Childhood Educational Outcomes of Infants Born With Esophageal Atresia With or Without Tracheoesophageal Fistula
Funding: This work was supported by the March of Dimes/Centers for Disease Control and Prevention (CDC) (grant number U38OT000199 [to JR]).
The abstract and the preliminary findings of this article were presented at the Society for Pediatric Research, Washington, DC, May 2023.
[Correction added after first online publication on 24 December 2024. Author wishes to Update the article title.]
ABSTRACT
Background
There are limited studies on educational outcomes of children born with esophageal atresia (EA) with or without tracheoesophageal fistula (TEF). We aimed to compare 3rd to 5th grade academic proficiency among children born with EA/TEF versus unaffected children.
Methods
Children born with EA/TEF (2000–2005) were identified from the Arkansas Reproductive Health Monitoring System. For each child born with EA/TEF, up to two unaffected children were selected from birth certificates and matched on hospital and month of birth, sex, and race and ethnicity. Data on NICU hospitalization were abstracted from medical records at Arkansas' only pediatric specialty hospital. The study outcomes were 3rd to 5th grade proficiency on literacy and mathematic standardized achievement tests, referral to special education, and days of school absence. Regression models were used to assess the association of outcome measures with diagnosis of EA/TEF, after adjusting for differences in covariates between EA/TEF and unaffected children and accounting for paired correlations using the generalized estimating equation method.
Results
The final cohort included 20 surviving children born with EA/TEF and 31 unaffected children. There was no significant difference in literacy (3rd: 70% vs. 71%; 4th: 83% vs. 81%; 5th: 94% vs. 87%, p > 0.05) or mathematics proficiency (3rd: 80% vs. 87%; 4th: 83% vs. 78%; 5th: 75% vs. 78%, p > 0.05), referral to special education (20% vs. 19%, p = 0.65), or total days of school absence (47 vs. 26 days, p = 0.07) between EA/TEF and unaffected children.
Conclusions
Children born with EA/TEF had comparable academic proficiency to unaffected children.
Abbreviations
-
- ACH
-
- Arkansas Children's Hospital
-
- ADE
-
- Arkansas Department of Education
-
- ADH
-
- Arkansas Department of Health
-
- AGA
-
- appropriate for gestational age
-
- AHID
-
- Arkansas Hospital Inpatient Discharge
-
- ARHMS
-
- Arkansas Reproductive Health Monitoring System
-
- EA
-
- esophageal atresia
-
- GEE
-
- generalized estimating equation
-
- ICD-CM
-
- International Classification of Diseases-Clinical Modification
-
- LGA
-
- large for gestational age
-
- max
-
- maximum
-
- min
-
- minimum
-
- NICU
-
- Neonatal Intensive Care Unit
-
- SGA
-
- small for gestational age
-
- TEF
-
- tracheoesophageal fistula
-
- UAMS
-
- University of Arkansas for Medical Sciences
1 Introduction
Esophageal atresia (EA) with or without tracheoesophageal fistula (TEF) is a congenital foregut anomaly that occurs in 1:2500–4500 live births (Mai et al. 2019) and requires early neonatal surgery (van der Zee, Tytgat, and van Herwaarden 2017). Although EA/TEF can occur as an isolated finding, up to 60% of these patients have additional congenital defects and/or chromosomal abnormalities (Sfeir et al. 2013). With the recent advances in neonatal and surgical care, the current survival of these infants exceeds 90%, with mortality mostly attributed to associated congenital anomalies (Sfeir et al. 2013; Wang et al. 2014). Although most prior studies on outcomes of children born with EA/TEF have focused on their long-term physical and medical morbidities (Peters et al. 2017; Sfeir et al. 2021), a small but growing literature has recently shifted to evaluating their neurodevelopment outcomes (Burnett et al. 2021; Harmsen et al. 2017; Mawlana et al. 2018).
