Epidemiology of sepsis in a Japanese administrative database
Abstract
Sepsis is the leading cause of death worldwide. Considering regional variations in the characteristics of patients with sepsis, a better understanding of the epidemiology in Japan will lead to further development of strategies for the prevention and treatment of sepsis. To investigate the epidemiology of sepsis, we conducted a systematic literature review of PubMed between 2003 and January 2023. Among the 78 studies using a Japanese administrative database, we included 20 that defined patients with sepsis as those with an infection and organ dysfunction. The mortality rate in patients with sepsis has decreased since 2010, reaching 18% in 2017. However, the proportion of inpatients with sepsis is increasing. A study comparing short-course (≤7 days) and long-course (≥8 days) antibiotic administration showed lower 28-day mortality in the short-course group. Six studies on the treatment of patients with septic shock reported that low-dose corticosteroids or polymyxin B hemoperfusion reduced mortality, whereas intravenous immunoglobulins had no such effect. Four studies investigating the effects of treatment in patients with sepsis-associated disseminated intravascular coagulation demonstrated that antithrombin may reduce mortality, whereas recombinant human soluble thrombomodulin does not. A descriptive study of medical costs for patients with sepsis showed that the effective cost per survivor decreased over an 8-year period from 2010 to 2017. Sepsis has a significant impact on public health, and is attracting attention as an ongoing issue. Further research to determine more appropriate prevention methods and treatment for sepsis should be a matter of priority.
BACKGROUND
Sepsis is the leading cause of death worldwide, with mortality rates ranging from 15% to 30%.1 In 2017, there were an estimated 48.9 million cases of sepsis worldwide, of which 11 million patients died.2 In addition, the medical costs of sepsis in the United States in 2013 exceeded US $20.0 billion, demonstrating a greater social impact than other diseases.3 As such, the World Health Organization called for global action with regard to sepsis in 2017. Following the implementation of the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) in 2016, multiple studies have demonstrated the characteristics and clinical outcomes of sepsis under the new definition.4-6 Population-based research is expected to enhance public awareness of sepsis and facilitate a comprehensive understanding of the current situation. Nevertheless, such research conducted on a population basis remains scarce in Japan, emphasizing the need for comprehensive studies using administrative databases.7
Epidemiological studies on sepsis conducted in North America and Europe between 1979 and 2014 found that mortality decreased; however, the proportion of inpatients with sepsis and the number of sepsis-related deaths were on the rise.6, 8-11 By contrast, a recent Global Burden of Diseases study between 1990 and 2017 reported a decreased proportion of sepsis among all inpatients and a decreased number of sepsis-related deaths.2 This inconsistency may indicate a recent shift in the trends of patients with sepsis or regional variations. Therefore, it is important to understand the characteristics, clinical management, and outcomes of patients diagnosed with Sepsis-3 in Japan.
A comprehensive reimbursement system for medical costs, named the Diagnosis Procedure Combination (DPC) system, was launched in 2003. The claims-based database has population-based statistics on diagnosis, treatment, and medical costs during hospital stays, covering more than 80% of all acute care hospitals in 2019.12 Using this database, several epidemiological studies have revealed an increasing number of patients with sepsis and an escalating cost of sepsis-related medical care in Japan's super-aging society13, 14; however, there is a lack of literature review to obtain a comprehensive understanding of population-based studies in Japan. In this review, we describe the epidemiology, clinical management, and medical costs of patients with sepsis who had an infection and organ dysfunction, which is linked with Sepsis-3 using a Japanese administrative database.
METHODS
Search strategy and procedures
We conducted a systematic literature search of the PubMed database for articles published between 2003 and January 2023. The search query we used was as follows: “Sepsis” OR “Septic shock” OR “Systemic inflammatory response syndrome” OR “Multiple Organ Failure” OR “Multiple Organ dysfunction” AND (“DPC” OR “claims database” OR “national database” OR “administrative database”) AND Japan, Publication Type as (NOT review [Publication Type]) and publication language as (English [Language]).
