Influence of the antiscatter grid on dose and image quality in pediatric interventional cardiology X-ray systems
Conflict of interest: Nothing to report.
Abstract
Objective
To present a methodology and experimental results to assess the influence, in terms of dose and image quality, of the antiscatter grid (AG) in a pediatric cardiology X-ray system.
Method
Entrance surface air kerma and image quality, using a test object and different added thicknesses of polymethyl methacrylate (PMMA), for three different acquisition protocols, were measured with and without the AG, for fluoroscopy and cine modes. The image quality parameters, signal-to-noise ratio (SNR), high-contrast spatial resolution (HCSR) and two figures of merit (FOM) were evaluated.
Results
The average bucky factor values measured during this experiment were 1.99, 2.49, 2.85, and 3.30, respectively for 4, 8, 12, and 16 cm of PMMA. SNR variations do not appear to be relevant when removing the AG. However, the use of AG improves HCSR significantly. Imaging the test object with 4 cm of PMMA seems appropriate without the AG, but for 8 cm (equivalent to chest thicknesses of 12 cm) and greater thicknesses, a good image quality would require the use of AG.
Conclusions
The AG should not be used for neonates and very young children with chest thicknesses equal to or less than 6 cm and weight less that 6 kg. © 2013 Wiley Periodicals, Inc.
INTRODUCTION
The antiscatter grid is a tool placed between patient's body and the image detector used for reducing the scattered radiation produced by the patient during X-ray imaging which reaches the image detector. It is constructed of alternate strips of an X-ray absorbing material, such as lead, and a relatively nonabsorbing interspace material, such as carbon fibre or aluminium 1. It is a general recommendation that antiscatter grid should be removed in interventional X-ray systems for pediatric procedures, but few studies have been made to quantify the degradation in image quality versus the benefit in patient dose reduction. According to the standardization documents for interventional radiology equipment 2, the antiscatter grid should be easily removable.
Pediatric patients require special attention in radiation protection aspects because of the higher radiosensitivity of their tissues compared with those of adults 3. The risk of cancer induction by ionizing radiation is three times higher for newborns and children than for adults, in accordance to the International Commission of Radiological Protection 4. This higher risk is also explained by the longer life expectancy in children for expression of any harmful effects of radiation 5. Therefore, it is important to reduce radiation doses, following the recommendations of the “Image Gently and Step Lightly campaigns”, which addressed in the US the issue of radiological responsibility, focusing on the risks of unnecessary and excessive medical radiation from pediatric interventional radiology 6.
Antiscatter grid improves the image quality, removing a substantial part of scatter radiation, but also increases the incident dose 7-10. It is widely accepted that the improvement in image quality compensates for the dose increase in adult patients, but it is recommended to remove it for younger (and smaller) patients, as the scatter radiation intensity is smaller and the derived dose decrease would outweigh the image quality degradation.
All modern interventional systems are equipped with some kind of Automatic Exposure Control (AEC) or Automatic Dose Control (ADC) as well called as Automatic Brightness Control (ABC). Each system operates trying to maintain a constant dose at the image receptor to produce a good image quality (brightness and contrast) on the viewing monitor, independently of the thickness or patient anatomic composition. The AEC operates combining the radiographic parameters kVp, mA and pulse time and different algorithms that include copper filtration in the X-ray beam, especially in pediatrics 11, 12. The fluoroscopic technique that produces optimum image quality with a minimal radiation dose suggests a more efficient combination of radiographic parameters in neonates (high kV and low mA) than in an adult patient 13.
It is not fully clear to pediatric interventional cardiologists when and for which patient sizes antiscatter grid should be removed. Some authors recommend its steady use, even with newborns 14, while others recommend the opposite 13, 15-17. Some others suggest its removal only for infants or younger children 7, 18-21.
Most of the studies 7, 8, 10, 14 to evaluate antiscatter grid performance have been conducted simulating chest thickness from 8 cm polymethyl methacrylate (PMMA) upwards (equivalent to 12 cm chest thickness), according to Rassow et al. 22, thus disregarding lesser thicknesses such as neonates, which may have a posterior-anterior thickness of about 6 cm 23. In addition, some of these studies have assessed image quality overlooking the effect of the antiscatter grid on spatial resolution and only analysing the low contrast parameters (contrast, signal-to-noise ratio (SNR), contrast-to-noise ratio, etc).
