Assessing Environmental Justice in Mexico: How Polluting Industries and Healthcare Disparities Impact Congenital Heart Defects
Funding: The authors received no specific funding for this work.
ABSTRACT
Background
Congenital heart defects (CHDs) are the most prevalent birth defects globally and the second leading cause of death in Mexican children under five. This study examines how industrial activity and social vulnerabilities independently and jointly influence CHD incidence across 2446 Mexican municipalities from 2008 to 2019.
Methods
Using negative binomial regression models, we evaluated associations between polluting industries, healthcare access, and CHD incidence. We analyzed these factors independently, jointly, and through interaction terms to assess potential effect modification by healthcare access. Incidence rate ratios (IRRs) and 95% confidence intervals were estimated across healthcare access strata.
Results
Municipalities without healthcare facilities were more likely to host polluting industries, highlighting structural inequities. The presence of polluting industries was associated with increased CHD incidence, even after adjusting for healthcare access. For instance, municipalities with poor healthcare access and two or more polluting industries exhibited a 42% higher CHD incidence (IRR = 1.42, 95% CI: 1.25–1.60) compared to a 26% increase in municipalities with better healthcare access (IRR = 1.26, 95% CI: 1.02–1.57).
Conclusions
These results show how environmental pollutant exposure and social vulnerabilities interact synergistically, disproportionately impacting socially vulnerable populations. Targeted policy interventions addressing both environmental pollution and healthcare inequities are crucial. Further research is also needed to clarify the mechanisms linking pollution to CHDs and to guide public health strategies aimed at reducing these disparities in Mexico.
1 Introduction
Mexico's industrial sector has been a keystone of its economic development, contributing substantially to employment and gross domestic product (GDP) growth (Bajpai 2023). Since 1980, industrial activities related to manufacturing, mining, and oil and gas production have contributed 25%–35% of Mexico's GDP (World Bank 2023). Such industrialization has led to severe environmental pollution, adversely impacting public health (Wu 2022). Key industries, such as chemical, petrochemical, automotive, and hazardous waste treatment plants, are major contributors to environmental pollution, and they are point sources for a variety of pollutants, including volatile organic compounds (VOCs), heavy metals, and particulate matter, which have all been linked to respiratory illnesses, cardiovascular diseases, and other serious health conditions (Blackman et al. 2010). Pollution intensity varies geographically, with some states having high pollutant generation relative to their output, like Chiapas, Guanajuato, and Veracruz (SEMARNAT 2010). In addition to adverse environmental exposures, access to healthcare is a critical determinant of public health outcomes.
Mexico's healthcare system comprises a mix of public and private providers, with initiatives such as Seguro Popular and the Instituto de Salud para el Bienestar (INSABI) aimed at expanding healthcare coverage (Reich 2020). Seguro Popular, a “publicly funded health insurance” launched in 2004, aimed to provide health insurance to the uninsured population, primarily benefiting low-income households (Garcia-Diaz et al. 2023). INSABI, introduced in 2020, seeks to achieve universal health coverage by offering free medical services and medications to all citizens (Reich 2020). Despite these efforts, disparities in access to quality healthcare persist, especially in rural and marginalized areas (Serván-Mori et al. 2023). These disparities have been shown to exacerbate the health impacts of environmental pollution, as affected populations often lack adequate medical care and preventive services (Bhatt and Bathija 2018).
Pregnant persons, developing fetuses, and children are especially vulnerable to the toxic effects of environmental exposures. Gestation is a uniquely vulnerable period of life in which all organs are developed, and as such, exposure to environmental toxicants increases the risk of various immediate and long-term health consequences, including congenital heart defects (CHDs), the most prevalent birth defects globally. The embryogenesis of the heart begins in the early stages of pregnancy. The heart starts to form around the third week of gestation and goes through different stages of development, including the formation of the heart tube, looping, and septation, which eventually lead to the development of the four chambers and the major blood vessels (Houyel and Meilhac 2021). Disruptions at any stage of this process can result in structural abnormalities (Erhardt et al. 2021). CHDs impose significant burdens on individuals, families, and healthcare systems (Reller et al. 2008), and they range in severity, with common types of CHDs being ventricular septal defect (VSD), atrial septal defect (ASD), tetralogy of Fallot, and transposition of the great arteries (Hoffman and Kaplan 2002). CHDs are often diagnosed through prenatal screening and postnatal examinations, and therefore, early detection requires unimpeded access to routine and specialized healthcare services throughout pregnancy and in early life. In Mexico, CHDs are a serious public health concern, as mortality has increased in recent years, with most deaths from CHD occurring in the neonatal period. In 2013, CHDs were responsible for 24% of infant mortality (Torres-Cosme et al. 2016).