Children born with EA/TEF have ongoing gastrointestinal and respiratory morbidities that may affect their neurodevelopment (Malmström et al. 2008; Pedersen et al. 2013). Previous reports have assessed their referral rate to special education services (Bouman, Koot, and Hazebroek 1999; Faugli et al. 2009; Hamrick et al. 2010; Lacher et al. 2010) or evaluated their physical, intellectual, and psychosocial functioning up to 17 years of life. While some reported reassuring motor performance and normal intelligence or psychosocial functioning in comparison to population norms (Aite et al. 2014; Gischler et al. 2009) or healthy controls (Lindahl 1984; Walker et al. 2016), others found weakened motor performance and reduced attention (Harmsen et al. 2017) or impaired intelligence (Bouman, Koot, and Hazebroek 1999; Kubota et al. 2011). Thus, there are currently contradictory reported findings regarding the neurodevelopment of these infants and insufficient evidence concerning their academic performance at school age.
Our objectives were to examine 3rd through 5th grade educational outcomes of children born with EA/TEF and unaffected matched children and compare their rates of referral to special education services and total days of school absence during 3rd through 5th grade. Our a priori hypothesis was that children born with EA/TEF, with no associated chromosomal abnormalities, had similar academic performance to unaffected children.
2 Methods
This retrospective cohort study was approved by the Arkansas Department of Health (ADH) Scientific Advisory Committee and the University of Arkansas for Medical Sciences (UAMS) Institutional Review Board (# 207318).
2.1 Databases and Linkage
Children born with EA/TEF, from January 1, 2000 to December 31, 2005, were identified from the Arkansas Reproductive Health Monitoring System (ARHMS), a statewide, population-based birth defects surveillance program whose trained health information systems' staff abstract clinical, demographic, and socioeconomic data from medical records at all delivering hospitals in Arkansas, the state's only pediatric specialty-care hospital and associated clinics, and the high-risk pregnancy and prenatal diagnosis centers. ARHMS staff code birth defects based on the six-digit British Pediatric Association extension of the International Classification of Diseases, Ninth Edition Clinical Modification (ICD-9-CM) coding system, as modified by the Division of Birth Defects and Developmental Disabilities of the Centers for Disease Control and Prevention and ARHMS. Eligibility for ARHMS requires Arkansas residency of the mother at the time of delivery and diagnosis of a structural congenital malformation during pregnancy, after stillbirth or termination of pregnancy, after live birth, and up to 2 years of age.
Using key identifiers such as mother's and child's first and last names, ARHMS data were linked to the ADH vital health statistics that track data on all births and deaths in Arkansas. For each child born with EA/TEF, up to two unaffected children (i.e., children who did not have a structural birth defect) were randomly selected from birth certificates and matched on hospital and month of birth, sex, and maternal race and ethnicity. The resultant file was linked to death records using birth certificate number. Demographic and socioeconomic characteristics including maternal education and limited clinical variables and paternal age, race, and ethnicity were obtained from birth certificate data on surviving EA/TEF children and unaffected matched children. We defined size for gestational age based on the U.S. sex-specific national standard growth curve. As such, small (SGA) and large for gestational age (LGA) infants had a birth weight < 10th or > 90th percentile, respectively (Olsen et al. 2010), while appropriate for gestational age (AGA) had a birth weight at or between the 10th and 90th percentile.
Using the birth certificate number, the ADH linked ARHMS surviving children with EA/TEF to the Arkansas Hospital Inpatient Discharge (AHID) database. AHID database claims track discharges from hospitals in Arkansas that had a hospital length of stay of ≥ 1 day and include their dates of service, length of stay, procedures, discharge diagnoses, and discharge status. We determined the number of rehospitalization and length of stay of hospital readmissions for surviving children with EA/TEF within 5 years of discharge from the neonatal intensive care unit (NICU) hospitalization where the initial surgery for EA/TEF repair was completed. The AHID database also documents payer status. Maternal education collected from the ADH vital health records and child's payer status abstracted from the AHID database were considered proxy measures of socioeconomic status.
