Associations of depressive rumination and positive affect regulation with emotional distress after the death of a loved one
Abstract
The death of a loved one may precipitate symptoms of prolonged grief disorder (PGD), post-traumatic stress disorder (PTSD) and depression. Brooding about the causes and consequences of one's negative affect (NA), also termed depressive rumination, has been linked to distress after loss. The role of dysregulation of positive affect (PA) has received less attention. We examined (1) the factor structure of depressive rumination and PA dysregulation and (2) to what extent these factors were related to PGD, PTSD and depression symptom levels. Self-report data were included from 235 Dutch bereaved people who completed measures tapping symptoms of PGD, PTSD and depression. Depressive rumination and PA regulation strategies were assessed with the Ruminative Response Scale (RRS) Brooding Scale and the Response to Positive Affect (RPA) Questionnaire (including three subscales: emotion-focused and self-focused rumination and dampening), respectively. Confirmatory factor analyses and structural equation modelling were used for data analyses. The four-factor model (i.e., depressive rumination and the three RPA subscales) showed the best fit. An increase in depressive rumination was related to higher distress levels (across all outcomes in univariate and multivariate analyses). An increase in emotion-focused rumination about PA was associated with less depression. More dampening of PA was related to higher PTSD levels. Findings suggest that, alongside the regulation of NA, the regulation of PA plays a role in how people respond to the death of a loved one. This points to the need for more research on NA and PA regulation in grief.
Key Practitioner Message
- Brooding about causes and consequences of negative affect—also termed depressive rumination—contributes to distress following loss.
- Positive affect regulation strategies likely also influence emotional reactions to loss.
- This study examined linkages of negative affect regulation (viz., depressive rumination) and positive affect regulation (viz., positive rumination and dampening) with these reactions.
- Depressive rumination was correlated with symptom levels of prolonged grief, post-traumatic stress and depression.
- Emotion-focused positive rumination and dampening of positive affect explained additional variance in depressive and post-traumatic stress symptoms, respectively.
1 INTRODUCTION
Losing a loved one is a major life event that may precipitate different forms of emotional distress. A significant minority of bereaved people develop disturbed grief, interchangeably referred to as persistent complex bereavement disorder (as per DSM-5; American Psychiatric Association [APA], 2013) or prolonged grief disorder (PGD; as per ICD-11; WHO, 2019). In addition, symptoms of post-traumatic stress disorder (PTSD) and depression may follow loss. Both at clinical and subclinical levels, these symptoms are associated with significant impairments in functioning (Boelen, Smid, Mitima-Verloop, De Keijser, & Lenferink, 2019). Given the clinical relevance and public health significance of bereavement-related emotional distress, it is important to search for factors maintaining this distress. Studying variables that are amenable to treatment interventions is particularly relevant to improve treatment options.
The current study sought to further our understanding of emotion dysregulation in grief. Emotional dysregulation refers to impairments in the processes that people may use to maintain, increase, or decrease their emotions (Carl, Soskin, Kerns, & Barlow, 2013; Gross, 2015). A growing number of studies have examined dysregulation of negative emotions after bereavement, specifically rumination. For instance, Eisma et al. (2015) found that both depressive rumination—that is, brooding about the causes and consequences of one's negative affect (NA) as defined in Nolen-Hoeksema's (1991) response style theory—as well as grief-rumination, repetitive thinking about the causes and consequences of the loss (Eisma et al., 2014), were associated with bereavement-related distress concurrently and longitudinally. Repeatedly considering these themes is also part of adaptive grief work; however, when rumination persists and serves to escape from elaborating on the meanings and implications of the loss itself and processing the associated pain, it tends to exacerbate rather than ameliorate distress (Stroebe et al., 2007). Alongside disturbances in NA regulation, the dysregulation of positive affect (PA) contributes to psychopathology. PA dysregulation represents a range of strategies people may use that decrease the frequency and duration of positive emotions, including controlled cognitive strategies such as dampening of PA (i.e., devaluating, suppressing or downgrading one's PA) and impaired savouring (i.e., considering positive aspects of moments PA was experienced) of PA (Carl et al., 2013). Research in non-clinical samples has shown that response styles to PA (particularly this dampening) are longitudinally related to depression severity, while controlling for baseline depression and response styles to NA (Raes, Smets, Nelis, & Schoofs, 2012). In addition, there is recent evidence that dysregulation of both NA and PA is associated with PTSD. For instance, in a study among women confronted with intimate partner violence, Weiss, Nelson, Contractor, and Sullivan (2019) found both dysregulation of NA and PA—including the non-acceptance of NA, as well as the non-acceptance of PA—to be associated with PTSD severity (cf. Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018).