Emerging evidence indicates that environmental exposures during gestation, including benzene, lead, and fine particulate matter (PM2.5), contribute to the etiology of CHDs (Padula et al. 2013). Other environmental epidemiologic studies have shown associations between residential proximity to hazardous waste sites and increased rates of CHDs (Geschwind et al. 1992; Malik et al. 2004). These findings similarly suggest that environmental pollutants, such as volatile organic compounds (VOCs) and heavy metals, may contribute to the development of CHDs. While the mechanisms through which these pollutants affect fetal heart development are not fully understood, they may involve oxidative stress, inflammation, and disruption of normal cellular signaling pathways (Vrijheid et al. 2011) as well as genetic and epigenetic modifications (Vecoli et al. 2016).
Given the compounding disparities related to adverse environmental exposures and lack of healthcare services, we sought to apply an environmental justice lens to understand and contextualize the public health problem of CHDs in Mexico.
2 Methods
2.1 Data Sources
2.1.1 Births and Birth Defects
The subsystem of information on births (SINAC) in Mexico is an information system developed by the federal government to integrate the information on live births that occurred in the country and the conditions of their birth, with the objective of supporting the protection of children's rights and the planning, assignment, and evaluation of the programs directed to the maternal-child population (Secretaria de Salud 2022).
The system requires children to be registered through it to obtain a birth certificate. It was established in 2008, and it is estimated to hold information for around 98% of the births that occurred since 2008 in both hospital and non-hospital settings (INEGI 2015).
SINAC passively collects data on birth defects, which are registered and codified using international ICD-10 codes. The data for SINAC from 2008 to 2022 was downloaded from the official government website, sorted by mother's municipality of residence, and classified according to EUROCAT'S classification by organ systems (Tables S1) (EUROCAT 2022). Only records from 2008 to 2019 were selected for the final model; we excluded data from 2020 to 2022 from the analysis after observing a trend of underreporting, even for congenital conditions with relatively stable prevalence, such as Down syndrome. This pattern suggested systematic issues with reporting rather than true declines in prevalence. We hypothesize that the COVID-19 pandemic may have contributed to these inconsistencies, potentially due to disruptions in healthcare services and reporting systems. Individuals who were registered with a known genetic syndrome were excluded from the database, as these have known genetic causes; preterm and late-term individuals were also excluded. Data from SINAC was also used to determine total births by municipality.
2.1.2 Polluting Industry Density
The Registro de Emisiones y Transferencia de Contaminantes (RETC) was established in 2004 and updated in 2013 (SEMARNAT 2013). The program seeks to inform communities about the quantity of contaminants that are transferred from industrial sites to water, air, or soil. The program regulates 200 substances, and reporting limits are established by law (NOM-165-SEMARNAT-2013). Industrial sectors designated as established sources are the chemical, petrochemical, paints, automotive, cellulose and paper, metallurgic, glass, electric energy generation, asbestos, cement, and hazardous residues treatment industries. Big generators of hazardous substances, defined as establishments that generate 10 tons or more of hazardous substances per year, as well as establishments discharging wastewater into national waters (SEMARNAT 2013). Although industries are required to report their emissions, RETC is not considered a regulatory database; rather, it is a public disclosure mechanism where industries self-report their emissions without validation by regulatory agencies (Chakraborti 2019). This self-reporting aspect introduces potential biases in our data. Industries may not adequately report their emissions, and some industries might not be included in the database.
Data from RETC was downloaded from the official website, and a database from 2008 to 2019 was generated. Polluting industries were aggregated by municipality, and the maximum number of industries by municipality was included in the final model. Industries were classified by the industrial sector depending on the national distribution among municipalities.
2.1.3 Sociodemographic Characteristics
The National Council for the Evaluation of Social Development Policy (CONEVAL) is a decentralized public organization of the Federal Public Administration, with autonomy and technical capacity to generate objective information on the situation of social policy and the measurement of poverty in Mexico, which allows for improved decision making in the matter (CONEVAL 2022). CONEVAL is responsible for issuing the guidelines and criteria for the definition, identification, and measurement of poverty using the information generated by the National Statistics and Geography Institute (INEGI). Importantly, CONEVAL uses a multidimensional approach to defining poverty by using multiple indicators including current income per capita; educational lag (delay in educational attainment); access to health services; access to social security; housing quality and spaces; access to basic services in housing; access to food; and degree of social cohesion. CONEVAL issues a report every 5 years on poverty in Mexico. With these variables, CONEVAL builds and publishes a measurement for multidimensional poverty that not only considers economic wellness but also considers social vulnerabilities to determine poverty (CONEVAL 2022). Data for lack of access to healthcare for 2015 by municipality was downloaded from the official website and added to the database. Excluded municipalities can be found on Table S3.
