Three-dimensional adipofascial and dermal structures involved in forehead crease formation
Abstract
Deeply etched forehead creases indicate aging. Various treatments such as filler injections, fat grafting, and facelift surgery are used to remove them. However, knowledge of the anatomical structures associated with subcutaneous tissue changes and the superficial musculoaponeurotic system is lacking, and there is no consensus about the appropriate treatment. We have investigated the subcutaneous structures involved in forehead creases; this will help to establish selection criteria for improved treatment. The forehead sections of five unfixed adult Asian cadavers were obtained. Tissues containing forehead creases were removed from the periosteum and were examined using gross observation, radiography, histology, and nano-computed tomography. All methods revealed that the dermis in the skin crease area, namely the fold visible from the body surface, was bound to the frontalis muscle by a three-dimensional fibrous structure between the fatty septa. This structure was dense near the skin folds and sparse and thin in other areas. In particular, it was tightly bound to the dermis immediately below the crease, with collagen fibers traversing toward the epidermis. In addition, there were fewer skin appendages near the crease than in the normal area, or they were absent altogether; the epidermis was thicker, and the dermal papillae were more developed. It is thought that the density and firmness of the fibrous fatty septal structures between the dermis-frontalis muscle and the specific structures of the epidermis and dermis immediately below the crease account for the characteristic plastic forehead creases.
1 INTRODUCTION
Age-related skin changes are associated with the initiation or exacerbation of cosmetic disorders characterized by developing skin creases and sagging. These changes significantly affect quality of life in older people (Mallouris et al., 2016). Facial creases and sagging are caused by age-related changes: thinning of the epidermis, loss of skin elasticity, and atrophy of the fat compartment owing to loss of muscle traction and facial bone mass (Cotofana et al., 2016; Shaw et al., 2011). Currently, interest in rejuvenating the appearance through restoring age-altered facial features to their former state is increasing worldwide (Wong & Mendelson, 2015). Understanding the anatomical structures involved in age-related crease enhancement is vital for such rejuvenation.
Various studies have been conducted to explain frontal creases. Such creases cover the frontal bone, and their pattern is nearly horizontal (Carruthers & Carruthers, 2010; Hadi & Wilkinson, 2017). Facial skin changes have been described, emphasizing the subcutaneous fat compartment and its alterations (Gierloff et al., 2012; Wan et al., 2014). Histologically, these changes have been attributed to loss of skin elasticity, epidermal thinning, slowing of cell division in the stratum germinativum, and flattening of the epidermal-dermal interface. However, those causes are characteristic of “wrinkles” rather than “creases” (Kruglikov et al., 2016).
Also, a recent study of the anatomy of facial creases revealed none of the morphological changes in superficial musculoaponeurotic system (SMAS) architecture that could account for the development of such creases. The authors concluded that the forehead fold was a cutaneous depression caused by interacting aging-related dermal-skeletal-muscular changes without SMAS architectural predilections (Sandulescu et al., 2019). Consequently, our understanding of frontal muscle contraction, and the frontal creases that become more prominent with aging, is inadequate.
Various techniques have been developed to reduce forehead creases, including hyaluronic acid and fat injections to augment volume (Kapoor et al., 2021; Schultz et al., 2020), facelift surgery (Guyuron & Lee, 2014), and suppression of frontalis muscle movement with botulinum toxin injections (Zhang et al., 2020). Hyaluronic acid is frequently used for skin rejuvenation because of its minimally invasive nature and simplicity. It is injected into various layers including the intradermal, shallow fat, deep fat, SMAS, and intramuscular layers (Tadano et al., 2021). Understanding the exact anatomy and physiological mechanisms underpinning the formation of forehead creases will help to determine the indications for those treatments and will increase awareness of the layers of skin to be used.