This article offers practical information to help pediatric cardiologists with the decision to remove the antiscatter grid. A detailed experiment with a dedicated biplane pediatric cardiology X-ray system has been used. Results have been obtained using a test object (TO) and different thicknesses of PMMA to simulate several patient sizes, analyzing the improvements in image quality and the increase in entrance surface air kerma (ESAK) 24 when the antiscatter grid is used.
MATERIALS AND METHODS
An interventional biplane X-ray system (Siemens Axiom Artis BC), equipped with two image intensifiers and customized for pediatric interventional cardiology procedures, was used for the measurements. The system was characterized using the protocols agreed upon the DIMOND and SENTINEL European programmes 12, 25. Different thicknesses of pediatric patients were simulated with PMMA plates of 25 cm × 25 cm x 0.5 cm (or 1 and 2 cm). A TO (Leeds TOR 18-FG) 26 has been used to evaluate image quality. The TO contains 18 low-contrast circles each with varying metal thickness and exponential decreases between them. In addition, it includes a standard metal bar pattern in the centre, to measure the high-contrast spatial resolution, with 21 series of bars in which the resolution goes from 0.5 to 5 line-pairs/mm. The TO was positioned at the middle of the PMMA thickness and at the isocentre, to evaluate image quality throughout the dose measurements, simulating real clinical conditions. Thus, the table height was decreased as the PMMA thickness increased to always have the TO at the isocentre. The image intensifier was always positioned 5 cm from the PMMA last plate, as in clinical working conditions with patients.
A dosimetry system Unfors Xi (model 8201010-A), with a solid-state detector (model 82020030-AXi) 27 in contact with the PMMA plates was used to measure incident air kerma 19. The detector was placed inside the radiation field but in the periphery avoiding the AEC central area. A backscatter (BS) factor of 1.3 24 was used to calculate ESAK from the measured incident air kerma and to estimate patient entrance doses during clinical procedures, for easy comparison of our results with other published values. Measurements were made with and without the antiscatter grid (Siemens model number 05660217) with 17:1 grid ratio, 70 lines per cm, and 100 cm focal distance (see Fig. 1). Images were recorded simultaneously with dose measurements. The dosimeter used was duly calibrated, traceable to official calibration laboratories.

Experimental arrangement for measurement with and without antiscatter grid.
The distance from the Unfors Xi solid-state detector to the X-ray focus was 74 cm when the phantom of 4 cm PMMA was used. For 8, 12, and 16 cm PMMA, this distance was reduced 2, 4, and 6 cm, respectively, to maintain the TO at the isocentre. Measurements were made for the three available fluoroscopy modes (low, medium, and high dose (10 pulses s−1) and for cine mode (30 frames s−1) using a field of view (FOV) of 22 cm. The evaluated procedure protocols in the system used for the experiment were [according to the Siemens nomenclature based on the weight, which establishes the scale newborn (<5 kg), infant (5 to <15 kg) and child (>15 kg)], to cover all patient sizes in the pediatric hospital.
A total of 32 series of images for cine and fluoroscopy were archived in DICOM format in 512 × 512 pixels and 8 bits, to evaluate image quality changes when the antiscatter grid is used or removed for the different operation conditions.
Osiris software, version 4.18 28, was used to evaluate the images with a computer having an IBM Corporation Intel[R] Pentium[R] M processor 29. The evaluation of image quality was always performed on three images (numbers 10, 12, and 15 of the series) and mean values and maximum deviations from the mean are reported. The initial images demonstrate varying image quality until the AEC stabilizes the X-ray tube output.
To evaluate image quality the following numerical parameters were used: SNR and high contrast spatial resolution (HCSR) for evaluation of low-contrast and spatial resolution, respectively. Moreover, two figures of merit (FOM) which indicate the necessary dose (ESAK) to obtain a certain image quality (FOM1 using the SNR2 and FOM2 using the HCSR2 parameter) have been used 12, 30-32.