There is overlap between symptoms and underlying mechanisms of depression, PTSD and disturbed grief (e.g., Boelen, Van den Hout, & Van den Bout, 2006). Accordingly, it is conceivable that both the dysregulation of NA and PA contribute to emotional distress following loss. From a theoretical viewpoint, there may be bidirectional relationships between PA dysregulation and persistent grief. For instance, difficulties to experience and maintain PA in the present likely fuel the tendency to yearn for and hold onto what is lost and also block the motivation to engage in activities promoting recovery. Conversely, a sense of meaninglessness about life, pessimism about the future and elevated feelings of self-blame and guilt—implicated in persistent grief—may fuel the downregulation of PA.
Although there is evidence that the experience of PA fosters recovery from loss (Bonanno & Keltner, 1997; Ong, Bergeman, Bisconti, & Wallace, 2006; Tweed & Tweed, 2011), the role of the dysregulation of PA in grief has, to our knowledge, only been addressed in one empirical study (Lenferink, Wessel, & Boelen, 2018). In that study, the Response to Positive Affect (RPA) Questionnaire (Feldman, Joormann, & Johnson, 2008) was used to tap three elements of PA dysregulation, namely, ‘dampening’ (referring to devaluating, suppressing or downgrading one's PA) and ‘self-focused and emotion-focused rumination’ (referring to ways to enhance one's PA). In addition, the ‘brooding’ subscale of the Ruminative Response Scale (RRS; Treynor, Gonzalez, & Nolen-Hoeksema, 2003) was used to tap into depressive rumination, as a form of NA dysregulation. The linkage of PA dysregulation and depressive rumination with disturbed grief, PTSD and depression was examined in two samples: one sample of 187 people, bereaved in the past 12 months, and a second sample including 134 relatives of long-term missing persons. Outcomes showed that both PA dysregulation and depressive rumination explained variance in loss-related distress.
Building on these findings, the current study further examined the linkage of depressive rumination and PA dysregulation with emotional distress following loss, specifically symptom levels of disturbed grief (operationalized as PGD as per Prigerson et al., 2009), PTSD and depression. We sought to extend these prior findings in a number of ways. First, Lenferink et al.'s (2018) study only included people in the first year of bereavement; therefore, the degree to which NA and PA dysregulation contributes to emotional distress beyond the first year of bereavement is still an outstanding question. In the current study, we included people who were all bereaved between 1 and 5 years earlier. Second, based on principal factor analysis, Lenferink et al. combined items of self-focused and emotion-focused rumination into one variable (coined ‘enhancing’); although this accords with Nelis et al.'s (2016) findings that the two types of positive rumination represent a single construct, they were originally proposed as distinct (Feldman et al., 2008). In the current study, we used confirmatory factor analysis (CFA) to examine if items tapping self-focused and emotion-focused rumination should best be considered as one or two factors. A third addition to prior research was that, in this study, items tapping depressive rumination and PA dysregulation were included in measurement and structural models; this allowed us to examine if NA and PA regulation strategies are distinguishable and to apply robust estimations of the associations of latent variables of NA and PA regulation with multiple distress outcomes.
Taken together, the first aim of this study was to examine the factor structure of depressive rumination and PA dysregulation. We expected items tapping depressive rumination and dampening to cluster in two factors, distinguishable from items representing ‘enhancing’ of PA. Because research is inconclusive about the distinctiveness of self-focused and emotion-focused rumination, we compared two models: a three-factor model with distinct dimensions of depressive rumination, dampening and enhancing, and a four-factor model, in which enhancing was divided into self-focused and emotion-focused rumination. The second aim was to examine the linkage of distinct factors of depressive rumination and PA dysregulation with symptom levels of PGD, PTSD and depression. Based on prior work (Lenferink et al., 2018), we anticipated that both depressive rumination and one or more element of PA dysregulation would be correlated with these symptom levels.
