretation of the findings
The results of our study that physical multimorbidity was associated with higher odds for depression concur with those of previous studies from diverse settings and age groups (Barnett et al., 2012; Read et al., 2017). There are several plausible pathways that can explain the physical multimorbidity/depression relationship. First, the present study identified several individual chronic conditions that are associated with a significantly higher odds for depression (i.e., edentulism, arthritis, asthma, angina, chronic lung diseases, chronic back pain, and visual impairment). For example, arthritis, asthma, angina, and some forms of chronic low back pain are associated with low-grade inflammation (Kewalramani et al., 2008; Simmonds & Foxwell, 2008). There is now an extensive body of data showing that depression is associated with both a chronic low-grade inflammatory response, activation of cell-mediated immunity, and activation of the compensatory anti-inflammatory reflex system, characterized by negative immunoregulatory processes (Berk et al., 2013). Visual impairment may increase the risk for depression via its negative impact on daily and social activities (Ribeiro et al., 2015), while the link between edentulism and depression may be explained by its influence on facial appearance, nutritional intake, and the ability to eat, speak, and socialize (Tyrovolas et al., 2016). The cumulative effect of the individual chronic conditions may thus increase risk for depression in those with physical multimorbidity.
Importantly, this study identified several potential mediators in the physical multimorbidity/depression relationship, with pain/discomfort, sleep/energy, and mobility explaining the largest proportions. In physical multimorbidity, pain could be a result of a multitude of different health problems and their exacerbations (Scherer et al., 2016), while pain is linked to changes in the central nervous system (e.g., altered central processing), and this can subsequently increase risk of depression (Campbell et al., 2003). Next, physical multimorbidity may lead to sleep problems via pain and discomfort or the exacerbation of chronic conditions at night (Scherer et al., 2016), and in turn, sleep problems may lead to depression owing to sustained arousal and chronic activation or hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis, the major neuroendocrine mediator of stress response, that plays a vital role in the development of depression in insomniacs with objective short sleep duration (Li et al., 2016). Finally, people with physical multimorbidity are more likely to have mobility limitations as many diseases (e.g., arthritis, chronic back pain, angina, and stroke) are associated with symptoms (e.g., pain, paralysis in stroke, and difficulty breathing) that can lead to this condition. In turn, mobility limitations may lead to depression via increase in sedentary behavior (Lampinen & Heikkinen, 2003), and declines in quality of life and functional abilities (Musich et al., 2018).
Other factors that were identified as potential mediators but to a lesser degree include cognition, perceived stress, disability, and loneliness, with food insecurity explaining only a very small proportion. Physical multimorbidity may increase risk for cognitive impairment via factors such as microvascular changes, and inflammatory processes (Biessels et al., 2006; Jacob et al., 2019). Cognitive impairment could be a symptom of depression, but it is also possible for poor cognitive function to lead to depression via forgetfulness and reluctancy to participate in social activity. Next, physical multimorbidity can lead to high levels of stress via the symptoms of the chronic conditions (e.g., disability, mobility limitations, and pain), or the complications in treatment of multiple conditions (Stubbs et al., 2018). Perceived stress in turn can lead to depression through psychological pathways. For example, uncontrollable circumstances may create an event-specific perception of stress. These specific stresses could then accumulate into a generalized perception of stress that would affect depression levels through changes in global perceptions of control and associated negative emotional reactions (Ghorbani et al., 2008). The explanation behind disability is likely to be similar to that of mobility limitation mentioned above. People with physical multimorbidity may feel more lonely owing to feelings of inadequacy, dependency, and dejection and thus avoid social activities (Stickley & Koyanagi, 2018), while the link between loneliness and depression has been explained by low levels of social wellbeing and lack of a support system (Mushtaq et al., 2014). Interestingly, although previous studies have shown that multimorbidity can increase levels of poverty due to loss of jobs, or the high treatment costs associated with treating multiple conditions (Bähler et al., 2015), while poverty is known to be strongly associated with depression (Beckwith, 2020), potential indicators of poverty such as wealth, unemployment, and food insecurity had no or almost no influence in the association between physical multimorbidity and depression.