To compare the image quality parameters from the two groups of images (with and without antiscatter grid), we used a Wilcoxon-Mann-Whitney rank sum test using the software SPSS 33. This nonparametric comparison procedure tests hypotheses about differences between two independent populations that are not necessarily distributed normally. Values of P < 0.05 were considered statistically significant.
RESULTS
Table 1 shows the most relevant radiographic parameters adjusted by the X-ray system with and without antiscatter grid for all the evaluated acquisition modes and available pediatric protocols.
| Exam protocol | Acquisition mode | Frames (s−1) | PMMA | With antiscatter grid | Without antiscatter grid | ||||
|---|---|---|---|---|---|---|---|---|---|
| Tube potential (kVp) | Tube current (mA) | Filter (mm Cu) | Tube potential (kVp) | Tube current (mA) | Filter (mm Cu) | ||||
| Newborn | LFM | 10 | 4 | 68 | 15 | 0.9 | 62 | 15 | 0.9 |
| MFM | 10 | 75 | 15 | 0.9 | 68 | 15 | 0.9 | ||
| HFM | 10 | 58 | 73 | 0.9 | 58 | 44 | 0.9 | ||
| CIM | 30 | 52 | 96 | 0.2 | 51 | 81 | 0.3 | ||
| Infant | LFM | 10 | 8 | 77 | 15 | 0.9 | 68 | 15 | 0.9 |
| MFM | 10 | 77 | 21 | 0.9 | 76 | 15 | 0.9 | ||
| HFM | 10 | 58 | 143 | 0.9 | 58 | 75 | 0.9 | ||
| CIM | 30 | 61 | 242 | 0.3 | 59 | 283 | 0.6 | ||
| Child | LFM | 10 | 12 | 77 | 22 | 0.9 | 75 | 15 | 0.9 |
| MFM | 10 | 77 | 32 | 0.9 | 77 | 19 | 0.9 | ||
| HFM | 10 | 66 | 72 | 0.6 | 58 | 126 | 0.9 | ||
| CIM | 30 | 67 | 314 | 0.3 | 63 | 307 | 0.6 | ||
| Child | LFM | 10 | 16 | 77 | 34 | 0.9 | 77 | 19 | 0.9 |
| MFM | 10 | 77 | 50 | 0.9 | 77 | 28 | 0.9 | ||
| HFM | 10 | 66 | 137 | 0.6 | 66 | 59 | 0.6 | ||
| CIM | 30 | 70 | 365 | 0.1 | 67 | 246 | 0.3 | ||
- LFM, low fluoroscopy mode; MFM, medium fluoroscopy mode; HFM, high fluoroscopy mode; CIM, cine mode.
ESAK and numerical values of image quality parameters obtained with and without antiscatter grid for all the evaluated acquisition modes and exam protocols are shown in Tables 2 and 3.
Figure 2 shows one example of two images (with and without antiscatter grid) of the TO, used to assess the different numerical parameters to evaluate image quality (e.g., FOM1 and FOM2). These images correspond to the experimental setting in cine mode for 16 cm of PMMA.
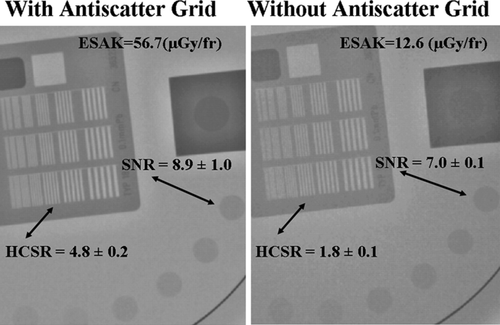
Comparison of two images obtained with and without antiscatter grid, for cine mode and for 16 cm of PMMA.
DISCUSSION
Deterministic effects (tissue reactions) and stochastic effects (carcinogenetic and genetic effects) in patients should be considered as part of the interventional cardiology practice 34. Avoiding expression of the first type and minimizing the probability of occurrence of the second type demand the application of the principle ALARA (as low as reasonably achievable) 4. Chambers et al. suggested several strategies to reduce radiation exposure to the patient, by implementing a radiation safety program for the catheterization laboratory 35.