Arkansas Children's Hospital (ACH) is the only pediatric specialty hospital in the state where > 90% of infants born with EA/TEF in Arkansas are transferred shortly after birth. If the medical record number was not available, the child's name and date of birth as well as mother's name were used to link children born with EA/TEF to their medical records at ACH. Data collected from ACH medical records included clinical and surgical characteristics of the first NICU admission of these children as well as length of stay and discharge diagnoses of any EA/TEF-related readmission within five years of NICU discharge.
The file including data from surviving children born with EA/TEF and surviving unaffected matched children was securely transmitted to the Arkansas Department of Education (ADE). The ADE database includes scores and proficiency designations from the Arkansas public school students who took the Augmented Benchmark Examination tests in literacy and mathematics (grades 3–8) that are administered annually. Scores designated as proficient or advanced (“proficient”) represented performance at or above grade level, while scores designated “non-proficient” represented performance below grade level (ElHassan et al. 2022; Walden et al. 2023). The threshold of proficiency is set by the ADE and is determined by the percentage of correct answers on the exams. The ADE database also documents the total days of school absence per child at 3rd through 8th grade and whether the child was referred to special education at any of these grades. The two groups of children were linked to their annual ADE records using their social security numbers. Students who were home schooled, attended private schools, or moved out of Arkansas, did not take the benchmark examination, could not be linked to their achievement test records, and were excluded. This final file was de-identified and securely transmitted to the UAMS researchers for analysis. The primary outcome measure was dichotomous variable of proficiency for each of the literacy and mathematics achievement tests at 3rd to 5th grade. The secondary outcomes measures were dichotomous variable of referral to special education at 3rd, 4th, or 5th grade and total days of school absence at 3rd through 5th grade.
2.2 Statistical Analysis
Continuous variables were summarized as median (minimum (min), maximum (max)); categorical variables were summarized as numbers and frequency (%). Mann–Whitney U test and Fisher's exact tests were used to compare statistics of numerical and categorical variables between EA/TEF children with links to education data versus those without links to education data. We compared characteristics of children born with EA/TEF and matched unaffected children using mixed-effect models for continuous variables and mixed-effect logistic and cumulative regression models for binary and categorical variables, respectively. A random effect was included in these models to account for correlations between matched pairs. In cases where small (≤ 3) number of children was observed for a binary variable among a comparison group, a Fisher's exact test was used. Characteristics with a p value < 0.2 were selected as covariates for the multivariate statistical models. At each grade, a multivariate logistic regression model was used to assess the association of a binary outcome of proficiency in literacy (or mathematics) with a diagnosis of EA/TEF (EA/TEF vs. unaffected), after adjusting for covariates and accounting for paired correlation using the generalized estimating equation (GEE) method. The same logistic regression model was also applied to the binary outcome of referral to special education. For the numerical outcome of total days of school absence, a Poisson regression model was used to assess its association with EA/TEF diagnosis after adjusting for the same covariates and accounting for the paired effect using GEE method. Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
3 Results
3.1 Study Cohort
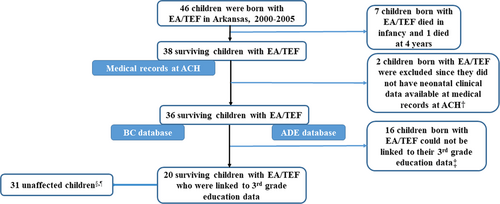
A total of 46 infants were born, 2000–2005, with EA/TEF in Arkansas. Eight children with associated cardiovascular malformations, chromosomal abnormalities, or extreme prematurity did not survive to school age. Two children were excluded since they were possibly transferred out of state after birth and were not admitted to the NICU at ACH. Sixteen children were homeschooled, adopted, attended private school, or moved out of state and could not be linked to their 3rd grade education data. The final cohort included a total of 20 children with EA/TEF and 31 matched children without a structural birth defect (Figure 1).
