Hybrid Transcatheter Pulmonary Valve Replacement With SAPIEN S3 Following Right Ventricular Outflow Tract Reduction Using Tricuspid Annuloplasty Rings
ABSTRACT
We describe a novel variation of hybrid TPVR using a tricuspid annuloplasty ring which can be considered for patients with very large RVOT, short pulmonary artery, and limited vascular access and to avoid the risk of cardiopulmonary bypass. The utilization of Carpentier-Edwards Physio Tricuspid annuloplasty ring can reduce the size of the RVOT and at the same time the ring served as an effective docking site for the implantation of the SAPIEN S3 (Edwards Lifesciences). All three reported cases showed satisfactory immediate hemodynamic and clinical outcomes as well as at mid-term follow up.
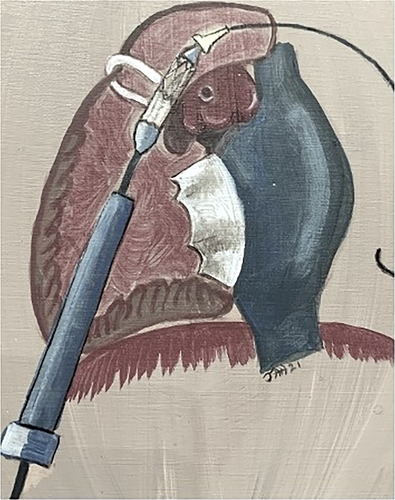
Transcatheter pulmonary valve replacement (TPVR) has emerged as a non-surgical alternative to surgical pulmonary valve replacement [1]. However, there were specific challenges and limitations associated with TPVR, particularly in patients characterized by either excessively large or abnormal right ventricular outflow tract (RVOT) anatomy [2, 3]. Therefore, hybrid TPVR has emerged as the complimentary operation and intervention for these patients in need. Reported cases of PA banding or PA plication to decrease the size of the dilated RVOT to facilitate TPVR have been previously described. Alternately, transcatheter the Alterra Adaptive Pre-stent (Edwards Lifesciences) was designed to internally reduce RVOT size but this technology was not yet available at the time [4-11]. Additionally, the Harmony platform was also not available in Thailand and the Venus P valve was still in clinical trials. Our hybrid approach also provides an alternate access of TPVR particularly in small pediatric patients to avoid vascular complications [9, 10]. Moreover, some of these patients with co-morbidities can also be benefit from hybrid operations by avoiding cardiopulmonary bypass. We report three cases of Hybrid TPVR using SAPIEN S3 (Edwards Lifesciences, Irvine, CA) valve following RVOT size reduction using the Carpentier-Edwards Physio Tricuspid annuloplasty ring (Edwards Lifesciences, Irvine, CA) through midline sternotomy (Figure 1). The Carpentier-Edwards Physio Tricuspid annuloplasty ring is used to reduce main pulmonary artery size and serves as an excellent and stable landing zone for implantation of SAPIEN S3 well above the level of the muscular RVOT.
Case 1: A 9-year-old boy (height 129 cm, weight 21 kg, BSA 0.82 m2) with double outlet right ventricle with severe infundibular and valvular pulmonary stenosis, and large inlet ventricular septal defect (VSD). He underwent surgical total correction using transannular patch to enlarge RVOT and pulmonary annulus at age 2 ½ year old. During clinical follow up, he had been failure to thrive. Cardiac MRI showed ventricular ejection fraction (LVEF) 51.7%, right ventricular ejection fraction (RVEF) 40.1%, right ventricular end diastolic volume index (RVEDVI) 166.3 mL/m2, pulmonic regurgitation fraction (PRF) 51.3%. RVOT diameter measured 27 mm. Initial cardiac catheterization with balloon sizing, the RVOT was expandable with the waist of balloon measuring 31.3 mm.
Case 2: A 31-year-old man (height 170 cm, weight 79 kg, BSA 2.0 m2) underwent Tetralogy of Fallot (TOF) surgical total correction at 7 years of age and LPA stenting at 20 years of age. He subsequently developed severe PR and underwent surgical pulmonic valve replacement using Homograft # 29 mm at 21 years of age. The perioperative neurologic complication was described as stroke and seizure. During the 10 year-period of follow up, he became gradually declined in his functional status. Cardiac MRI showed LVEF 67.0% and RVEF 41.0%, respectively. RVEDVI 158.1 mL/m2, PRF 29.7%, and RVOT diameter 28.1 mm. Initial cardiac catheterization with balloon sizing, the RVOT was expandable with the waist of balloon measuring 34.9 mm.
Case 3: A 15-year-old female adolescent (Height 146 cm, weight 38 kg, BSA 1.2 m2) underwent TOF and complete atrioventricular septal defect (AVSD) surgical total correction with RVOT reconstruction using pericardial patch and pericardial monocusp at 4 years of age. Cardiac MRI showed: LVEF 43.0%, RVEF 29.3%, RVEDVI 151.9 mL/m2, PRF 52%, and RVOT diameter measured 34.0 mm.