2.2 Statistical Analysis
We first evaluated the distributions of polluting industrial activities, noting a heavy right-skewed distribution. As such, we categorized all polluting industrial activities within a municipality as “none,” “one,” and “two or more.” We additionally categorized activities separately by activity type using the same aforementioned categories, except for the plastics industry which was operationalized as “none” or “at least one,” given its relative infrequency within municipalities. For ease of interpretation, we dichotomized healthcare inaccessibility at the overall median across all municipalities.
We calculated descriptive statistics of the distributions of polluting industries by healthcare access within municipalities, and we estimated polychoric correlations among polluting industries within municipalities, and then developed adjusted models to comprehensively examine the relationships of polluting industries with incidence rates of congenital heart defects and whether these associations were modified by healthcare access.
We evaluated the bivariate associations between industrial activity categories and dichotomous healthcare inaccessibility using frequency tables, with statistical significance determined by Fisher's exact tests. We used Fisher's exact tests over 𝛘2 tests since some combinations of industrial activity and healthcare inaccessibility had low sample sizes. We also estimated the polychoric correlations between all pairwise combinations of industrial activity categories. Polychoric correlations were chosen because they are particularly suited for assessing the relationships between ordinal variables derived from categorical data, especially when those variables are theorized to represent underlying continuous distributions (Roscino and Pollice 2006).
To evaluate the associations of polluting industrial activities and healthcare inaccessibility with CHD incidence rates, we used negative binomial regressions to account for the overdispersion we found within our data. This modeling approach was chosen because it accounts for overdispersion in count data (Hilbe 2011). In these models, the total count of CHD-affected births in a municipality (over the study time period) was the outcome while we used the total number of births within a municipality (over the study time period) as an offset term, which provided a birth-rate standardized estimate of incidence rate ratios (IRRs) and 95% confidence intervals (95% CIs). We evaluated a series of four stepwise models that included only healthcare inaccessibility (Model 1), polluting industrial activities only (Model 2), both healthcare inaccessibility and polluting industrial activities (Model 3), and the interaction between them (Model 4). We used the p-value of the interaction term as an overall indicator of effect measure modification (EMM), using a p-value of 0.20 as a threshold to rule in statistical modification. To help contextualize the interaction, we estimated healthcare inaccessibility strata-specific IRRs within categories of polluting industrial activities, and we calculated Wald-type p-values for these strata-specific associations along with 95% CIs. For all models, we used Huber-White robust variance estimation.
All analyses were conducted using Stata version 15.1 (StataCorp LLC. College Station, TX, USA).
2.3 Ethical Considerations
The study was submitted to The George Washington University IRB and was issued a determination of non-human subject research; all data used for the project is retrospective and publicly available (NCR235079).
3 Results
3.1 Descriptive Analysis
3.1.1 Population Characteristics
The study included data from 2446 municipalities out of the 2454 total municipalities recognized in 2015. Municipalities are the smallest geographic division of the Mexican territory. Eight municipalities were excluded from the final models due to a lack of access to healthcare data (Table S2). The number of births varied significantly, with some municipalities having as few as 36 births over the 12-year span of the study, while others exceeded 100,000 births in this timeframe. The median percentage of people without access to healthcare was 13%, with a range from 3% to 35%.
The distribution of reported congenital heart defects per municipality exhibited a range from none to 398 cases. The median number of congenital heart defects per municipality was 1, with a mean of approximately 5.85 and a standard deviation of approximately 21.83. Rates ranged from 0% to 5% of births. The data displayed a right-skewed distribution, indicating that a few municipalities had a disproportionately high number of reported congenital heart defects.
The majority (86%) of CHD cases were vaguely coded in the SINAC database with terms such as “congenital heart defect, not specified,” “other congenital heart defects, not specified,” “possible congenital heart defect,” and “heart defect,” among others. This percentage of unspecified diagnoses makes it challenging to identify and analyze the distribution of specific CHD types across municipalities accurately.
3.1.2 Polluting Industry Distribution
The study examined the distribution of polluting industries across 2446 municipalities. While half of the municipalities had no polluting industries, the average number of industries per municipality was approximately 1.52 (Table 1) However; there was considerable variability, with a standard deviation of 6.29. The data exhibited a right-skewed distribution, indicating that a few municipalities had a disproportionately high number of polluting industries. For the chemical industry, the median number of facilities per municipality was 0, with a mean of approximately 0.31. Similarly, for lead-emitting industries, the median was 0, with a mean of around 0.66. Petrochemical and metallurgic industries exhibited even lower median numbers, both at 0, with mean values of approximately 0.17 and 0.25, respectively. The plastic industry showed a median of 0 and a mean of approximately 0.04. The automotive industry had a median of 0 and a mean of about 0.18. In contrast, heavily contaminated sites exhibited a higher median of 0 and a mean of around 0.44, indicating a more significant presence of such sites compared to other industries.