In addition to histological observations using radiography and Azan stains, nano-computed tomography (CT) was used in this study to elucidate the finer details of the three-dimensional (3D) structure of the subcutaneous fibrous tissue. We hypothesized that there is a structure specific to the crease area anchoring the skin to the fascia because (1) a forehead crease forms in conjunction with the frontalis muscle, (2) the area is constant, and (3) the same wrinkle does not migrate. Finally, we clarified the mechanism of this dynamic crease formation through a detailed analysis.
2 MATERIALS AND METHODS
2.1 Samples and ethical consideration
Autopsies were performed on five unfixed Japanese cadavers (aged 69–95 years at death). Three samples were taken from each donor body to examine the crease, between the creases, and crease-free areas. The cadavers used were donated to the Keio University School of Medicine with the consent of the bereaved families. All studies followed the “Guidelines for Autopsy of Cadavers in Clinical Medicine Education and Research” of the Japan Surgical Society and the Japanese Society of Anatomy. This work was approved by the Keio University Medical Research Ethics Committee (approval number: 2021-1064). Specimens with creases on the forehead area were selected visually. Specimens with visible wounds or tissue injury at the donor site or a history of head and neck surgery or irradiation were excluded. All autopsies were performed by the first author alone. The sagittal section of the forehead skin tissue on the periosteum was obtained with the area that covered the deeper hairline, frontal bone, and upper eyebrows.
2.2 Radiography
The frontal tissue was dissected from the head under the periosteum within the hairline, frontal bone, and above the eyebrows. The tissue was sectioned vertically (3 mm width) with a blade. In addition to gross observation, x-ray irradiation for 4 min was used to image fascial structures using a soft tissue x-ray irradiator (SOFTEX; Softec Co, Tokyo, Japan; 30 kVp, 10 mA).
2.3 Histology
A 1 cm × 2 cm × 1 cm tissue block containing the skin, subcutaneous tissue, and frontal muscles was dissected and embedded in paraffin. A continuous section in the vertical plane of a prominent frontal, central crease was cut to a thickness of 5 μm. All sections were collected, and every 10th section was stained with Azan. They were photographed using a NanoZoomerXR C12000 (Hamamatsu Photonics K.K., Shizuoka, Japan).
2.4 Nano CT imaging and 3D reconstruction
Nano CT uses a transmission x-ray tube with a resolution in the submicron range, allowing fine structures such as fascia and fat septa to be observed, which is not feasible with micro CT (Contet-Audonneau et al., 1999). The crease in the center of the frontal forehead and the crease-free area (1 mm width) were cut vertically around the crease and imaged using nano CT (nano3DX [Rigaku, Tokyo, Japan]). The images were reconstructed into 3D by IMARIS software (Carl Zeiss AG, Oberkochen, Germany).
3 RESULTS
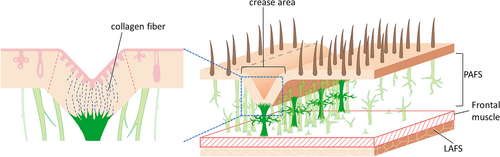
Gross observation and radiographic images of the crease area showed wide, white fibers in the fatty septum from just below the dermis to the frontalis muscle. These fibers were denser around the crease area than in other areas. They were observed in areas without creases, but their density was lower, and some areas were disconnected up to the middle layer of fat, indicating a fibrous structure (Figure 1).
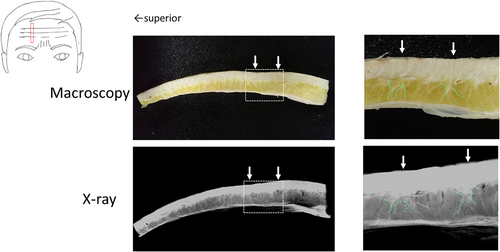
Three areas were observed in the tissue image with Azan staining: (1) the area where the skin depression line could be recognized visually, (2) the area between the depression lines, and (3) the area taken from the range where no depression line was visible. First, under low-power magnification, area (1) had the most histologically depressed crease line, consistent with visual observation. In the area 5–7 mm on both sides of this line, a dense fibrous structure ran longitudinally through the subcutaneous fat layer and there was clear continuity from the frontal fascia to the dermis, as observed on radiography; some also branched horizontally. Beyond this zone, as outside of (1) or in (2), there was a greater distance between the fibrous structures, the fibers within the structure were less dense, and there was less horizontal branching, so the structure was less adhesive. In the area with no depression line (3), the fibrous structures showed continuity with the dermis but poor continuity with the frontalis muscle and were sparse in the fatty middle layer, so the tissue was more fragile.