Three investigators (T. I., T. O., and N. T.) independently identified potentially eligible studies based on titles and abstracts, retrieved the full-text copy of each potentially eligible study, and conducted a full-text review. We excluded studies that did not investigate sepsis characterized by both infection and organ dysfunction, which aligns with the Sepsis-3 definition. Review articles were excluded.
RESULTS
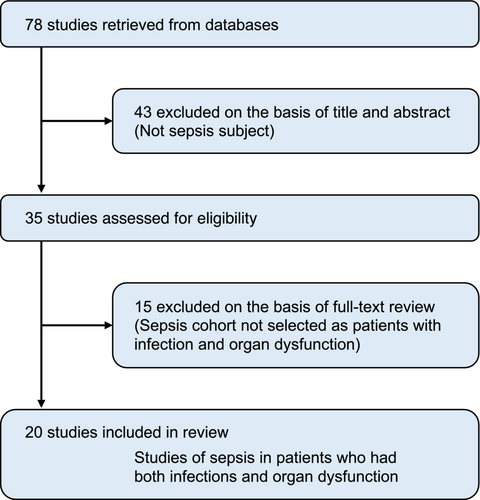
An initial literature search of observational studies using a Japanese administrative database identified 78 articles. Of these, 43 were excluded after a review of titles and abstracts. We performed a full-text review of 35 articles and excluded 15 owing to inconsistencies in the current definition of sepsis. The remaining 20 studies included patients with sepsis with both infection and organ dysfunction (Figure 1). Of the 20 studies investigating patients with sepsis, 6 examined patients with sepsis as a whole, regardless of the site of infection and organ dysfunction.13-18 The remaining 14 studies included only sepsis with pneumonia, perforation of the lower gastrointestinal tract, or shock.12, 19-31 Four studies on patients with sepsis overall were based on the same cohort13-16 (Table 1).
| Study information | Eligible patients, n | Objective | Results |
|---|---|---|---|
| T. Tagami et al. (2014)19 | 9075 | To examine the efficacy of antithrombin in patients with sepsis-associated DIC following severe pneumonia | Antithrombin administration may be associated with reduced 28-day mortality |
| T. Tagami et al. (2015)21 | 6342 | To examine the efficacy of rhTM in patients with sepsis-associated DIC following severe pneumonia | There may be little association between the rhTM administration and mortality |
| T. Tagami et al. (2015)22 | 4919 | To examine whether IVIG administration to mechanically ventilated patients with septic shock due to lower intestinal perforation reduces 28-day mortality | There may be no significant association between IVIG use and mortality in patients with septic shock on mechanical ventilation after emergency laparotomy |
| T. Tagami et al. (2015)23 | 8264 | To examine the effectiveness of IVIG for treating mechanically ventilated patients with pneumonia with septic shock | There may be no significant association between IVIG use and mortality in patients with septic shock on mechanical ventilation for pneumonia |
| T. Tagami et al. (2015)24 | 2202 | To evaluate the efficacy of rhTM in patients with septic shock who develop sepsis-associated DIC after laparotomy for lower intestinal perforation | No association was found between rhTM administration and 28-day mortality in mechanically ventilated patients with septic shock and DIC following intestinal perforation |
| T. Tagami et al. (2015)25 | 2164 | To examine the efficacy of low-dose corticosteroid as an adjunctive therapy for abdominal septic shock | In patients with refractory septic shock after emergency laparotomy for lower intestinal perforation, low-dose corticosteroid administration may be associated with reduced in-hospital mortality |
| T. Tagami et al. (2015)27 | 6925 | To determine whether the use of low-dose corticosteroid reduces mortality in patients with CAP requiring mechanical ventilation | The use of low-dose corticosteroids may improve 28-day mortality in mechanically ventilated patients with CAP and shock, but not in those without shock |
| T. Tagami et al. (2015)30 | 2164 | To examine the effectiveness of antithrombin in mechanically ventilated patients with septic shock and DIC after emergency surgery for lower intestinal perforation | Antithrombin administration may be associated with lower 28-day mortality |