3.2 Study Cohort Characteristics
There was no significant difference in parental or neonatal characteristics between those children who were linked versus not linked to their education data (Table S1). Most mothers of children born with EA/TEF were Caucasian (75%), received prenatal care (94%), and completed at least a high school education (81%). Infants had a median gestational age of 38 weeks (min = 30; max = 42) at birth and were typically singleton (83%) and AGA (75%). The majority of these infants had EA with distal TEF (83%) and more than half (56%) had associated congenital anomalies (12 infants had non-cyanotic heart disease including ventricular or atrial septal defect; 7 infants had a gastrointestinal anomaly including imperforate anus or duodenal atresia; 8 infants had a renal anomaly including absent kidney, horseshoe kidney, multi-dysplastic kidney, hydronephrosis, or ureteropelvic obstruction; 10 infants had a musculoskeletal anomaly including tethered cord, absent radii, rib anomaly; and 10 of these patients had at least anomalies in 2 systems). Eighty-nine percent had undergone an open surgical repair with almost half (47%) developing a stricture and 11% developing anastomosis leak, afterwards. These children received a median dose of 0.65 mg/kg of morphine and 0.3 mg/kg of lorazepam for pain and sedation control during their NICU hospitalization. The median length of their NICU stay was 20 days with almost half (46%) requiring EA/TEF related readmissions within the first 5 years of discharge from NICU hospitalization where the initial surgery for EA/TEF repair was completed.
The demographic, socioeconomic, and clinical characteristics of the matched unaffected children were obtained from the birth certificates and AHID database (Table 1). Among children who could be linked to their education data, unaffected children had a higher median birth weight (3260 (min = 879; max = 4649) grams) in comparison to children born with EA/TEF (median birth weight = 2864 (min = 1049; max = 4621) grams) (p = 0.02) though comparable gestational age and size for gestation.
| Characteristics | Children born with EA/TEF N = 20 | Unaffected matched children N = 31 | p-value |
|---|---|---|---|
| Maternal characteristics | |||
| Age (years), median (min, max) | 24 (18, 38) | 23 (16, 38) | 0.33 |
| Parity, n (%) | 0.11 | ||
| 0, 1 | 17 (85%) | 20 (65%) | |
| ≥ 2 | 3 (15%) | 11 (35%) | |
| Caucasian race, n (%) | 14 (70%) | 22 (71%) | 0.93 |
| Prenatal care (yes), n (%) | 19 (100%)c | 30 (97%) | 1.00d |
| Smoking (yes), n (%) | 3 (15%) | 4 (13%) | 1.00d |
| Less than high school education (yes), n (%) | 4 (20%) | 9 (29%) | 0.48 |
| Paternal characteristics | |||
| Age (years), median (min, max) | 27 (19, 59) | 29 (18, 59) | 0.47 |
| Caucasian race, n (%) | 14 (70%) | 20 (65%) | 0.91 |
| Neonatal characteristics | |||
| Male sex, n (%) | 8 (40%) | 14 (45%) | 0.92 |
| Birth weight (g), median (min, max) | 2864 (1049, 4621) | 3260 (879, 4649) | 0.02 |
| Gestational age (weeks), median (min, max) | 38 (30, 42) | 39 (27, 41) | 0.21 |
| Size for gestation, n (%) | 0.53 | ||
| SGA | 3 (15%) | 5 (16%) | |
| AGA | 16 (80%) | 22 (71%) | |
| LGA | 1 (5%) | 4 (13%) | |
| Singleton, n (%) | 17 (85%) | 30 (97%) | 0.17 |
| Apgar score at 5 minutes < 7 (yes), n (%) | 2 (11%)c | 1 (3%) | 0.73d |
| Delivery by cesarean section (yes), n (%) | 7 (35%)c | 9 (29%) | 0.73 |
| Payer status, n (%) | |||
| Medicaid | 6 (30%) | 16 (52%) | 0.46 |
| Private | 14 (70%) | 10 (32%) | |
| Missing | 0 (0.0%) | 5 (16%) | |
- Abbreviations: AGA, appropriate for gestational age; EA, esophageal atresia; LGA, large for gestational age; max, maximum; min, minimum; SGA, small for gestational age; TEF, tracheoesophageal fistula.
- a Children born with EA/TEF who were transferred to Arkansas Children's Hospital following birth.