2 METHODS
2.1 Participants and procedure
Data were collected in the context of the Utrecht Longitudinal Study on Adjustment to Loss (ULSATL project), studying the course of loss-related distress and its cognitive and behavioural correlates. The study was approved by the ethical review board of the social sciences faculty at Utrecht University (FETC16-062). Participants were recruited via announcements on internet websites. After applying for participation, participants were referred to a secured website where more information about the study was given and an informed consent form could be completed. Then, participants completed the questionnaires online. Data were included from 235 participants who were all bereaved between 1 and 5 years earlier. Most (89.4%) were women. The mean age was 51.1 (SD = 11.9, range 19–78) years, 136 (57.9%) participants had college/university level education, and 99 (42.1%) had followed lower levels of education. Ninety-five (40.4%) participants lost a partner, 24 (10.2%) a child, 14 (6.0%) a sibling, 87 (37.0%) a parent and 15 (6.4%) some other loved one. The average time since lost was 29.3 (SD = 13.5) months. Losses were due to natural/non-violent causes in 209 (88.9%) participants and due to unnatural/violent causes (suicide, homicide or accidents) in 26 (11.1%) participants.
2.2 Measurements
The PGD scale (Boelen, Keijsers, & van den Hout, 2012) was used to assess symptom levels of PGD, in accord with criteria from Prigerson et al. (2009). It includes 11 items representing one separation distress symptom, nine cognitive and emotional symptoms and one functional impairment symptom. Respondents rate how frequently they experienced each grief reaction during the preceding month on 5-point scales ranging from 1 (never) to 5 (always). The PGD scale has good reliability and concurrent and predictive validity (Boelen et al., 2012). Cronbach's α in the current sample was .91.
PTSD Symptom Scale–Self-Report (PSS-SR) version. The PSS-SR is a 17-item measure of PTSD, as defined in the fourth Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA, 2000). Participants rate the frequency of symptoms during the preceding month on 4-point scales (0 = not at all, 3 = five/more times per week/almost always). The index event was defined as ‘the death of your loved one’ (e.g., ‘How often did you have unpleasant dreams or nightmares about the death of your loved one?’). English (Foa, Riggs, Dancu, & Rothbaum, 1993) and Dutch versions (Engelhard, Arntz, & van den Hout, 2007) have good psychometric properties. In the current sample, the α was .91.
The depression subscale of the Hospital Anxiety and Depression Scale (HADS-D) was used to assess depressive symptoms (Zigmond & Snaith, 1983). This 7-item measure instructs respondents to select one of four answers that best describes how frequently they experienced the symptoms during the past week (e.g., “I feel as if I am slowed down”). Items are scored on a 0 to 3 scale. The HADS-D showed good psychometric properties (Bjelland, Dahl, Haug, & Neckelmann, 2002). Cronbach's α in the current study was .92.
RRS Brooding Scale. The brooding scale of the RRS is a well-validated 5-item subscale of the 22-item RRS (Treynor et al., 2003). This subscale taps into unconstructive pondering (e.g., ‘I think “Why do I always react this way?”’) in response to a sad/depressed mood. Respondents rate to what extent they engage in the responses represented by each item on 4-point scales (1 = almost never to 4 = almost always). English (Treynor et al., 2003) and Dutch studies (Schoofs, Hermans, & Raes, 2010) have corroborated the psychometric qualities of the RRS, including its brooding scale. In this study, the α of the brooding scale was .79.
RPA Questionnaire. The RPA is a 17-item instrument developed by Feldman et al. (2008). Respondents rate what they normally do when they feel happy, excited or enthused on a 4-point scale ranging from 1 (almost never) to 4 (almost always). The items represent three dimensions, namely, ‘dampening’ (seven items, e.g., ‘Remind yourself these feelings won't last’), ‘self-focused positive rumination’ (four items, e.g., ‘Think “I am achieving everything”’) and ‘emotion-focused positive rumination’ (five items, e.g., ‘Think about how happy you feel’). The well-validated Dutch version was used; this includes 16 items, with item ‘Think about how hard it is to concentrate’ being removed due to low factor loadings (Raes, Daems, Feldman, Johnson, & Van Gucht, 2009). In the current sample, αs were .76 (dampening), .86 (self-focused rumination) and .83 (emotion-focused rumination).
