Histological Grading and Staging of Chronic Hepatitis
Abbreviations
-
- CAH
-
- chronic aggressive hepatitis
-
- CH
-
- chronic hepatitis
-
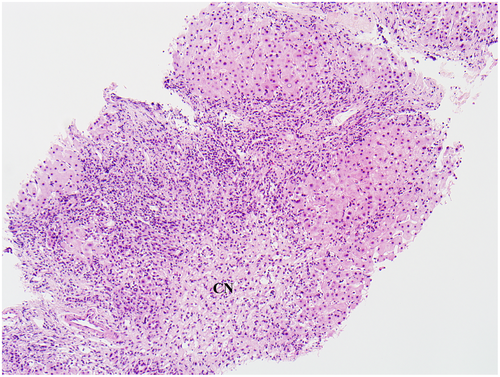
- CN
-
- confluent hepatocyte necrosis
-
- CPH
-
- chronic persistent hepatitis
-
- HAI
-
- Histological Activity Index
-
- HBV
-
- hepatitis B virus
-
- HCV
-
- hepatitis C virus
-
- IASL
-
- International Association for the Study of the Liver
-
- METAVIR
-
- Meta-analysis of Histological Data in Viral Hepatitis
-
- PMN
-
- piecemeal necrosis
Grading and Staging of Chronic Hepatitis
The liver biopsy is often an important part of the evaluation of a patient with abnormal liver function. It is the only procedure that provides a direct visualization of the extent of liver injury. If the etiology of dysfunction is not clear or involves multiple possible causes, the biopsy findings may guide the clinical team toward establishing a diagnosis and appropriate clinical management. In the setting of a known chronic hepatitis (CH), a biopsy provides information regarding: (1) the extent of ongoing necroinflammatory activity, which is a precursor to fibrogenesis; and (2) the extent of fibrosis. These two variables have drawn comparisons with neoplastic processes and have thus been termed “grade” and “stage,” respectively. In addition, the biopsy may reveal other concurrent processes (such as fatty liver disease and iron overload) that may influence the prognosis and management. This review is limited to grading and staging of CH, such as viral and autoimmune hepatitis, and does not include discussion of steatohepatitis. It outlines the goals and basic elements of grading and staging, a historical perspective, and the common currently used systems.1-3
Goals and Limitations of Grading and Staging
All grading and staging systems are created with the following goals: (1) reflecting the current extent of liver injury using relatively discrete categories or scores, (2) ensuring relevance in clinical care and/or research, and (3) acceptable reproducibility. Notably, all such systems are dependent on subjective evaluation of histological features, and the interobserver agreement for these features is variable; generally, the kappa values for degree of fibrosis are higher than that for necroinflammatory changes.2 Also, with the use of the schema, discrete categories are created of processes that are a histological continuum. Other considerations include the adequacy of the biopsy sample, variability in pathological changes in different areas of the liver, and the confounding features of other concurrent disease processes, such as steatohepatitis and iron overload. For evaluation of grade and stage in CH, a biopsy measuring 20 mm in length with more than 10 portal tracts is considered optimal.1 Transjugular biopsies tend to be smaller, fragmented, and include the vein wall and surrounding collagen that could be overinterpreted as advanced fibrosis.4 Intraoperative biopsies should include deeper liver parenchyma to avoid difficulties with staging caused by subcapsular fibrosis. This is best achieved with a core biopsy of adequate size. In a patient with no known liver disease and a nodular-appearing liver seen intraoperatively, a larger wedge biopsy, including deeper tissue, may be helpful to evaluate for nodular regenerative hyperplasia as a differential diagnostic consideration. Regional changes that may affect assessment of fibrosis include changes secondary to mass lesions and localized areas of postnecrotic scarring.
Historical Perspective
Multiple grading and staging terminologies and systems have been established over the last 60 years. The approach has evolved with better understanding of the etiology and natural course of chronic hepatitides, and the availability and need to evaluate newer treatment options. Early descriptive classifications emphasized the pattern of necroinflammatory injury as prognostic categories, leading to use of terminologies such as “chronic persistent,” “chronic aggressive,” “chronic active,” and “chronic lobular hepatitis.”5, 6 Unfortunately, rather than being prognostic categories, these were increasingly being considered as disease entities and, therefore, are not currently used. This was followed in 1981 by a detailed scoring system proposed by Knodell et al.7; the major drawback of this system was combining the score for activity and fibrosis. A modification of this system was later proposed by Ishak et al.8 in 1995 and is currently popular, especially in the setting of clinicopathological studies. In the 1990s, more concise systems were proposed, which were easier to use for clinical reporting. This was led by the Scheuer system (1991) and followed by the International Association for the Study of the Liver (IASL) system (1994), Batts and Ludwig system (1995), and Meta-analysis of Histological Data in Viral Hepatitis (METAVIR) system (1996) (Table 1).9-12 A comparison of grade and stage in three simple systems is shown in Tables 2 and 3, respectively. The reader is encouraged to review the reference publications for the various systems for further details.