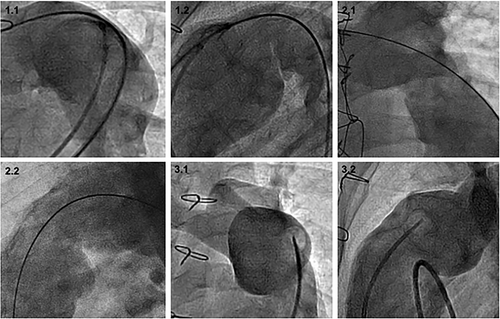
Figure 2 illustrated RVOT angiography in frontal and lateral projections of the three patients.
1 Surgical Operation and TPVR Placement
All procedures were performed under general anesthesia in a hybrid operating room. Transesophageal echocardiography (TEE) was available. Midline sternotomy was performed. For this approach, circumferential dissection of RVOT is not required. RVOT size was reduced by externally placed Carpentier-Edwards Physio Tricuspid annuloplasty ring at an anterior part of the RVOT at the location intended to deploy SAPIEN S3.
Usually, the ring is placed at least 1 cm below pulmonary artery bifurcation for optimal valve placement. Once the ring is in place, it was secured to RVOT the with 4-0 prolene suture to improve stability. The surgical incision was left open for the duration of the procedure.
Carpentier-Edwards Physio Tricuspid annuloplasty ring is a rigid incomplete ring with specific size. It constructed of a titanium core with a silicone sewing ring margin covered with a polyester cloth (Figure 3).
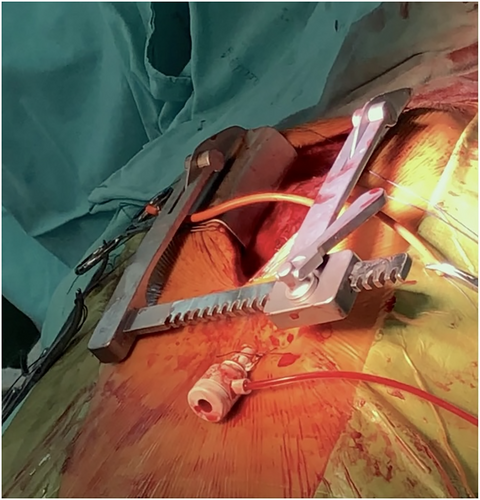
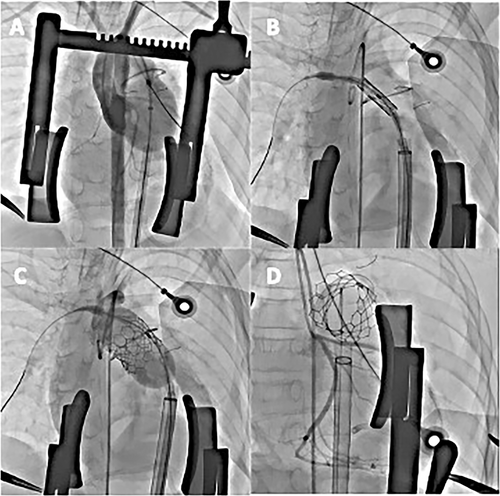
RV apex was punctured using direct visualization to access RVOT with 6 Fr sheath. A Lunderquist Extra-Stiff Wire (Cook Medical, Bloomington, IN) was positioned in a distal branch PA via the JR catheter. A 6 Fr sheath was then exchanged to Certitude delivery system (Edwards Lifesciences, Irvine, CA), superficially 18 Fr system for SAPIEN S3#26 and 21 Fr system for S3#29 valve, respectively. A sizing balloon was then used to confirm the new RVOT size and to test for the risk of coronary and aortic compression. SAPIEN S3 valve positioning is relatively straight forward, as the tricuspid ring has a distinct fluoroscopic landmark. Not only does the ring effectively reduce the pulmonary artery size, but it also provided a landing zone for the SAPIEN S3 valve (Figure 3).
Multiple fluoroscopic angles are required to confirm that the valve was within the ring, not at the ring-free zone before implantation. The valve was then fully deployed by slow balloon inflation aiming at 60−40 position using the ring as the landmark. The valve function was confirmed by angiography and trans-esophageal echocardiogram after deployment (Figure 4).
Case 1: The hybrid implantation of SAPIAN S3 #26 in TV ring use Carpentier-Edwards Physio Tricuspid annuloplasty ring #26 was successful. There was no major adverse event. There was no valvular and paravalvular regurgitation after implantation.