| Industry | Median | Mean | Std. Dev | 95th percentile |
|---|---|---|---|---|
| All Industries | 0 | 1.52 | 6.29 | 7 |
| Chemicals | 0 | 0.31 | 1.64 | 7 |
| Lead emitting | 0 | 0.66 | 2.51 | 3 |
| Petrochemical | 0 | 0.17 | 1.13 | 1 |
| Plastics | 0 | 0.04 | 0.24 | 0 |
| Metallurgic | 0 | 0.25 | 1.12 | 1 |
| Automotive | 0 | 0.18 | 1.17 | 1 |
| Heavily contaminated Sites | 0 | 0.44 | 3.90 | 2 |
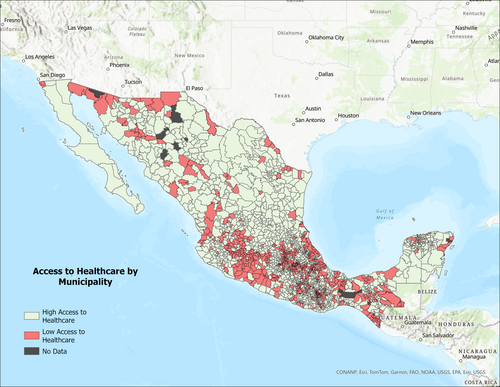
Municipalities with higher percentages of people lacking access to healthcare were more likely to host polluting industries. (Table 2) For example, heavily contaminated sites were present in 18% of municipalities with high healthcare inaccessibility compared to 11% of those with better access. Similarly, 19% of municipalities with high healthcare inaccessibility had two or more polluting industries, whereas only 10% of municipalities with better healthcare access had multiple polluting industries. This pattern was consistent across various types of industries, including lead-emitting, chemical, petrochemical, plastics, automotive, and metallurgic industries. Southern and coastline municipalities showed less access to healthcare than northern municipalities. (Figure 1).
| Municipalities with more access to healthcare (below median) | Municipalities with less access to healthcare (above the median) | |
|---|---|---|
| Heavily contaminated sites | ||
| None |
1090 89% |
1008 82% |
| At least one |
77 6% |
121 10% |
| Two or more |
56 5% |
94 8% |
| Fisher's exact | 0.000 | |
| All polluting industries | ||
| None |
961 78% |
815 67% |
| At least one |
143 12% |
172 14% |
| Two or more |
119 10% |
236 19% |
| Fisher's exact | 0.000 | |
| Lead emitting | ||
| None |
1015 83% |
874 72% |
| At least one |
142 12% |
200 16% |
| Two or more |
66 5% |
149 12% |
| Fisher's exact | 0.000 | |
| Chemicals | ||
| None |
1160 95% |
1068 87% |
| At least one |
40 3% |
58 6% |
| Two or more |
23 2% |
87 7% |
| Fisher's exact | 0.000 | |
| Petrochemicals | ||
| None |
1167 95% |
1101 90% |
| At least one |
42 4% |
82 7% |
| Two or more |
14 1% |
40 3% |
| Fisher's exact | 0.000 | |
| Plastics | ||
| None |
1202 98% |
1174 96% |
| At least one |
21 3% |
49 4% |
| Fisher's exact | 0.001 | |
| Automotive | ||
| None |
1182 97% |
1123 92% |
| At least one |
22 2% |
51 4% |
| Two or more |
19 1% |
49 4% |
| Fisher's exact | 0.000 | |
| Metallurgic | ||
| None |
1117 91% |
1064 87% |
| At least one |
63 5% |
84 7% |
| Two or more |
43 4% |
75 6% |
| Fisher's exact | 0.001 | |
- a Number and percentage of municipalities with different levels of industrial presence, stratified by healthcare accessibility (measured as the percentage of the population without access to healthcare).
Polychoric correlations indicated positive relationships between the presence of polluting industries and the lack of access to healthcare. (Table 3) Correlation coefficients ranged from 0.14 (lead emitting) to 0.31 (chemicals), showing that municipalities with more extensive polluting industries also tend to have higher percentages of individuals without access to healthcare services. All correlations were statistically significant.
| Industry | Correlation coefficients |
|---|---|
| All polluting industries | 0.23 |
| Lead emitting | 0.14 |
| Petrochemicals | 0.25 |
| Automotive | 0.26 |
| Metallurgic | 0.15 |
| Heavily contaminated Sites | 0.18 |
| Chemicals | 0.31 |
| Plastics | 0.22 |
- a Correlation coefficients between industry presence and lack of healthcare access (measured as the percentage of the population without access to healthcare).
