Coronary artery embolism from infectious endocarditis treated with catheter thrombectomy using a GuideLiner catheter
Conflict of interest: Nothing to report.
Abstract
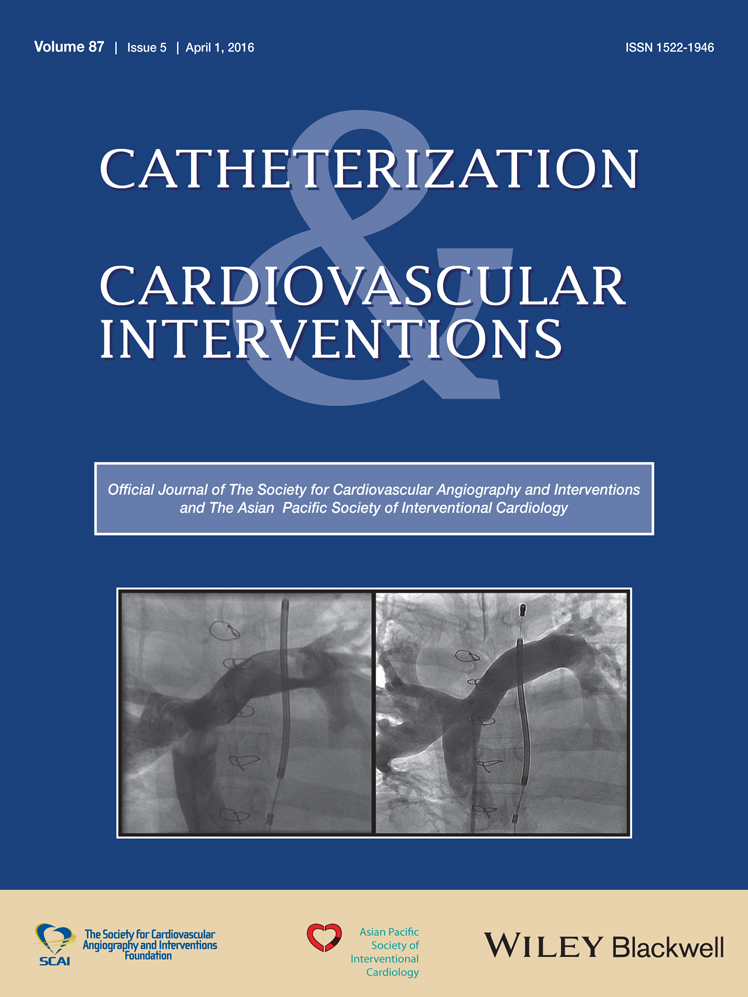
A 27-year-old male with history of IV drug use and recurrent endocarditis necessitating bioprosthetic mitral and tricuspid valve replacements presented with 2 weeks of fevers and chest pain. ECG revealed inferior ST-elevation myocardial infarction and he was taken urgently to the cardiac catheterization laboratory. Coronary angiography revealed thrombotic occlusion of the distal right coronary artery (RCA) with no angiographic evidence of atherosclerotic disease. Aspiration thrombectomy was performed followed by rheolytic thrombectomy. Despite multiple attempts at thrombectomy, significant residual organized thrombus persisted in the distal RCA. Therefore, further thrombectomy was performed by placing a GuideLiner catheter (Vascular Solutions, Minneapolis, MN) deep within the right coronary artery near the bifurcation into the posterior descending and posterior left ventricular arteries. After repeat aspiration, there was significant improvement with thrombolysis in myocardial infarction 3 flow. Intravascular ultrasound of the RCA revealed a normal-appearing vessel without evidence of atherosclerotic disease and mild residual thrombus. The decision was made to not pursue stent placement, given the concern for a likely embolic source. Following the procedure, the patient's chest pain resolved and his ST-segments normalized. © 2015 Wiley Periodicals, Inc.