A detailed analysis of image quality parameters should be made to justify the dose increase when using antiscatter grid in pediatrics during a clinical procedure. The decision to use or remove the antiscatter grid, should be based considering the weight and size of the patient and the requirements in image quality, depending on the pathology. In our research, we used the conversion factor (body dimension/phantom thickness) defined by to Rassow et al. 22, according to this, the simulated chest dimensions were 6, 12, 18 and 24 cm. For patients with body dimensions equal to 6 cm it would correspond an age range up to 0.5 years old. Patients with PA dimensions of 7, 8, 10 and 11 cm correspond to ages of 2, 3, 4 and 5 years old. Therefore, according to Table 2.9 of ICRP 89 36, patients of 0.5, 2, 3, 4, and 5 years, would correspond to approximate weights of 7, 14, 16, 17, and 19 kg.
| Exam protocol (acquisition mode) | PMMA | ESAK (μGy/fr) with AG | ESAK (μGy/fr) without AG | P | SNR (circle 1) with AG | SNR (circle 1) without AG | P | HCSR (7th group) with AG | HCSR (7th group) without AG | P |
|---|---|---|---|---|---|---|---|---|---|---|
| Newborn (LFM) | 4 | 0.14 | 0.08 | 0.13 | 3.6± 0.4 | 3.6 ± 0.4 | 0.77 | 4.4 ± 0.3 | 3.6 ± 0.1 | 0.15 |
| Newborn (MFM) | 4 | 0.27 | 0.14 | 3.8 ± 0.3 | 3.9 ± 0.4 | 3.8 ± 0.6 | 2.9 ± 0.5 | |||
| Newborn (HFM) | 4 | 0.55 | 0.26 | 6.9 ± 0.2 | 5.6 ± 0.2 | 5.9 ± 0.1 | 4.5 ± 0.1 | |||
| Newborn (CIM) | 4 | 2.47 | 1.15 | 11.2 ± 0.5 | 10.2 ± 0.7 | 9.8 ± 0.2 | 6.3 ± 0.1 | |||
| Infant (LFM) | 8 | 0.32 | 0.16 | 0.04 | 2.6 ± 0.4 | 2.6 ± 0.1 | 0.42 | 2.7 ± 0.7 | 2.1 ± 0.8 | 0.01 |
| Infant (MFM) | 8 | 0.68 | 0.30 | 3.0 ± 0.4 | 2.8 ± 0.2 | 3.8 ± 0.1 | 1.9 ± 0.2 | |||
| Infant (HFM) | 8 | 1.60 | 0.62 | 6.7 ± 0.6 | 4.7 ± 0.4 | 6.4 ± 0.6 | 3.5 ± 0.5 | |||
| Infant (CIM) | 8 | 7.87 | 2.54 | 11.9 ± 0.7 | 8.9 ± 0.5 | 6.3 ± 0.2 | 3.4 ± 0.1 | |||
| Child (LFM) | 12 | 0.79 | 0.29 | 0.04 | 2.2 ± 0.2 | 2.4 ± 0.3 | 0.56 | 2.9 ± 0.2 | 1.1 ± 0.4 | 0.01 |
| Child (MFM) | 12 | 1.64 | 0.59 | 3.1 ± 0.1 | 2.8 ± 0.1 | 2.6 ± 0.5 | 1.1 ± 0.3 | |||
| Child (HFM) | 12 | 3.52 | 1.39 | 4.6 ± 0.1 | 4.1 ± 0.1 | 4.6 ± 0.3 | 2.6 ± 0.5 | |||
| Child (CIM) | 12 | 15.7 | 4.65 | 9.1 ± 0.5 | 7.0 ± 0.4 | 5.2 ± 0.1 | 2.4 ± 0.0 | |||
| Child (LFM) | 16 | 1.71 | 0.64 | 0.04 | 2.6 ± 0.4 | 1.8 ± 0.1 | 0.17 | 3.0 ± 0.5 | 0.8 ± 0.2 | 0.01 |
| Child (MFM) | 16 | 3.78 | 1.32 | 2.8 ± 0.5 | 2.2 ± 0.4 | 2.6 ± 0.4 | 1.1 ± 0.3 | |||
| Child (HFM) | 16 | 8.73 | 2.77 | 4.7 ± 0.2 | 3.3 ± 0.1 | 4.5 ± 0.4 | 1.7 ± 0.4 | |||
| Child (CIM) | 16 | 56.7 | 12.6 | 8.9 ± 1.0 | 7.0 ± 0.1 | 4.8 ± 0.2 | 1.8 ± 0.1 |
- LFM, low fluoroscopy mode; MFM, medium fluoroscopy mode; HFM, high fluoroscopy mode; CIM, cine mode.