2.3 Statistical analyses
Statistical analyses were performed in Mplus version 8.4 (Muthén & Muthén, 1998–2019) in two stages. In the first stage of the analyses, a measurement model was tested. CFAs were performed to examine the factor structure of the fiveitems tapping depressive rumination (RRS Brooding Scale) and the 16 items tapping PA regulation (RPA). All items were rated on 4-point Likert scales and therefore considered categorical. A robust weighted least squares estimation method (WLSMV) was used for the CFAs. The statistical fit of a three-factor model (depressive rumination, dampening and enhancing) was compared with a four-factor model (depressive rumination, dampening, self-focused rumination and emotion-focused rumination). To evaluate model fit, the following fit statistics were considered (Kline, 2005): (a) comparative fit and Tucker–Lewis index (CFI and TLI) with values more than 0.90 indicating adequate fit (and more than 0.95 excellent fit) and (b) root-mean-square error of approximation (RMSEA) and standardized root mean square residual (SRMR) with values less than 0.10 representing acceptable fit (and less than 0.05 excellent fit). We tested whether the fit of the four-factor model was significantly better than the three-factor model by using the DIFFtest command in Mplus. A maximum of two responses were missing for each RRS and RPA item. These missing data were handled using full maximum likelihood estimation.
In the second stage of the analyses, structural equation modelling (SEM) was used to examine the associations of depressive rumination and PA dysregulation with symptom levels of PGD, PTSD and depression by regressing each of these outcomes on each factor of the measurement model. Outcomes were predicted in three distinct models. Additionally, in order to account for the associations between PGD, PTSD and depression symptoms, we also included these outcomes simultaneously in one multivariate model. Known risk factors of symptoms were included in SEM as covariates, including gender (0 = male, 1 = female), age (in years), educational level (0 = lower than college/university, 1 = college/university), cause of death (0 = natural, 1 = unnatural) and time since loss (in months). We also included kinship; to limit the number of variables in the models, this variables was dichotomized as 0 = death of partner or child, 1 = death other person. Death of partner and child were combined because evidence shows that both these losses yield substantially more distress, relative to other losses (e.g., Lenferink, Nickerson, de Keijser, Smid, & Boelen, 2020). We included the covariates by regressing the symptom levels of psychopathology on these risk factors. One respondent had missing values on the covariates and was therefore excluded from the SEM analyses.
3 RESULTS
3.1 Descriptive statistics
We calculated the number of people meeting criteria for a provisional PGD diagnosis by treating each item rated as more than 3 as ‘symptom endorsed’ and then follow Prigerson et al.'s (2009) diagnostic rule that requires endorsement of (i) the yearning (Criterion A) item, (ii) the functional impairment item and (iii) more than 4 of the remaining (Criterion C) items. Accordingly, n = 22 (9.4%) met criteria for probable PGD. In addition, n = 26 (11.1%) met criteria for probable PTSD according to the DSM-IV (APA, 2000) based scoring rule put forth by Brewin, Andrews, and Rose (2000) with symptom scores of at least 2 (two to four times a week/half of the time) on at least one reexperiencing, three avoidance and two hyperarousal symptoms. Also, n = 62 (26.4%) scored beyond the threshold of more than 7 on the HADS-D indicating elevated depression (Bjelland et al., 2002).
3.2 Measurement model
The three-factor model did not show an adequate fit (χ2 = 656.76 (186), p < .001, RMSEA = 0.104, (90% CI; 0.095–0.112), CFI = 0.890, TLI = 0.876, SRMR = 0.102). All factor loadings were above 0.600, except for RPA item 6 (‘Think “This is too good to be true”’) and RPA item 11 (‘Think “People will think I'm bragging”’), which had factor loadings of 0.040 and 0.488, respectively. Also considering prior evidence that these items perform relatively poorly (Lenferink et al., 2018; Nelis et al., 2016), these items were removed from subsequent analyses. Table 1 shows the fit indices for the three- and four-factor model. The three-factor model showed acceptable fit (after removal of RPA items 6 and 11). The ‘enhancing’ factor was significantly and moderately (r = −.31) related to the ‘dampening’ factor and significantly and weakly related to ‘depressive rumination’ (r = −.26). ‘Dampening’ was significantly and strongly related to ‘depressive rumination’ (r = −.69). The four-factor model showed a better fit compared with the three-factor model as evidenced by higher CFI and TLI values and lower RMSEA and SRMR values. The chi-square difference test supported this (Δχ2 = 42.37 (3), p < .001). The factor loadings and associations between the four factors are shown in Table 2.