Model 1 assessed the relationship between access to healthcare and the incidence of congenital heart defects. (Table 4) The association was not statistically significant (IRR: 1.06; 95% CI: 0.97–1.16; p = 0.196), but the direction of the effect suggested a potential increase in the risk of congenital heart defects in municipalities with poor access to healthcare.
| IRR (95% CI) | p | |
|---|---|---|
| Lack of access to healthcare | 1.06 (0.97–1.16) | 0.196 |
- a Model 1 estimates the association between healthcare inaccessibility and CHD incidence, presenting incidence rate ratios (IRRs) and 95% confidence intervals (CIs).
Model 2 demonstrated significant associations between the presence of polluting industries and an increased incidence of congenital heart defects. (Table 5) The incidence rate ratios (IRRs) for municipalities with at least one heavily contaminated site was 1.21 (95% CI: 1.06–1.37; p = 0.003), and for those with two or more sites, it was 1.23 (95% CI: 1.09–1.38; p = 0.001). Similar associations were observed across various types of polluting industries, with the strongest association in the chemical industry (IRR: 1.40 for two or more sites; 95% CI: 1.24–1.58; p < 0.0001).
| IRR (95% CI) | p | |
|---|---|---|
| Heavily contaminated sites | ||
| None | REF | |
| At least one | 1.21 (1.06–1.37) | 0.003 |
| Two or more | 1.23-(1.09–1.38) | 0.001 |
| All polluting industries | ||
| None | REF | |
| At least one | 1.17 (1.03–1.33) | 0.013 |
| Two or more | 1.31 (1.19–1.44) | p < 0.0001 |
| Lead emitting | ||
| None | REF | |
| At least one | 1.24 (1.12–1.38) | p < 0.0001 |
| Two or more | 1.26 (1.13–1.40) | p < 0.0001 |
| Chemicals | ||
| None | REF | |
| At least one | 1.30 (1.13–1.50) | p < 0.0001 |
| Two or more | 1.40 (1.24–1.58) | p < 0.0001 |
| Petrochemicals | ||
| None | REF | |
| At least one | 1.17 (1.02–1.34) | 0.019 |
| Two or more | 1.24 (1.08–1.42) | 0.002 |
| Plastics | ||
| None | REF | |
| At least one | 1.33 (1.14–1.54) | p < 0.0001 |
| Automotive | ||
| None | REF | |
| At least one | 1.19 (1.02–1.38) | 0.022 |
| Two or more | 1.23 (1.40–1.44) | 0.013 |
| Metallurgic | ||
| None | REF | |
| At least one | 1.23 (1.08–1.41) | 0.002 |
| Two or more | 1.25 (1.10–1.43) | 0.001 |
- a Model 2 estimates the association between polluting industrial activities and CHD incidence, presenting incidence rate ratios (IRRs) and 95% confidence intervals (CIs).
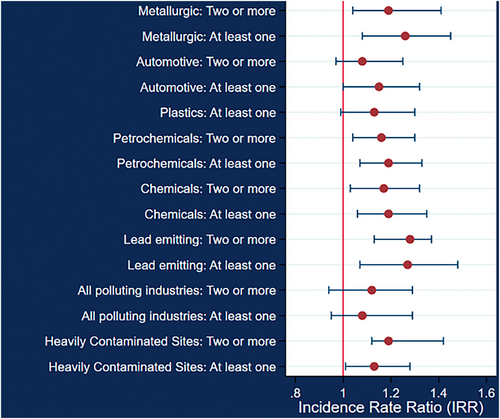
After adjusting for lack of access to healthcare (controlling for prenatal diagnosis bias and early detection differences), the relationship between congenital heart defects and the polluting industry, including heavily contaminated sites, remained robust and statistically significant (Table 6, Figure 2). The highest risk was found within municipalities with a higher presence of the chemical industry, with a 39% increased risk of congenital heart defects, even after accounting for variations in access to healthcare. A similar model controlling for both access to healthcare and access to food was explored, and the direction of the association and the statistical significance remained similar, further reinforcing the robustness of the findings (Table S3).