Furthermore, the dermis of the forehead area is very rich in skin appendages; however, an area approximately 1 mm on each side across the crease line was devoid of skin appendages such as hair follicles, sweat glands, and sebaceous glands. This area was named the crease area.
Magnification of the boundary between the dermis and the subcutaneous fat layer revealed fibrous tissue bound to the dermis in both areas; however, the form of this binding differed between the areas (Figure 2B). In the crease area, the fibrous tissue adhered to the lower dermis in a planar manner and encroached irregularly into the dermis thanks to the absence of dermal appendages. However, outside the crease area, the fibrous tissue was fragmented by the appendages and only linearly attached to the dermis.
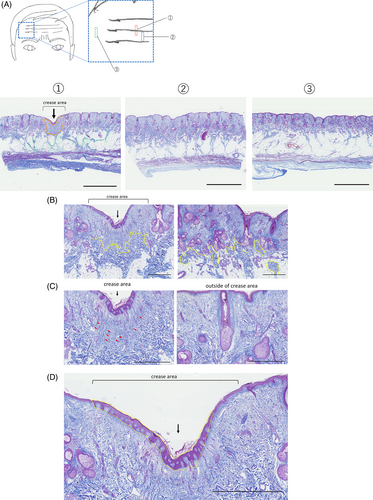
Further magnification of the dermis's internal structure revealed that fibrous structures penetrated it, and collagen fibers ascended through the dermis to near the epidermis (Figure 2C). On the other hand, except in the crease area, collagen fibers were randomly oriented in the dermis and no ascending fibers were observed. In the crease area, the epidermis was thick and the dermal papillae were well-developed (Figure 2D).
Therefore, the characteristics of the fold structure recognized visually as a depressed line in the forehead include: (1) fibrous structures that are intricately connected to the dermis just below the fold, or crease line, and to the frontalis muscle, (2) differences in the density of fibrous structures connecting the dermis to the frontalis muscle between the crease area and other areas, (3) epidermis thickening in the crease area, development of dermal papillae and collagen fibers running longitudinally in the dermis, and (4) absence of dermal appendages including hair follicles, sweat glands, and sebaceous glands in the crease area.
However, it is difficult to determine the continuity of these fascial structures because of the constant direction of sectioning and the lower limit on thickness of one section in the tissue image. Therefore, we observed the continuity of subcutaneous structures related to creases by nano CT imaging of the frontal tissue in crease and non-crease areas.
The dermis and deep fascia of the skin depressions were connected by fibrous structures of the septa at multiple points (Figure 3A,B). This structure was also confirmed to be thin layered and formed by three-dimensional fusion and dispersion of the septa. In contrast, in subcutaneous areas without clear depressions, there were septal structures between adipose tissues, but no structures connecting the dermis to the deep fascia were identified (Supporting information Figure S1A,B).