- b Children born with EA/TEF and unaffected children who survived till 3rd grade and were successfully linked to their 3rd grade school standardized achievement tests.
- c Data was missing on one patient.
- d Fisher exact test was used.
3.3 Educational and School Outcomes
The number of children with EA/TEF and unaffected children who were linked to their education data decreased as they advanced from 3rd to 5th grade (Table 2). The ages of the children born with EA/TEF and unaffected matched children were comparable and were estimated at 9, 10, and 11 years-old at 3rd, 4th, 5th grade achievement-tests examination. No significant differences were observed in literacy (3rd: 70% vs. 71%; 4th: 83% vs. 81%; 5th: 94% vs. 87%, p > 0.05) or mathematics proficiency (3rd: 80% vs. 87%; 4th: 83% vs. 78%; 5th: 75% vs. 78%, p > 0.05), rate of referral to special education (20% vs. 19%, p = 0.65), or total (3rd through 5th grade) days of school absence (47 (min = 8; max = 488) vs. 26 (min = 1; max = 241) days, p = 0.07) between EA/TEF and unaffected children, while accounting for matching and after adjusting for differences in characteristics between the two groups (Table 2).
| Grade level | Children born with EA/TEF, N, n (%) | Unaffected matched children, N, n (%) | Adjusted odds ratio (95% confidence interval) | p-value |
|---|---|---|---|---|
| Proficiency on literacy achievement-tests | ||||
| Grade 3 |
N = 20 14 (70%) |
N = 31 22 (71%) |
0.68 (0.22, 2.11) | 0.51 |
| Grade 4 |
N = 18 15 (83%) |
N = 27 22 (81%) |
0.95 (0.17, 5.20) | 0.95 |
| Grade 5 |
N = 16 15 (94%) |
N = 23 20 (87%) |
1.35 (0.34, 5.43) | 0.67 |
| Proficiency on mathematic achievement-tests | ||||
| Grade 3 |
N = 20 16 (80%) |
N = 31 27 (87%) |
0.49 (0.09, 2.75) | 0.42 |
| Grade 4 |
N = 18 15 (83%) |
N = 27 21 (78%) |
1.26 (0.22, 7.07) | 0.79 |
| Grade 5 |
N = 16 12 (75%) |
N = 23 18 (78%) |
0.30 (0.08, 1.18) | 0.08 |
| Referral to special education | ||||
| At 3rd, 4th, or 5th grade, N, n (%) |
N = 20 4 (20%) |
N = 31 6 (19%) |
1.52 (0.25, 9.06) | 0.65 |
- Abbreviations: EA, esophageal atresia; TEF, tracheoesophageal fistula.
- a Children born with EA/TEF who were transferred to Arkansas Children's Hospital following birth.
- b Both children born with EA/TEF and unaffected children have survived till 3rd grade and were successfully linked to their 3rd grade school standardized achievement tests.
- c Ages of children born with EA/TEF and unaffected children were comparable at time of test examination and were estimated at 9, 10, and 11 years old at 3rd, 4th, and 5th grade, respectively.
4 Discussion
We leveraged the linkage established between four state databases to compare 3rd through 5th grade educational outcomes of surviving children born with EA/TEF to unaffected children. We noted that children born with EA/TEF with no associated chromosomal abnormalities or cyanotic heart disease and unaffected matched children have comparable 3rd through 5th grade literacy and mathematics proficiency on standardized achievement tests, rate of referral to special education services, and total days of school absence.
The characteristics of the EA/TEF group in our study cohort were comparable to previously reported findings in the literature. The majority (> 80%) of surviving children had EA with distal TEF (Shaw-Smith 2006), were more commonly born at term gestation to Caucasian mothers (Hamrick et al. 2010; Mawlana et al. 2018), had surgery performed within 2 to 3 days of life (Sfeir et al. 2021), and spent a median duration of 2 days on mechanical ventilation and 20 days during their NICU hospitalization (Sfeir et al. 2021). Consistent with our findings, roughly half of infants with EA/TEF have another congenital defect (Geneviève et al. 2007). However, infants in our surviving study cohort did not have cyanotic heart disease, which was previously shown to be associated with poor educational outcomes (Mulkey et al. 2014).