In Table I, the radiographic parameters (kVp and mA) adjusted by AEC, were greater, as expected with the use of antiscatter grid. Knowledge of radiographic parameters e.g., nominal focal spot size, kVp, mA, pulse time, filtration, focus-patient distance or detector-patient distance are necessary because of their considerable impact on image quality and on the dose imparted throughout the procedure.
The necessary increments in ESAK, when antiscatter grid is used, are very different depending on the acquisition mode and the corresponding selected acquisition protocol. For 4 cm of PMMA the use of antiscatter grid requires a dose per frame 75% higher for low fluoroscopy mode and a dose increase of 115% for cine mode. These increases are greater using 16 cm of PMMA in low fluoroscopy mode (167%) and substantially higher for cine mode (351%) (see Table 2). The increase in the values of ESAK when using antiscatter grid is known as Bucky factor (BF). The averages BF measured during this experiment were 1.99 (4 cm of PMMA), 2.49 (8 cm of PMMA), 2.85 (12 cm of PMMA), and 3.30 (16 cm of PMMA), respectively. These results are similar to those reported by Onnasch et al. 8.
Table 2 also shows that when using antiscatter grid, SNR variations do not appear significantly important and it reaches an average increase of 14%. Partridge et al. 17 state that the improvement of the reported SNR by Onnasch et al. 14, which reaches a 27%, is considered to be a debatable advantage in justifying the use of antiscatter grid for all type of patients. Changes in HCSR are more evident with the use of antiscatter grid (as could be expected) especially for cine mode. When using these values of HCSR as “relative” criteria, the image quality improvement ranges from 56%, in the case of 4 cm of PMMA, to 167% for 16 cm of PMMA. When applying the statistical U Mann–Whitney test for the two data sets (with and without antiscatter grid), the differences for SNR and HCSR were not always significant. For example, the differences found for SNR were not statistically significant in any of the four thicknesses of PMMA studied. However, for HCSR, the parameter associated with the ability to see small blood vessels, was statistically significant for 8, 12, and 16 cm of PMMA.
For fluoroscopy modes the increases on ESAK are not significantly high in comparison with cine mode, but obviously it is not practical in clinical practice to remove the antiscatter grid in fluoroscopy and include the antiscatter grid for cine series. Thus, the FOM1 defined from the SNR (Table 3) does not seem useful in deciding whether or not to use the antiscatter grid, as FOM1 values were always higher for the measurements without antiscatter grid. However, FOM2 defined from HCSR gives the best results to recommend whether or not to use antiscatter grid. For 4 and 8 cm of PMMA, it does not seem reasonable to use antiscatter grid with the settings applied in this X-ray system, at least for LFM, but for 12 and 16 cm, the improvement in image quality was considerable and statistically significant in all acquisition modes. Observing the differences in quality in Fig. 2 with the images obtained at 16 cm of PMMA, with and without antiscatter grid, one can acceptably judge the quality of both images, but the numerical assessment of image quality reveals clearly the advantage of that obtained with antiscatter grid, particularly for the parameter HCSR, which was used to define the FOM2.