| System | Description | Author(s) | Year |
|---|---|---|---|
| CPH/CAH5 | Two descriptive categories based on presence and extent of PMN: portal inflammation with no/minimal PMN (CPH) or prominent PMN (CAH) | De Groot et al. | 1968 |
| HAI7 | Numerical scoring of three activity variables (piecemeal/bridging necrosis 0-10, intralobular degeneration and focal necrosis 0-4, portal inflammation 0-4), and fibrosis 0-4, all added as a final HAI score (0-22) | Knodell et al. | 1981 |
| Scheuer9 | Subjective assessment of two activity variables (portal/periportal and lobular activity) and fibrosis, with overall numerical grade (0-4) and stage (0-4) | Scheuer | 1991 |
| IASL10 | Etiology (e.g., HCV, HBV), combined with descriptive reporting of grade and stage (grade: none, minimal-mild, moderate, severe; fibrosis: none, mild, moderate, severe/cirrhosis) | Desmet et al. | 1994 |
| Batts-Ludwig11 | Subjective assessment of two activity variables (PMN and lobular inflammation/necrosis) and fibrosis, with overall numerical grade (0-4) and stage (0-4); reproducibility enhanced by included schematic diagrams for grade and stage | Batts and Ludwig | 1995 |
| Modified HAI8 | Modified from HAI (above), numerical scoring of four activity variables (PMN 0-4, confluent necrosis 0-6, focal necrosis/apoptosis/focal inflammation 0-4, portal inflammation 0-4), and fibrosis 0-6. Activity scores are added (0-18) and reported separately from fibrosis score (0-6) | Ishak et al. | 1995 |
| METAVIR12 | Numerical scoring of two activity variables (PMN 0-3 and lobular necrosis 0-2), combined in an algorithm to obtain a final activity score (A0-A3), and separate fibrosis score (F0-F4) | Bedossa et al. | 1996 |
| IASL | Batts-Ludwig | METAVIR |
|---|---|---|
| CH, minimal activity | Grade 1 | A1 |
| CH, mild activity | Grade 2 | A1 |
| CH, moderate activity | Grade 3 | A2 |
| CH, marked activity | Grade 4 | A3 |
| CH, marked activity + bridging/multiacinar necrosis | Grade 4 | A3 |
- Although the criteria for different grades are not identical in the three systems, emphasis is placed on PMN (interface hepatitis) and lobular injury/inflammation.
| Histological Findings | IASL | Batts-Ludwig | METAVIR |
|---|---|---|---|
| No fibrosis | No fibrosis | Stage 0 | F0 |
| Fibrous portal expansion | Mild fibrosis | Stage 1 | F1 |
| Periportal fibrosis + occasional septae | Moderate fibrosis | Stage 2 | F2 |
| Many septae + architectural distortion | Severe fibrosis | Stage 3 | F3 |
| Probable/Definite cirrhosis | Cirrhosis | Stage 4 | F4 |
Essential Components of Grading and Staging
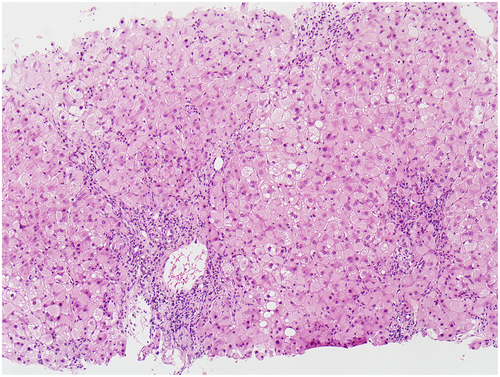
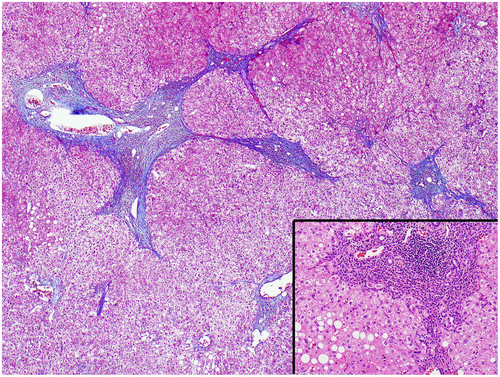
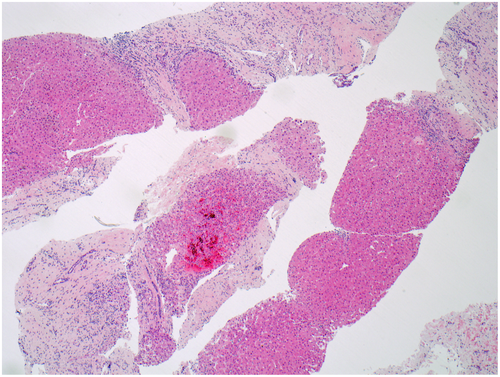
All grading systems include morphological assessment for inflammation and hepatocellular necrosis. The extent and distribution of these processes form the basis of grading. All staging systems are based on quantifying the extent of fibrosis that follows persistent necroinflammatory injury. In CH, the fibrosis occurs in the portal tracts initially and progressively expands the tracts over time, forming “bridges” or “septae” between adjacent portal tracts (less often between portal tracts and central veins). When the process involves the liver diffusely and is accompanied by regenerative nodule formation, it is called cirrhosis (“end-stage liver”). A trichrome stain is useful in confirming the presence of fibrosis. Examples of a few grades and stages of CH are illustrated in Figs. 1, 2, 3, and 4.
Choosing The Grading/Staging System
In practice, a pathologist, often in conjunction with the hepatologist, has to decide which system to use and has the option to choose from several that are mentioned earlier. Whichever system is used, it is very important that the criteria are applied consistently and the clinical team is adequately familiar with it.3 Generally, using simpler systems for clinical care is sufficient. Mention of the system in the report obviates any confusion, especially if the patient is also seeking care at another institution. Care should be taken for cases with more than one pathological process, such as CH C and steatohepatitis. It is important to be aware that the grading and staging systems were not designed for such combined clinical situations. It is often helpful to include a description of the histological findings in the report in addition to providing a grade and stage. For the purpose of research studies, a popular current system used is the Modified Histological Activity Index.8
In summary, grading and staging are important elements of evaluating and reporting liver specimens in CH, and they can be done effectively using one of the established systems. For such an effort to be meaningful in the clinical context, the systems should be used with a clear understanding of the criteria and reporting categories, their implications in patient care, and the importance of an adequate biopsy.