| CFI | TLI | RMSEA (90% CI) | SRMR | Chi square | DF | |
|---|---|---|---|---|---|---|
| Three-factor model: Enhancing, dampening and depressive rumination | 0.938 | 0.929 | 0.085 (0.076–0.096) | 0.080 | 404.791 | 149 |
| Four-factor model: Emotion-focused positive rumination, self-focused positive rumination, dampening and depressive rumination | 0.954 | 0.946 | 0.075 (0.064–0.085) | 0.072 | 337.275 | 146 |
- Abbreviations: CFI, comparative fit index; RMSEA, root-mean-square error of approximation; SRMR, standardized root mean square residual; TLI, Tucker–Lewis index.
| Item | Emotion-focused positive rumination | Self-focused positive rumination | Dampening of positive affect | Depressive rumination |
|---|---|---|---|---|
| Notice how you feel full of energy | 0.778 | |||
| Savour this moment | 0.845 | |||
| Think about how happy you feel | 0.823 | |||
| Think how strong you feel | 0.881 | |||
| Think about how proud you are of yourself | 0.623 | |||
| Think ‘I am getting everything done’ | 0.829 | |||
| Think about how you feel up to doing everything | 0.910 | |||
| Think ‘I am living up to my potential’ | 0.837 | |||
| Think ‘I am achieving everything’ | 0.780 | |||
| Think about things that could go wrong | 0.696 | |||
| Remind yourself these feelings will not last | 0.774 | |||
| Think ‘I do not deserve this’ | 0.791 | |||
| Think ‘My streak of luck is going to end soon’ | 0.879 | |||
| Think about things that have not gone well for you | 0.675 | |||
| Think ‘Why do I always react this way’ | 0.687 | |||
| Think about a recent situation, wishing it had gone better | 0.628 | |||
| Think ‘Why do I have problems other people do not have?’ | 0.817 | |||
| Think ‘What am I doing to deserve this’ | 0.830 | |||
| Think ‘Why cannot I handle things better?’ | 0.754 | |||
| Correlation among factors | ||||
| Emotion-focused positive rumination | 0.796** | −0.335** | −0.299** | |
| Self-focused positive rumination | −0.255** | −0.193* | ||
| Dampening | 0.689** |
- * p < .01.
- ** p < .001.
3.3 Structural model
Using SEM, three distinct models were examined to investigate the associations between the latent variables (i.e., emotion-focused positive rumination, self-focused positive rumination, dampening and depressive rumination) and symptom levels of PGD, PTSD and depression, respectively. Age, gender, kinship, education, cause of death and time since loss were included as covariates in the models. Standardized regression coefficients for all models are summarized in Table 3 and illustrated in Figures 1-3. All three models demonstrated acceptable fit. For the model with PGD severity as dependent variable: χ2 = 532.13 (275), p < .001, RMSEA = 0.063, (90% CI; 0.055–0.071), CFI = 0.944, TLI = 0.937, SRMR = 0.127. For the model predicting PTSD severity: χ2 = 530.68 (275), p < .001, RMSEA = 0.063, (90% CI; 0.055–0.071), CFI = 0.944, TLI = 0.937, SRMR = 0.127. For the model with depression severity as dependent variable: χ2 = 538.53 (275), p < .001, RMSEA = 0.064, (90% CI; 0.056–0.072), CFI = 0.942, TLI = 0.934, SRMR = 0.127. PGD severity was significantly associated with depressive rumination only, PTSD severity with dampening and depressive rumination and depression severity with emotion-focused positive rumination and depressive rumination.