| Exam protocol (acquisition mode) | PMMA | FOM1 (circle 1) with AG | FOM1 (circle 1) without AG | P | FOM2 (7th group) with AG | FOM2 (7th group) without AG | P |
|---|---|---|---|---|---|---|---|
| Newborn (LFM) | 4 | 92 ± 20.1 | 167.9 ± 43.7 | 0.01 | 134.4 ± 16.4 | 169.7 ± 8.0 | 0.64 |
| Newborn (MFM) | 4 | 53.1 ± 11.7 | 104.2 ± 18.3 | 54.0 ± 16.1 | 59.1 ± 19.7 | ||
| Newborn (HFM) | 4 | 84.7 ± 7.5 | 117.8 ± 7.9 | 62.3 ± 2.6 | 77.7 ± 2.4 | ||
| Newborn (CIM) | 4 | 50.4 ± 6.8 | 90.8 ± 11.9 | 39.2 ± 1.5 | 34.2 ± 0.9 | ||
| Infant (LFM) | 8 | 21.3 ± 6.4 | 42.4 ± 2.7 | 0.01 | 23.2 ± 14.1 | 30.3 ± 26.8 | 0.27 |
| Infant (MFM) | 8 | 13.8 ± 3.4 | 26.6 ± 4.3 | 20.8 ± 1.0 | 12.1 ± 1.9 | ||
| Infant (HFM) | 8 | 28.0 ± 4.8 | 34.9 ± 8.3 | 25.7 ± 4.4 | 20.0 ± 5.8 | ||
| Infant (CIM) | 8 | 18.0 ± 2.8 | 31.1 ± 5.4 | 5.1 ± 0.3 | 4.6 ± 0.3 | ||
| Child (LFM) | 12 | 6.0 ± 0.8 | 20.4 ± 4.8 | 0.01 | 10.7 ± 1.9 | 4.8 ± 3.6 | 0.07 |
| Child (MFM) | 12 | 5.8 ± 0.5 | 13.1 ± 2.2 | 4.1 ± 1.5 | 2.2 ± 1.1 | ||
| Child (HFM) | 12 | 6.0 ± 0.4 | 12.0 ± 1.3 | 6.1 ± 0.7 | 4.9 ± 1.9 | ||
| Child (CIM) | 12 | 5.2 ± 1.2 | 10.6 ± 5.9 | 1.7 ± 0.1 | 1.2 ± 0.1 | ||
| Child (LFM) | 16 | 3.9 ± 1.7 | 4.9 ± 1.3 | 0.01 | 5.2 ± 1.7 | 1.0 ± 0.3 | 0.01 |
| Child (MFM) | 16 | 2.1 ± 1.0 | 3.6 ± 1.1 | 1.7 ± 0.5 | 1.0 ± 0.5 | ||
| Child (HFM) | 16 | 2.5 ± 0.3 | 4.0 ± 0.4 | 2.3 ± 0.4 | 1.0 ± 0.6 | ||
| Child (CIM) | 16 | 1.4 ± 0.3 | 3.9 ± 0.4 | 0.4 ± 0.1 | 0.2 ± 0.1 |
- LFM, low fluoroscopy mode; MFM, medium fluoroscopy mode; HFM, high fluoroscopy mode; CIM, cine mode.
As a complement, Fig. 3 shows two images with and without antiscatter grid corresponding to real patients of similar characteristics and pathology. In both cases, image quality is enough to perform a good diagnosis of the persistent ductus arteriosus (diameter and length), allowing the proper selection of the device to be implanted. Nevertheless, the procedure without antiscatter grid in comparison to the image of the patient using antiscatter grid resulted on a dose saving of a ∼50%.
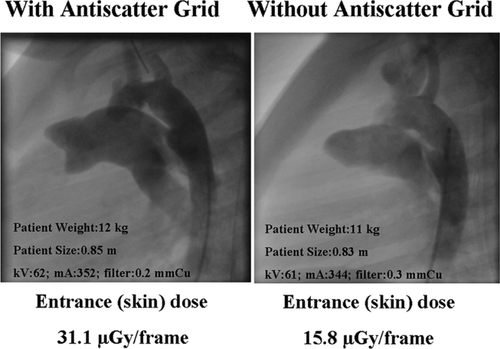
Comparison of two images of real patients obtained with and without antiscatter grid, for cine mode.
CONCLUSIONS
The antiscatter grid produces significant improvements in image quality with a sustained increase in patient radiation dose for children with chest thicknesses greater than 12 cm (equivalent to 8 cm of PMMA) corresponding approximately of 5 years old and 19 kg weight. Avoiding the use of antiscatter grid seems advisable for all neonate and very young children, whose structures are extremely small (chest thicknesses equal or less than 6 cm, or weight less than 6 kg). However, in all cases, criteria of the clinicians, and particular conditions of same patients should be taken into account before removing the antiscatter grid if a high image quality was necessary to obtain.