| IRR (95% CI) | p | |
|---|---|---|
| Heavily contaminated sites | ||
| None | REF | |
| At least one | 1.20 (1.06–1.32) | 0.005 |
| Two or more | 1.22 (1.08–1.38) | 0.001 |
| All polluting industries | ||
| None | REF | |
| At least one | 1.17 (1.03–1.33) | 0.014 |
| Two or more | 1.31 (1.18–1.44) | p < 0.0001 |
| Lead emitting | ||
| None | REF | |
| At least one | 1.24 (1.11–1.38) | p < 0.0001 |
| Two or more | 1.25 (1.12–1.40) | p < 0.0001 |
| Chemicals | ||
| None | REF | |
| At least one | 1.30 (1.13–1.50) | p < 0.0001 |
| Two or more | 1.39 (1.23–1.58) | p < 0.0001 |
| Petrochemicals | ||
| None | REF | |
| At least one | 1.16 (1.01–1.33) | 0.028 |
| Two or more | 1.22 (1.07–1.40) | 0.003 |
| Plastics | ||
| None | REF | |
| At least one | 1.32 (1.13–1.53) | p < 0.0001 |
| Automotive | ||
| None | REF | |
| At least one | 1.18 (1.02–1.37) | 0.03 |
| Two or more | 1.21 (1.03–1.43) | 0.02 |
| Metallurgic | ||
| None | REF | |
| At least one | 1.23 (1.07–1.41) | 0.003 |
| Two or more | 1.24 (1.09–1.42) | 0.001 |
- a Model 3 estimates the association between CHD incidence, healthcare inaccessibility, and polluting industrial activities, presenting incidence rate ratios (IRRs) and 95% confidence intervals (CIs).
Model 4 examined the potential effect modification of the relationship between polluting industries and congenital heart defects by access to healthcare (Table 7). Significant interaction effects were found for several industries. For all polluting industries, municipalities with a higher percentage of individuals lacking access to healthcare exhibited higher IRRs for congenital heart defects. Specifically, the presence of two or more polluting industries resulted in IRRs of 1.42 (95% CI: 1.25–1.60) in municipalities with poor healthcare access, compared to 1.12 (95% CI: 0.94–1.34) in those with better healthcare access (Figure 3).
| IRR (95% CI) | IRR (95% CI) | ||
|---|---|---|---|
| All polluting industries | < Median healthcare inaccessibility (%) | ≥ Median healthcare inaccessibility (%) | Overall and strata-specificb EMM p-valuec |
| None | REF | REF | 0.099b |
| At least one | 1.15 (0.95–1.39) | 1.20 (1.01–1.42) | 0.772c |
| Two or more | 1.12 (0.94–1.34) | 1.42 (1.25–1.60) | 0.034c |
| Lead emitting | |||
| None | REF | REF | 0.025b |
| At least one | 1.26 (1.06–1.50) | 1.24 (1.08–1.42) | 0.889c |
| Two or more | 1.00 (0.81–1.23) | 1.38 (1.21–1.57) | 0.011c |
| Petrochemicals | |||
| None | REF | REF | 0.134b |
| At least one | 0.93 (0.70–1.24) | 1.27 (1.10–1.48) | 0.054c |
| Two or more | 1.12 (0.84–1.50) | 1.27 (1.10–1.48) | 0.463c |
| Automotive | |||
| None | REF | REF | 0.078b |
| At least one | 1.05 (0.77–1.42) | 1.25 (1.05–1.48) | 0.330c |
| Two or more | 0.85 (0.57–1.27) | 1.36 (1.14–1.61) | 0.036c |
| Metallurgic | |||
| None | REF | REF | 0.409b |
| At least one | 1.26 (1.00–1.59) | 1.22 (1.03–1.44) | 0.821c |
| Two or more | 1.08 (0.83–1.41) | 1.33 (1.15–1.55) | 0.200c |
| Chemicals | |||
| None | REF | REF | 0.239b |
| At least one | 1.32 (0.99–1.76) | 1.29 (1.10–1.51) | 0.884c |
| Two or more | 1.08 (0.77–1.52) | 1.47 (1.29–1.68) | 0.096c |
| Plastics | |||
| None | REF | REF | 0.765b |
| At least one | 1.27 (0.90–1.78) | 1.34 (1.14–1.58) | 0.766c |
| Heavily contaminated sites | |||
| None | REF | REF | 0.51b |
| At least one | 1.08 (0.87–1.35) | 1.27 (1.09–1.48) | 0.259c |
| Two or more | 1.18 (0.95–1.47) | 1.25 (1.08–1.44) | 0.689c |
- a Model 4 evaluates the interaction between healthcare inaccessibility and polluting industrial activities on CHD incidence, using a p-value threshold of 0.20 to assess effect modification.
- b Overall and strata-specific.
- c EMM p-value.