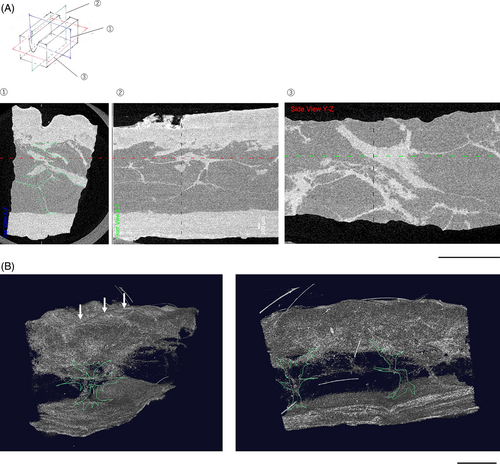
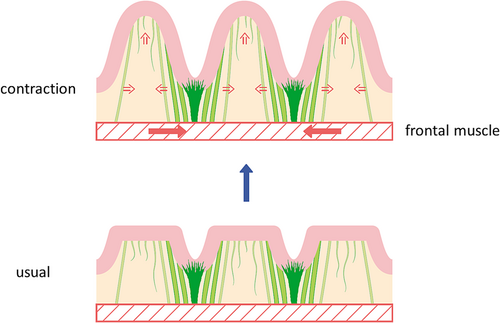
Consistent with the histological findings and CT images, numerous fibrous structures run longitudinally in the adipose tissue from the dermis to the frontalis muscle in the vicinity of the depression in the frontal crease, or crease area. Especially just below the depression, in the crease line, firm fibrous tissue is deeply embedded in the dermis. The difference in density of these fibrous structures from outside the crease area and the difference in collagen fibers in the dermis can be characterized as creases (Figure 4). However, these structures were not continuous in the creases, but were fuzzy structures that repeatedly dispersed and fused.
4 DISCUSSION
The aim of this study was to reveal the detailed three-dimensional anatomy of the subcutaneous tissue involved in the creases on the forehead, which are prominent and progressively more noticeable signs of aging. We predicted that an anchoring structure in the layers deep to the dermis in the wrinkle area would form creases in a fixed position, along with contraction of the frontalis muscle. Our results indicate that in the subcutaneous region near the crease, a fibrous structure traverses the dermis and adipose tissue and extends into the frontalis muscle. Previous studies have attributed frontalis wrinkles to changes in the skin, such as decreased elastin, tropoelastin, and collagen VII in the dermis and epidermal thinning (El-Domyati et al., 2014; Fujimura et al., 2007). However, those factors are specific causes for “wrinkles” and do not adequately explain “crease” formation by the contraction of the frontalis muscles. There is no deformation of the SMAS in the crease area. Since the increase in forehead creases with aging has been attributed to the activation of compensatory movements of the frontalis muscle in response to the progression of age-related upper eyelid ptosis (Knoll et al., 2008), there is still no clear explanation for the linkage with the frontalis muscle (Sandulescu et al., 2019).
Our results revealed a new crease-specific fibrous structure within the subcutaneous adipose tissue. Furthermore, we found that this structure within the forehead area differs in fiber density between the crease area, outside the crease area, and crease-free areas. In particular, the subcutaneous fat of the forehead is divided into three compartments (Rohrich & Pessa, 2007), and this structure in the central fat compartment from the nasal dorsum to the frontal information could account for the formation of creases in the central frontal area. SMAS in the frontal region is a general term for this structure. In our previous report, we classified the whole body's subcutaneous fat into protective adipofascial system (PAFS) and lubricant adipofascial system (LAFS); PAFS is the area between the dermis and the frontal muscles of the frontal region (Nakajima et al., 2004). In other words, bordering the facial muscles, the shallow layer is PAFS and the deep layer is LAFS. The facial muscles adhere to the skin via the PAFS, which allows muscle movements to be transmitted to the skin. The LAFS also allows the facial muscles to move well, resulting in a congruent structure. The fibrous structure observed in this study that joins the dermis to the frontalis fascia is the fatty septum within the PAFS, confirming that it is responsible for transmitting frontal contractions to the skin.