| M. Iwagami et al. (2016)31 | 3759 | To examine the efficacy of PMX in patients with septic shock requiring CRRT | PMX may be effective in patients with septic shock who require CRRT |
| J. Suzuki et al. (2020)26 | 3106 | To compare H2RA and PPI with regard to gastrointestinal bleeding, 28-day mortality, CDI, and nosocomial pneumonia in patients with septic shock following lower gastrointestinal tract perforation | H2RA was not associated with CDI, gastrointestinal bleeding requiring endoscopic hemostasis, 28-day mortality, or nosocomial pneumonia compared with PPI |
| T. Imaeda et al. (2021)13 | 2,043,073 | Epidemiological study on the incidence and mortality of sepsis in Japan | In the 8 years since 2010, in-hospital mortality and length of stay in patients with sepsis have improved significantly, but the incidence and death in patients with sepsis have increased annually |
| K. Fujimori et al. (2021)17 | 44,177 | To examine the association between SOFA score at the onset of sepsis and the effectiveness of PMX | PMX may be effective in patients with sepsis who have SOFA scores of 7–12 |
| K. Fujimori et al. (2021)20 | 30,731 | To examine the efficacy of PMX when used in conjunction with current standard management for patients with septic shock | PMX may be useful in reducing mortality in patients with septic shock who require noradrenaline |
| D. Okuno et al. (2021)12 | 3519 | To examine the use and effectiveness of corticosteroid therapy within 7 days from admission for patients with influenza pneumonia with respiratory failure | The use of systematic corticosteroid therapy in patients with influenza pneumonia was associated with increased in-hospital mortality |
| S. Aso et al. (2021)29 | 50,671 | To investigate the association between dexmedetomidine and mortality in patients with sepsis requiring mechanical ventilation | Dexmedetomidine was associated with lower all-cause 28-day mortality and shorter duration of mechanical ventilation |
| T. Oami et al. (2022)14 | 1,276,678 | To investigate the current trend in economic outcomes of patients with sepsis | Between 2010 and 2017, annual cost-effectiveness for patients with sepsis improved despite increasing medical costs |
| N. Takahashi et al. (2022)15 | 448,146 | To examine whether a shorter course of antibiotics for patients with bacterial sepsis do not significantly increase 28-day mortality compared with a longer course of antibiotics | The short-course group had significantly lower 28-day mortality in patients with sepsis, with a higher rate of reinitiated antibiotics |
| K. Endo et al. (2022)28 | 10,818 | To compare mortality and resource use between ICU and HDU in patients with septic shock | The 30-day mortality was lower in patients with septic shock admitted to the ICU than in those admitted to the HDU |
| T. Oami et al. (2023)16 | 1,167,901 | To test whether ICU admission would improve the survival rate in patients with sepsis | ICU admission may be associated with lower in-hospital mortality in patients with sepsis |
| K. Endo et al. (2023)18 | 49,156 | To test whether the COVID-19 pandemic decreased the incidence of HO-CDI | No significant change in the incidence of HO-CDI was observed in patients with sepsis admitted to a general ward before and after the first emergency declaration in Japan |
- Abbreviations: CAP, community-acquired pneumonia; CDI, Clostridioides difficile infection; COVID-19, coronavirus disease 2019; CRRT, continuous renal replacement therapy; DIC, disseminated intravascular coagulation; H2RA, histamine-2 receptor antagonists; HDU, high-dependency care unit; HO-CDI, health care facility–onset Clostridioides difficile infection; ICU, intensive care unit; IVIG, intravenous immunoglobulin; PMX, polymyxin B hemoperfusion; PPI, proton pump inhibitor; rhTM, recombinant human soluble thrombomodulin; SOFA, Sequential Organ Failure Assessment.