| β | SE | p value | |
|---|---|---|---|
| Prolonged grief disorder | |||
| Emotion-focused positive rumination | −0.036 | 0.082 | .661 |
| Self-focused positive rumination | −0.001 | 0.088 | .990 |
| Dampening of positive affect | 0.084 | 0.077 | .273 |
| Depressive rumination | 0.589 | 0.071 | <.001 |
| Gender (0 = male) | −0.079 | 0.056 | .154 |
| Age in years | −0.123 | 0.067 | .065 |
| Kinship (0 = deceased is partner or child) | −0.189 | 0.064 | .003 |
| Education (0 = lower than college/university) | −0.223 | 0.062 | <.001 |
| Cause of death (0 = natural) | 0.052 | 0.065 | .423 |
| Time since loss in months | −0.130 | 0.064 | .041 |
| Post-traumatic stress disorder | |||
| Emotion-focused positive rumination | −0.069 | 0.094 | .462 |
| Self-focused positive rumination | 0.018 | 0.095 | .847 |
| Dampening of positive affect | 0.163 | 0.076 | .033 |
| Depressive rumination | 0.478 | 0.070 | <.001 |
| Gender (0 = male) | 0.026 | 0.065 | .684 |
| Age in years | −0.178 | 0.061 | .004 |
| Kinship (0 = deceased is partner or child) | −0.187 | 0.065 | .004 |
| Education (0 = lower than college/university) | −0.117 | 0.063 | .061 |
| Cause of death (0 = natural) | 0.032 | 0.064 | .622 |
| Time since loss in months | −0.129 | 0.069 | .062 |
| Depression | |||
| Emotion-focused positive rumination | −0.240 | 0.084 | .004 |
| Self-focused positive rumination | 0.015 | 0.089 | .865 |
| Dampening of positive affect | 0.112 | 0.078 | .151 |
| Depressive rumination | 0.406 | 0.067 | <.001 |
| Gender (0 = male) | −0.058 | 0.057 | .312 |
| Age in years | −0.122 | 0.060 | .042 |
| Kinship (0 = deceased is partner or child) | −0.202 | 0.068 | .003 |
| Education (0 = lower than college/university) | −0.132 | 0.065 | .042 |
| Cause of death (0 = natural) | 0.042 | 0.059 | .473 |
| Time since loss in months | −0.177 | 0.072 | .013 |
- Note: Standardized regression coefficients for models including the covariates.
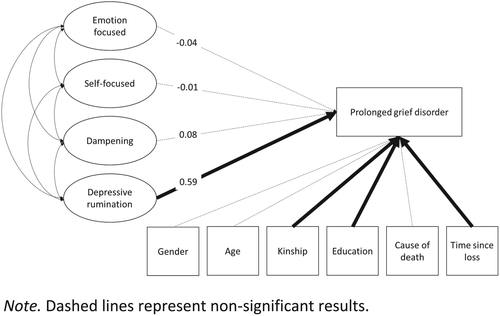
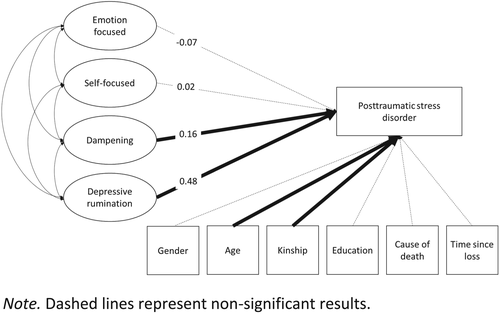
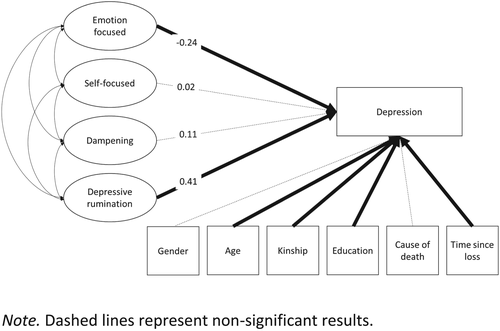
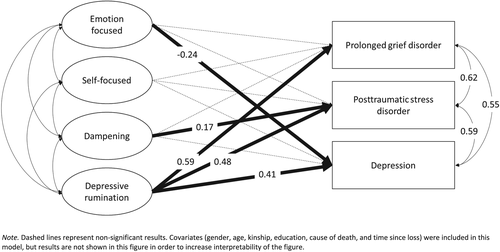
A fourth model, where all outcome variables were included simultaneously demonstrated acceptable fit (χ2 = 581.27 (305), p < .001, RMSEA = 0.062, [90% CI; 0.055–0.070], CFI = 0.937, TLI = 0.925, SRMR = 0.120). Outcomes are summarized in Table 4 and Figure 4. Higher levels of depressive rumination were strongly related to more severe PGD symptoms (β = 0.59, SE = 0.07, p <. 001) and moderately related to PTSD severity (β = 0.48, SE = 0.07, p < .001) and depression severity (β = 0.41, SE = 0.07, p < .001). An increase of use of emotion-focused positive rumination was weakly associated with lower depression severity (β = −0.24, SE = 0.08, p = .004). Increased dampening of PA was weakly related to higher PTSD severity (β = 0.17, SE = 0.08, p = .03).