Over 5 year of clinical follow up, the patient was in functional class I. Last echocardiogram showed TPVR in stable position with trivial valvular PR with maximal PG of 22 mmHg. There was mild TR, TAPSE 16 mm, and LVEF 80%.
Case 2: Successful hybrid implantation of SAPIAN S3#29 in TV ring use Carpentier-Edwards Physio Tricuspid annuloplasty ring #26. This case was complicated by tearing of ascending aorta during open sternotomy, but hemostasis was obtained. There was no valvular and paravalvular pulmonary regurgitation after implantation. Over 3 years clinical follow-up, the patient was in functional class I and echocardiogram showed TPVR in stable position with TPVR maximal PG 21 mmHg, no paravalvular leakage (PVL), functioning SAPIAN S3 without intra-valvular PR, mild TR, TAPSE 1.9, and LVEF 63%.
Case 3: The hybrid implantation of SAPIAN S3# 29 in TV ring use Carpentier-Edwards Physio Tricuspid annuloplasty ring #28 was successful. There was no major adverse event.
Last 3 years of echocardiogram consisted on stable TPVR position with trivial PR, maximal pressure gradient of 11 mmHg across RVOT, RV TAPSE 19 mm, LVEF 72%.
The patient was in functional class I at last clinical follow (3 years after the procedure).
2 Discussion
The benefits of hybrid strategy include the ability to reduce the patient's RVOT/pulmonary artery dimension, enhance device deliverability, shorten procedure time and avoid the use of cardio-pulmonary bypass machine (CPB). Additionally, this approach overcomes the limitation of sheath size and maneuverability by allowing the use of larger sheaths and devices in smaller patients. Finally, this technique also allows us to place a short balloon expandable valve well above the muscular RVOT. Patients that we would consider for hybrid approaches are those that may benefit from avoiding cardiopulmonary bypass. A collaborative approach involving a multidisciplinary team consisting of surgeons, interventionists as well as imaging specialists are essential when planning and executing any such hybrid procedure using novel innovative techniques, in treating patients who are not suitable for TPVR and have compelling reasons to avoid standard surgical valve replacement.
Our case series demonstrated successful treatment in all patients using a novel hybrid approach that involved the utilization of Carpentier-Edwards Physio Tricuspid annuloplasty ring to reduce the size of the RVOT. At the same time the ring served as an effective docking site for the implantation of the SAPIEN S3. The advantages of using the annuloplasty ring include its rigid nature and reliability in externally reducing the size of the RVOT. Moreover, the Edwards tricuspid physio-band has a three-dimensional shape which allows for a longer ‘landing zone’ than would be possible with a flat ring or band. As a medically graded device with specific sizing and incomplete ring, the annuloplasty ring allows simple and durable placement. In addition, the ring provides stable anchoring, and is easily visualized via fluoroscopy for accurate transcatheter valve deployment.
However, caution must be exercised to ensure optimal placement of SAPIEN 3 valve within the annuloplasty ring and not in the ring free zone. This can be confirmed through the use of multiple fluoroscopic angles and pre-implantation balloon testing. Median sternotomy provides optimal view of the operative site, while direct RV access facilitates relatively straight delivery pathway of the device to the landing zone. This technique also opens options for other adaptations, such as using a traditional transcatheter approach, if ones wish to avoid ventriculotomy and anterior thoracotomy for ring placement without the need for CPB.
All three patients showed sustained satisfactory hemodynamics and clinical outcomes during a mean follow-up period of 40 months (ranging from 32 to 55 months).
Recently FDA approval of Alterra Adaptive Prestent, which has been specifically designed to internally remodel a wide range of RVOT morphologies and sizes, thereby creating a suitable ‘landing zone’ for the implantation of a 29-mm SAPIEN valve, could be less invasive alternative option than the hybrid operation [8]. However, there are concerns over erosion of stent struts, with reported patients requiring reintervention due to concerns of main pulmonary artery perforation [12], as well as risk of interaction with muscular RVOT causing ventricular arrhythmias. In selected patients, we do believe this hybrid approach is an alternative option specifically those with very large RVOT, short pulmonary artery, certain challenging RVOT anatomies and small vascular access. In addition, this technique also has advantage of keeping the valve platform out of RVOT, which may keep this procedure relevant overtime.
3 Conclusion
We describe a novel variation of hybrid TPVR using a tricuspid annuloplasty ring which can be considered for patients with very large RVOT, short pulmonary artery, certain very challenging RVOT anatomies and limited vascular access. The procedure could be performed successfully with satisfactory and sustained hemodynamics and also good clinical outcomes at mid-term follow up.
Acknowledgments
All authors wish to thank Dr. Jamil Aboulhosn who shared the idea of this hybrid TPVR technique and proctored us on the first case.
Conflicts of Interest
Dr. Mann Chandavimol and Dr. Jamil Aboulhosn are consultants and proctors for Edwards Lifesciences. The other authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