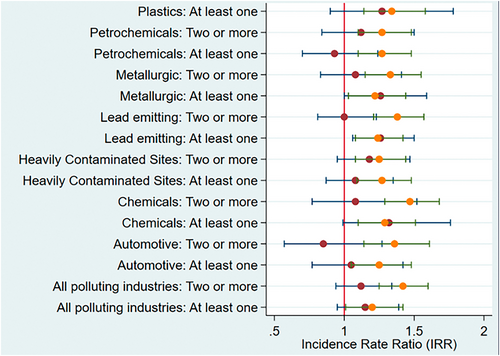
Lead-emitting industries showed significant results. In municipalities with high healthcare inaccessibility, the presence of two or more lead-emitting industries was associated with a higher risk of congenital heart defects (IRR: 1.38; 95% CI: 1.21–1.57) compared to those with better healthcare access (IRR: 1.00; 95% CI: 0.81–1.23). For municipalities that had at least one lead-emitting industry, the IRRs were 1.26 (95% CI: 1.06–1.50) in areas with better healthcare access and 1.24 (95% CI: 1.08–1.42) in areas with poor access.
Petrochemical industries showed mixed results. In municipalities with high healthcare inaccessibility, the presence of at least one petrochemical industry was associated with an IRR of 1.27 (95% CI: 1.10–1.48), compared to an IRR of 0.93 (95% CI: 0.70–1.24) in areas with better access (interaction p-value = 0.054). For municipalities that had two or more petrochemical industries, the IRRs were similar for both high and low healthcare inaccessibility (interaction p-value = 0.463).
In the automotive industry, the highest IRR was associated with areas with two or more industries and less limited access to healthcare. Statistically significant results were also found in both categories with greater proportions of individuals lacking access to healthcare. No significant interaction effects (p > 0.20) were observed for the metallurgic, chemicals, plastics industries, and heavily contaminated sites.
4 Discussion
Our study found that the presence of polluting industries in Mexican municipalities is significantly associated with higher incidence rates of congenital heart defects (CHDs), and this relationship is exacerbated in areas with poor access to healthcare. While the types of polluting industries vary, they consistently exhibit similar health outcomes and disproportionately impact the same vulnerable populations.
Our results highlight significant spatial and sociodemographic disparities in the distribution of polluting industries and their potential health impacts on congenital anomalies.
The analysis revealed that municipalities with higher percentages of individuals lacking access to healthcare were more likely to host polluting industries. Specifically, municipalities with greater healthcare inaccessibility exhibited a higher prevalence of heavily contaminated sites and multiple polluting industries. For instance, 19% of municipalities with high healthcare inaccessibility had two or more polluting industries compared to only 10% of municipalities with better healthcare access. This pattern was consistent across various types of industries, including lead-emitting, chemical, petrochemical, plastics, automotive, and metallurgic industries. Polychoric correlations supported these findings, indicating positive relationships between the presence of polluting industries and the lack of access to healthcare, with correlation coefficients ranging from 0.14 for lead-emitting industries to 0.31 for chemical industries.
Model 1 assessed the relationship between access to healthcare and the incidence of CHDs, showing a non-significant association (IRR: 1.06; 95% CI: 0.97–1.16; p = 0.196). Although not statistically significant, the direction of the effect suggested a potential increase in the risk of CHDs in municipalities with poor access to healthcare. This aligns with previous research indicating that limited access to healthcare services can exacerbate adverse health outcomes, particularly in vulnerable populations (Gulliford et al. 2002).
Model 2 demonstrated significant associations between the presence of polluting industries and increased incidence of CHDs. Municipalities with at least one heavily contaminated site had an IRR of 1.21 (95% CI: 1.06–1.37), and those with two or more sites had an IRR of 1.23 (95% CI: 1.09–1.38). Similar associations were observed across various types of polluting industries, with the strongest association in the chemical industry (IRR: 1.40 for two or more sites; 95% CI: 1.24–1.58). These findings corroborate toxicological evidence linking exposure to industrial pollutants with congenital anomalies (Zhang et al. 2016).
After adjusting for lack of access to healthcare in Model 3, the relationship between CHDs and polluting industries remained robust and statistically significant. For example, the presence of at least one heavily contaminated site was associated with a 20% increase in CHD risk (IRR: 1.20; 95% CI: 1.06–1.32), and the presence of two or more sites was associated with a 22% increase (IRR: 1.22; 95% CI: 1.08–1.38). The highest risk was found within municipalities with a higher presence of the chemical industry, even after controlling for healthcare access, highlighting the persistent risk posed by industrial pollutants (Ren et al. 2011).
Model 4 examined the potential effect modification by access to healthcare on the relationship between polluting industries and CHDs. Significant interaction effects were found for several industries. In municipalities with high healthcare inaccessibility, the presence of two or more lead-emitting industries was associated with a higher risk of CHDs (IRR: 1.38; 95% CI: 1.21–1.57) compared to those with better healthcare access (IRR: 1.38; 95% CI: 1.08–1.77). Similarly, for all polluting industries, municipalities with a higher percentage of individuals lacking access to healthcare exhibited higher IRRs for CHDs. Specifically, the presence of two or more polluting industries resulted in IRRs of 1.42 (95% CI: 1.25–1.60) in municipalities with poor healthcare access compared to 1.26 (95% CI: 1.02–1.57) in those with better healthcare access. These findings suggest that inadequate access to healthcare exacerbates the adverse health impacts of environmental pollution, highlighting the critical role of healthcare infrastructure in mitigating environmental health risks (Brender et al. 2011).