| β | SE | p value | |
|---|---|---|---|
| Prolonged grief disorder | |||
| Emotion-focused positive rumination | −0.035 | 0.083 | .673 |
| Self-focused positive rumination | <0.001 | 0.088 | .997 |
| Dampening of positive affect | 0.085 | 0.076 | .269 |
| Depressive rumination | 0.591 | 0.070 | <.001 |
| Gender (0 = male) | −0.268 | 0.183 | .143 |
| Age in years | −0.010 | 0.006 | .064 |
| Kinship (0 = deceased is partner or child) | −0.378 | 0.126 | .003 |
| Education (0 = lower than college/university) | −0.450 | 0.123 | <.001 |
| Cause of death (0 = natural) | 0.162 | 0.207 | .435 |
| Time since loss in months | −0.010 | 0.005 | .040 |
| Post-traumatic stress disorder | |||
| Emotion-focused positive rumination | −0.069 | 0.094 | .466 |
| Self-focused positive rumination | 0.019 | 0.096 | .845 |
| Dampening of positive affect | 0.165 | 0.076 | .030 |
| Depressive rumination | 0.478 | 0.070 | <.001 |
| Gender (0 = male) | 0.087 | 0.213 | .683 |
| Age in years | −0.015 | 0.005 | .004 |
| Kinship (0 = deceased is partner or child) | −0.372 | 0.129 | .004 |
| Education (0 = lower than college/university) | −0.238 | 0.127 | .060 |
| Cause of death (0 = natural) | 0.103 | 0.204 | .613 |
| Time since loss in months | −0.010 | 0.005 | .062 |
| Depression | |||
| Emotion-focused positive rumination | −0.241 | 0.084 | .004 |
| Self-focused positive rumination | 0.016 | 0.090 | .854 |
| Dampening of positive affect | 0.113 | 0.078 | .145 |
| Depressive rumination | 0.407 | 0.067 | <.001 |
| Gender (0 = male) | −0.190 | 0.188 | .312 |
| Age in years | −0.010 | 0.005 | .041 |
| Kinship (0 = deceased is partner or child) | −0.403 | 0.135 | .003 |
| Education (0 = lower than college/university) | −0.268 | 0.131 | .041 |
| Cause of death (0 = natural) | 0.135 | 0.188 | .474 |
| Time since loss in months | −0.013 | 0.005 | .013 |
- Note: Standardized regression coefficients for model including covariates.
4 DISCUSSION
Very few studies have so far examined the role of PA regulation strategies in recovery from loss. We examined the association of depressive rumination (a form of NA dysregulation frequently examined in the context of grief; Eisma & Stroebe, 2017), plus dampening and (reduced) enhancing of PA (representing PA dysregulation strategies) with symptom levels of PGD, PTSD and depression among people bereaved between 1 and 5 years earlier. A first main finding was that CFAs supported a four-factor structure of distinct, yet correlated, factors of self-focused and emotion-focused rumination, dampening and depressive rumination. This finding is broadly consistent with prior research showing that regulatory difficulties connected with NA and PA represent distinguishable phenomena rather than a single dimension (Carl et al., 2013). That self-focused and emotion-focused positive rumination emerged as distinct clusters accords with some prior studies (Feldman et al., 2008; Raes et al., 2009) but not with other studies showing these forms of positive rumination essentially form one concept (Lenferink et al., 2018; Nelis et al., 2016). Findings from our CFA indicate that examining both forms of rumination about PA separately has added value. This was corroborated by findings from our SEM showing that (lower) emotion-focused positive rumination, but not self-focused positive rumination was associated with depression.