There have been similar reports of this layered structure in recent studies (Ingallina et al., 2022). However, it is crucial to recognize that although this fibrous structure within the PAFS was relatively clear in our observations, these tissues are continuous with fibers of the dermis, deep fascia, and frontalis muscle, ambiguous structures that repeatedly disappear and fuse. It was hypothesized that the difference in fiber density between the area of the crease and the area outside the crease results in a difference in the transmission of frontalis muscle contraction to the skin. As a result, only the crease area is strongly anchored to the subcutaneous bed and is concave. In contrast, the area with sparse subcutaneous structure is more mobile, causing the skin to rise so the characteristic forehead creases appear only in specific locations (Figure 5).
We previously described a septal structure within the adipose tissue in the inframammary fold (Takaya et al., 2022). This is a multi-layered fuzzy septal structure that fused and dissociated within the adipose tissue from the pectoralis major fascia at the level of the fourth and fifth ribs, extending to the folds, where it branched and joined finely near the dermis, so the skin hung down. Similar to the macroscopic structure of the fascia, the small creases in the forehead also contain fibrous structures that connect the dermis to the fascia, further subdividing and connected at the microscopic level within the dermis in an epidermal direction.
The dermis in the crease areas has no skin appendages such as hair follicles, sweat glands, and sebaceous glands; multiple collagen fibers traverse into the dermis, and the septal structures penetrate deeply from the deep dermis to the shallow layers. In previous studies, creases were reported to be mechanical phenomena in which the mismatch of mechanical modules between adjacent epidermal-dermal or dermal-subcutaneous junctions leads to structural instability within the skin (Kruglikov & Scherer, 2018). In other words, they were considered a state of tissue folding with decreased thickness due to the reduction of ECM, dermal cells, and adipose tissue, forming a rigidly stratified epidermis (Varani et al., 2006). Tension is generated in the stiff skin, increasing cell activity and ECM synthesis (Hsu et al., 2018). In addition, epidermis-specific removal of integrins or focal adhesion kinase (FAK), which is involved in mechanotransduction, deforms the follicles and dysregulates hair cycle propagation (Essayem et al., 2006). Therefore, it is suggested that abnormal skin hardening and tension in the anchorage area contributes to dermal appendage hypoplasia at the crease.
Clinically, during facelift surgery on anterior forehead creases, dissection over the subcutaneous frontalis muscle to above the eyebrows is recommended (Surek, 2019). This is consistent with the idea that the creases can be eliminated by destroying the anchoring structures observed in this study. In addition, subcutaneous injection with hyaluronic acid fillers is the first choice treatment for creases (Kapoor et al., 2021); some reports suggest that blocking against extreme muscle range of motion, and contraction of inhibitory muscles by injecting hyaluronic acid with awareness of subcutaneous bulkhead structures, can be effective (de Maio, 2018). Keeping in mind that creases are fibrous connective tissue structures that connect the dermis to the facial muscles within the PAFS, it would be better to inject into the shallow and deep subcutaneous layers, respectively, or to debride the subcutis bluntly at the time of injection to reduce the transmission of frontalis muscle contraction to the skin.
Since relatively old cadavers were used in this anatomical study, more studies are needed to determine age-related changes in this structure and to ascertain whether it is congenital or forms with age. In addition, more cadavers are needed to examine race, age, and sex differences.
5 CONCLUSION
The frontal crease is an ambiguous, multi-point, three-dimensional fibrous structure that connects the dermis just below the fold to the frontal fascia within the PAFS, which penetrates deeply into the dermis in the crease area. The absence of dermal appendages within the dermis in the region near the crease it is also characteristic. This ambiguous fibrous structure is thought to transmit contractions of the frontalis muscle to the dermis via the PAFS, forming plastic, deep creases. This finding could contribute to the selection and development of rejuvenation treatments that ameliorate frontal creases anatomically correctly.
ACKNOWLEDGMENTS
This study used cadavers donated to the Laboratory of Clinical Anatomy, Department of Anatomy, Faculty of Medicine, Keio University. In addition, the use of the Clinical Anatomy Laboratory, Department of Anatomy, Faculty of Medicine, Keio University, was approved.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, K.T., upon reasonable request.