Our study is consistent with existing literature on environmental justice and health disparities, contributing to the understanding of how industrial pollution disproportionately affects vulnerable populations. Previous studies have shown that marginalized communities often face higher exposure to environmental pollutants and have limited access to healthcare, compounding their health risks (Brulle and Pellow 2006; Bullard 2005). Our findings add to this body of evidence by specifically linking industrial pollution to increased CHD incidence and highlighting the exacerbating effect of healthcare inaccessibility, an association that has not been previously demonstrated in Mexico.
Importantly, our study reveals that inadequate healthcare access exacerbates the health risks posed by industrial pollutants, specifically increasing the incidence of congenital heart defects (CHDs). Previous literature shows that limited access to healthcare can delay the diagnosis and treatment of CHDs, leading to increased child mortality (Liu et al. 2019).
However, several limitations should be acknowledged. The study lacks data on the distribution of non-polluting industries, which could provide a more comprehensive view of industrial impacts. Additionally, CHD cases in the SINAC database may not reflect all occurrences, as not all cases are screened or detected at birth (Van Nisselrooij et al. 2020). Many cases likely represent the most severe forms identified in hospitals, or even minor ones found in hospitals that conduct CHD screenings, while others go undetected or occur in settings with less rigorous screening protocols.
A significant limitation of our data is that 86% of CHD cases were coded as “congenital heart defect, not specified” in the SINAC database. This high percentage of unspecified diagnoses likely results from parents or families not knowing the specific type of CHD at the time of registration, or from the final diagnosis not being made when the birth was registered. This limitation hinders our ability to accurately identify and analyze the distribution of specific CHD types across municipalities, which is crucial for targeted interventions and understanding the full scope of environmental impacts on CHD incidence.
Environmental justice concerns arise from our findings, highlighting the need for equitable distribution of environmental risks and healthcare resources. The regulation of heavily contaminated sites in Mexico remains a challenge, with current measures often insufficient to protect public health fully. Awareness of these issues and their public health implications is crucial for driving policy changes and interventions. The public health burden of CHDs, exacerbated by industrial pollutants and poor healthcare access, requires targeted programs for protection and prevention. These findings should prompt more rigorous regulations that protect marginalized communities that have been disproportionately impacted by industrial pollution.
Current programs must be evaluated and expanded to address these disparities effectively. Interventions should focus on reducing industrial emissions, improving regulatory frameworks, and enhancing access to healthcare services. Future research should further explore the mechanisms underlying these associations and evaluate the effectiveness of policy measures aimed at reducing industrial emissions and enhancing healthcare services.
5 Conclusion
Our study highlights the significant association between polluting industries and the incidence of congenital heart defects (CHDs) in Mexican municipalities. Municipalities with higher levels of industrial pollution have increased rates of CHDs. This relationship persists even after adjusting for healthcare access, underscoring the direct impact of industrial emissions on congenital anomalies.
Importantly, inadequate healthcare access exacerbates the health risks posed by industrial pollutants. Municipalities with limited healthcare services show a stronger association between polluting industries and CHDs, highlighting the critical role of healthcare access in mitigating the effects of environmental contaminants.
Addressing environmental justice concerns is paramount. Our results highlight the need for strengthening regulatory frameworks in Mexico to control heavily contaminated sites and reduce the public health impact of industrial activities. Increasing public awareness of these issues is essential for mobilizing policy interventions and public health strategies.
The burden of CHDs requires targeted prevention and protection programs. Enhancing healthcare services and implementing robust environmental regulations are critical steps toward mitigating the health risks posed by industrial pollution. Evaluating and expanding current programs is crucial to addressing these disparities effectively.
Future research should focus on understanding the mechanisms linking industrial pollution to congenital anomalies and assessing the effectiveness of interventions aimed at reducing exposure and improving healthcare access. By addressing these complex interactions, we can work towards a more equitable and healthier environment for all.
Acknowledgments
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available in Subsistema de Información sobre Nacimientos (SINAC) at http://www.dgis.salud.gob.mx/contenidos/sinais/s_sinac.html. These data were derived from the following resources available in the public domain:-Subsistema de Información sobre Nacimientos (SINAC), http://www.dgis.salud.gob.mx/contenidos/sinais/s_sinac.html-Registro de Emisiones y Transferencia de Contaminantes, https://datos.gob.mx/busca/dataset/registro-de-emisiones-y-transferencia-de-contaminantes.