Further main findings concerned the associations of depressive rumination and PA dysregulation with bereavement-related distress. We found that depressive rumination, but not the three indices of PA dysregulation, was significantly associated with symptom levels of PGD. Further, depressive rumination was significantly associated with PTSD severity. Dampening was significantly associated with PTSD severity. Depressive rumination and (lower) self-focused rumination about PA were significantly associated with depression severity. One notable conclusion based on this is that impairments in the regulation of NA, in the form of unconstructive pondering about the causes and consequences of one's negative feelings, seems a considerably more important element of persistent bereavement-related distress than disturbances in the regulation of PA. This finding is broadly consistent with cognitive behavioural theorizing and research in which rumination in grief is conceptualized as a cognitive avoidance strategy (Stroebe et al., 2007) and narrative-constructivist conceptualizations postulating that persistent difficulties to get to the point that one has been able to make sense of the loss block the alleviation of grief (Neimeyer, 2016). Nevertheless, we still found that dysregulation of PA contributed to the explained variance in PTSD and depression severity, beyond sociodemographic and loss-related factors and depressive rumination. Pending replication of these findings in larger, preferably longitudinal, research, these findings may bear clinical implications. For instance, these suggest that, when helping bereaved people to adapt effectively to their loss, clinicians should address not only responses to negative feelings but also strategies that people use to regulate their positive feelings.
In a prior study, we examined depressive rumination and PA dysregulation among people who were all within the first year of bereavement (Lenferink et al., 2018). In that study, depressive rumination also emerged as a strong correlate of bereavement-related distress, and stronger compared with PA dysregulation. Taken together, these prior findings among relatively recently bereaved people, and the current findings obtained with more remotely bereaved people suggest that depressive rumination is critical in the onset as well as maintenance of disturbed responses to loss. Importantly, although studies in nonbereaved samples have indicated that depressive rumination is a prospective predictor of emotional distress (Watkins & Roberts, 2020), this has not been found in research among bereaved people (Eisma et al., 2015); hence, more research is needed to elucidate the role of depressive rumination in grief. In that prior study, among the more recently bereaved (Lenferink et al., 2018), self-focused and emotion-focused rumination explained variance in PGD severity, beyond depressive rumination. This was not observed in the present sample of more remotely bereaved people; that could be taken to suggest that disturbed PA regulation is involved in the onset but not the maintenance of symptoms of PGD over time.
Importantly, the present cross-sectional design does not allow drawing conclusions about the temporal order of dysregulation of NA and PA and emotional distress following loss. Further prospective and experimental studies are necessary to further our knowledge about this. Several other limitations should also be considered. About 90% of our sample consisted of women and people bereaved by a non-violent/natural loss. This calls into question the generalizability of our findings to bereaved men and people bereaved by other causes of loss. Furthermore, we assessed PGD symptoms using diagnostic criteria proposed by Prigerson et al. (2009). These criteria overlap, to some extent, both with criteria for persistent complex bereavement disorder in DSM-5 (APA, 2013) and PGD as defined in ICD-11 (WHO, 2019); that is, symptoms such as yearning/longing, difficulties accepting the loss, disbelief, bitterness/anger and difficulties pursuing interest are included in all these criteria sets (Lenferink, Boelen, Smid, & Paap, 2019). However, because the overlap between the symptoms measured in this study and criteria sets for disordered grief in DSM-5 and ICD-11 is not complete, conclusions from this study may not be fully generalizable to these other criteria-sets.
Notwithstanding these considerations, the current findings add to a growing research base showing that, alongside the regulation of NA, the regulation of PA plays a role in how people respond to and recover from different adverse life events (Weiss et al., 2018, 2019) including the death of a loved one (Coifman & Bonanno, 2010; Lenferink et al., 2018). Combined with study findings on depressive rumination in grief (Eisma et al., 2015) and PA regulation (Lenferink et al., 2018), the present findings point to the need for more research on NA and PA regulation in grief. That research could clarify whether these strategies have a different influence at different points in time following loss and vary in their impact on different emotional responses; for instance, it is possible that PA dysregulation is a more important determinant of earlier responses to loss compared with later responses and that PA dysregulation drives bereavement-related depression more than it influences symptoms of grief and post-traumatic stress. That research might also inform improvements of treatment options for persistent distress after loss and consider if extending people's repertoire in maintaining PA in the face of loss might be a fruitful approach to alleviate this distress. There is evidence from studies on ‘complicated grief treatment’ (e.g., Shear et al., 2016) and behavioural activation (Papa, Sewell, Garrison-Diehn, & Rummel, 2013) that a focus on positive experiences is indeed fruitful in alleviating disordered grief. It would be interesting for future work to enhance knowledge on which PA regulation strategies should be targeted to enhance treatment outcomes.
ACKNOWLEDGEMENT
Hans Pieterse is gratefully acknowledged for his help in the collection of the data.
CONFLICT OF INTEREST
The authors declare to have no conflict of interest.