Finally, in our study, the association between physical multimorbidity and depression was more pronounced among those aged 50–64 years compared to older people, and among those ≥65 years, only ≥4 chronic conditions were significantly associated with depression. These findings may be explained by older adults being more accepting of multiple chronic conditions and perceiving this to be part of the normal aging process (Clarke & Bennett, 2013). However, in middle-aged people, multimorbidity may have a more profound impact on their lives for factors such shame for having chronic conditions when it is not very common among people of similar age, hopelessness relating to having have to live with physical diseases for a longer time, and dim future prospects.
4.3 Implications of the study findings
Findings from the present study suggest that targeting the identified potential mediators in older people with physical multimorbidity may reduce risk for depression, especially among people aged ≥65 years. While pharmacological interventions may be possible for factors such as sleep problems and pain, given that people with multimorbidity may already be taking multiple medications, nonpharmacological interventions may be more suitable if possible, and this may particularly be important in LMICs where medical resources may be limited. For example, promotion of physical activity has been shown to be feasible among people with chronic conditions, and may help in relieving pain, sleep problems, and mobility limitations (Hosseini et al., 2018; Kong et al., 2016; Raman et al., 2013; Verhey et al., 2020). There is a clear need to increase awareness of the importance of considering physical activity participation among health care workers in LMICs. For example, continued medical education should be used to inform health care providers on the importance of assessing physical activity levels and how cognitive-behavioral principles (e.g., goal setting, problem-solving etc.) can be employed to assist patients to increase physical activity levels (Vancampfort et al., 2017). Finally, the utilization of cognitive-behavioral therapy may also be beneficial for reliving stress and improving sleep among those with physical multimorbidity, and has been shown to be feasible in LMICs.
4.4 Strengths and limitations
The large sample size, the use of nationally representative datasets, and the identification of potential mediators in the association between physical multimorbidity and depression are the strengths of the present study. However, findings must be interpreted in light of the limitations of the study. First, the majority of the variables were based on self-report potentially introducing both social desirability and recall bias into the findings. Second, our list of chronic diseases included a variety of diseases which are highly prevalent in LMICs, but lacked some diseases (such as cancer), which are known to be related with higher risk of depression. Finally, temporal associations cannot be established in this study due to the cross-sectional design. For example, it is also possible for depression to precede physical multimorbidity, with this link being explained by unhealthy lifestyles. In relation to this, mediators and confounders cannot be distinguished on statistical grounds. Thus, it is possible for the mediated percentage calculated in our study to be an overestimate for the various ways in which physical multimorbidity, depression, and the mediators can be interrelated. Future studies of longitudinal design are therefore warranted for a further understanding on the role of the identified potential mediators in the association between physical multimorbidity and depression.
5 CONCLUSION
Physical multimorbidity was associated with substantially increased odds for depression among older adults in LMICs. Factors such as pain/discomfort, sleep/energy, and mobility may be important mediators in this association. Future longitudinal and intervention studies are needed to assess temporal associations and the effect of addressing the potential mediators identified in our study on depression in people with multimorbidity among older people in LMICs.
ACKNOWLEDGMENTS
This study uses data from WHO's Study on Global Ageing and Adult Health (SAGE). SAGE is supported by the U.S. National Institute on Aging through Interagency Agreements OGHA 04034785, YA1323–08-CN-0020, Y1-AG-1005–01, and through research grants R01-AG034479 and R21-AG034263. Dr. Guillermo F. López Sánchez is funded by the European Union – Next Generation EU.
Open Research
DATA AVAILABILITY STATEMENT
Data are publicly available via https://www.who.int/data/data-collection-tools/study-on-global-ageing-and-adult-health subject to approval.