In the clinical management of patients with sepsis, only 1 study discussed antimicrobial therapy.15 Four studies evaluated the efficacy of antithrombin (AT) and recombinant human soluble thrombomodulin (rhTM) in patients with sepsis-associated disseminated intravascular coagulation (DIC).19, 21, 24, 30 Six studies evaluated the effect of intravenous immunoglobulin (IVIG), low-dose corticosteroid treatment, and direct hemoperfusion using polymyxin B–immobilized fiber column direct hemoperfusion (PMX-DHP) on patients with septic shock.17, 20, 22, 23, 25, 27, 31 One study evaluated the effect of ulcer prophylaxis in patients with sepsis after perforation of the lower gastrointestinal tract, and one study investigated the effect of dexmedetomidine in patients with sepsis requiring mechanical ventilation, respectively.26, 29 Only one study discussed medical costs for patients with sepsis.14
Epidemiology
Trends in patients with sepsis across inpatients in Japan
In a study of approximately 50 million adult inpatients during an 8-year period from 2010 to 2017, 2 million patients (4% of total inpatients) had sepsis and 360,000 died from it (Table 2). The median age of patients with sepsis was 76 years, with males accounting for 60% of the patients. Major comorbidities were malignancy (35%), hypertension (26%), and diabetes (22%), with the number of patients with hypertension and diabetes increasing significantly annually. Respiratory tract was the most common site of infection (41%). The median length of hospital stay was 29 days, and in-hospital mortality rate was 20%.13
| Proportion | 4.9% of the total inpatients in 2017, the annual proportion has increased during 2010–201713 |
| Age, year | 76 (66–84) in 2010–2017,13 82 (74–88) in 2018–202118 |
| Female | 41.4% in 2010–2017,13 44.9% in 2018–202118 |
| Comorbidity | 1. Malignant tumor 34.9%, 2. Hypertension 26.3%, 3. Diabetes mellitus 21.8%13 |
| Infectious site | 1. Respiratory 41.0%, 2. Urogenital 15.3%, 3. Abdominal 11.6% in 2010–201713 |
| 1. Respiratory 65.4%, 2. Urogenital 27.4%, 3. Abdominal 7.8% in 2018–202118 | |
| Organ dysfunction | 1. Respiratory 72.7%, 2. Renal 39.1%–44.7%, 3. Coagulation 10.8%–12.4%, 4. Cardiovascular 7.4%, 5. Liver 3.8%–4.0%13, 15, 16 |
| Organ support | 1. Mechanical ventilation 17.7%–18.7%, 2. Vasopressor 12.4%–12.8%, 3. Renal replacement therapy 6.7%–7.0% in 2010–201713, 15, 16 |
| 1. Mechanical ventilation 15.6%, 2. Renal replacement therapy 12.2% in 2018–202017 | |
| ICU admission | 17.1% in 2010–201713 |
| Mortality | 28-day mortality rate: 22.7% in 2018–202017 |
| In-hospital mortality rate: 18.7% in 2017, the annual in-hospital mortality rate has improved during 2010–201713; 22.0% in 2018–202118 | |
|
ICU vs. non-ICU 30-day mortality rate: ICU 25.8% vs. non-ICU 29.2% (overall patients with sepsis in 2010–2017)16; ICU 31.0% vs. HDU 29.9% (patients with septic shock in 2010–2021)28 |
- Note: Data on age are expressed as median (interquartile range).
- Abbreviations: ICU, intensive care unit; HDU, high-dependency unit.
This trend has remained consistent since 2018. In a study of approximately 50,000 adult inpatients with sepsis in general wards from 2018 to 2021, the median age of patients with sepsis was 82 years, with males accounting for 55% of the patients. Respiratory infections were the most common sites of infection (65%), followed by urinary tract (28%). The median length of hospital stay was 17 days. The in-hospital mortality rate was 22%.18
Changes in trends from 2010 to 2017
Only one article showed trends in the incidence and outcome of sepsis in Japan, covering approximately 2 million patients with sepsis during an 8-year period from 2010 to 2017. The mortality rate due to sepsis showed a downward trend from 25% in 2010 to 18% in 2017. However, the proportion of patients with sepsis across inpatients increased from approximately 110,000 in 2010 (3% of all inpatients) to approximately 360,000 in 2017 (5% of all inpatients). The annual number of deaths due to sepsis per 1000 inpatients has increased from 6.5 in 2010 to 8.0 in 2017. The number of deaths due to sepsis was approximately 60,000 per year in 2017, 2.3 times more than in 2010.13
Organ dysfunction