The quality of surgical and neonatal care has significantly improved over the last two decades. Many of the studies that evaluated the psychosocial or neurodevelopmental outcomes of children born with EA/TEF were not contemporaneous (Bouman, Koot, and Hazebroek 1999; Chetcuti and Phelan 1993; Lindahl 1984; Ure et al. 1995; Ure et al. 1998). Thus, their results were not comparable to our present study. Yet, most recent studies either assessed the neurodevelopment of these children via aptitude tests such as the Bayley Scale of Infant Development (Mawlana et al. 2018) or parental questionnaires (Burnett et al. 2021), reported their intelligence quotient and sustained attention (Faugli et al. 2009; Harmsen et al. 2017), evaluated their rate of referral to early intervention (Newton et al. 2016) or need of special education services at school age (Dellenmark-Blom et al. 2023; Hamrick et al. 2010; Kubota et al. 2011), or described their quality of life (Dingemann et al. 2014; Koivusalo et al. 2005; Tan Tanny et al. 2019). The results of the studies on neurodevelopmental outcome and intelligence assessment were conflicting. The definitions of the education school support and the measures of quality of life varied among studies. One study evaluated school absenteeism and found that children who were born with long-gap EA (where the gap was too large for a primary anastomosis during the initial surgery) and are at higher risk of medical complications had similar rates of school absence as children with EA/TEF who underwent primary anastomosis. Although the study determined that nearly one-third of these children missed school at least once per month in the past year, it did not assess their academic performance (Dellenmark-Blom et al. 2023). Some authors have questioned whether the consequences of the possible additional anomalies, primarily associated with major cardiovascular malformations, are sometimes more problematic than those directly related to EA/TEF (Bouman, Koot, and Hazebroek 1999). Thus, there remains a paucity of literature regarding the academic performance of children born with EA/TEF at school. Our study cohort included patients with cardiac septal defects rather than cyanotic heart disease who performed comparable to unaffected children on literacy and mathematics achievement tests and had a similar rate of referral to special education services and total days of school absence to unaffected children.
Our study had multiple strengths including the linkage of multiple databases to evaluate educational outcomes rather than assessing early neurodevelopment using aptitude tests, the comparison of academic performance of children born with EA/TEF to unaffected matched children rather than normative data, and the inclusion of detailed clinical characteristics and socioeconomic measures. However, limitations remain. We acknowledge that our study sample size was small, and we had additional loss to follow-up as patients advanced through grade level, though our number of patients was comparable to prior publications (Faugli et al. 2009). While we included the number and duration of rehospitalizations within the first five years of NICU discharge, we were unable to account for other potential childhood health issues or quality of life in these patients. However, EA/TEF is a rare congenital anomaly and despite our small sample size and the absence of detailed information on childhood health status or quality of life, our study offers valuable insights by assessing the academic performance of children with EA/TEF in late childhood across multiple grade levels.
In conclusion, children born with EA/TEF with no associated congenital cyanotic heart anomalies or chromosomal abnormalities had comparable academic performance to unaffected children. A multicenter collaboration will be needed to recruit a larger sample size and better understand the educational outcomes of these children. Despite our findings of comparable childhood academic performance to unaffected children, we agree with other authors (Burnett et al. 2021; Harmsen et al. 2017; Mawlana et al. 2018) on the importance of scheduled, multidisciplinary follow-up of children born with EA/TEF early in life in order to facilitate early identification and intervention for any possible neurodevelopmental delay and promote good educational outcomes among these children.
Acknowledgments
The authors thank James Robbins, PhD, Professor Emeritus, for his work as Principal Investigator of the original grant which established data linkages between health and education outcomes used in this study.
Disclosure
The authors have no financial relationships relevant to this article to disclose.
Ethics Statement
This study received approval and exempt of patient consent from the University of Arkansas for Medical Sciences Institutional Review Board. The Arkansas Department of Health Scientific Advisory Committee also approved the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All relevant data are within the paper and its supporting files.