Three studies referred to the incidence of acute organ dysfunction.13, 15, 16 Each study included all patients with sepsis regardless of the infection site, with cohort sizes ranging from 1,002,638 to 2,043,073 patients. The proportions of acute organ dysfunction for cardiovascular, respiratory, renal, coagulation, and liver was 7.4%, 72.7%, 39.1%–44.7%, 10.8%–12.4%, and 3.8%–4.0%, respectively. The organ support included vasopressor administration (12.4%–12.8%), mechanical ventilation (17.7%–18.7%), and renal replacement therapy (6.7%–7.0%). In addition, DPC data were added to the Sequential Organ Failure Assessment (SOFA) scores in 2018. The most frequent SOFA score among patients with sepsis was 6 or less (62%), followed by 7–9 (19%).17
Fourteen studies focused on sepsis in specific populations. Among them, the 28-day mortality rate was 35%–40% in patients with pneumonia requiring vasopressors and/or mechanical ventilation,19, 21, 23, 27 and 20%–25% in patients with lower gastrointestinal perforation requiring vasopressors in 2010–2013.22, 24, 26, 30 The proportion of vasopressor use was 13.8% in a cohort of patients with sepsis caused by influenza pneumonia,12 whereas the proportion increased to 36.4% in a study of patients requiring mechanical ventilation due to community-acquired pneumonia.27
One study also reported annual trends in acute organ dysfunction among patients with sepsis over an 8-year period from 2010 to 2017, showing decreasing trends in renal dysfunction, coagulopathy, and hepatic dysfunction. The proportion of patients supported by mechanical ventilation or renal replacement therapy declined annually after reaching its peak in 2012, whereas the proportion of patients using vasopressor use remained at 12%.13
Clinical management
Antimicrobial therapy
Only one study compared short- and long-course antibiotic administration for patients with sepsis as a post hoc analysis of a Japanese administrative database.15 The study cohort was divided into a short-course group receiving antibiotics for ≤7 days and a long-course group receiving antibiotics for ≥8 days. The propensity score-matched analysis including 448,146 patients in each of the two groups showed significantly lower 28-day mortality in the short-course group (hazard ratio [HR] 0.94; 95% confidence interval [CI] 0.92–0.95, p < 0.001). The short-course group showed significantly longer antibiotic-free days (21 vs. 17 days, p < 0.001), shorter hospital stays (24 vs. 31 days, p < 0.001), and lower medical costs (US $8970 vs. US $9766, p < 0.001).
Antithrombin and recombinant human soluble thrombomodulin
Four studies referred to therapy for sepsis-associated DIC. In two studies using propensity score matching, the use of AT reduced the 28-day mortality rate (patients with pneumonia requiring vasopressors and/or mechanical ventilation [2194 patients in each of the two groups]; 40.6% vs. 44.2%, p = 0.02,19 lower gastrointestinal perforation [518 patients in each of the two groups]; 19.9% vs. 27.6%; difference, 7.7%; 95% CI 2.0–7.130). Two other studies using propensity score matching demonstrated no significant association between rhTM administration and 28-day mortality in patients with DIC caused by pneumonia or lower gastrointestinal perforation.21, 24
Intravenous immunoglobulin
Two studies investigating the effect of IVIG in patients with sepsis using propensity score matching showed no association between IVIG administration and 28-day mortality in patients with sepsis caused by pneumonia or lower gastrointestinal perforation.22, 23
Corticosteroid
In two studies examining the effect of low-dose corticosteroid in patients with septic shock using propensity score matching, the low-dose corticosteroid treatment reduced the mortality rate in patients with septic shock (28-day mortality rate in pneumonia, 25.3% vs. 32.6%, p = 0.01; in-hospital mortality rate in lower gastrointestinal perforation, 17.6% vs. 25.0%; difference, −7.4%; 95% CI −9.9 to −5.0).25, 27
Polymyxin B–immobilized fiber column direct hemoperfusion
Three studies investigated the effect of PMX-DHP in patients with sepsis using an administrative database. In two studies examining patients with sepsis requiring vasopressors, the PMX group showed significantly lower 28-day mortality rate than the non-PMX group (40.2% vs. 46.8%, p = 0.00331; 22.1% vs. 28.9%, p < 0.000120). By contrast, one study reported that the effect of PMX on patients with sepsis depends on the SOFA score.17 In this propensity score-matched study including 2033 patients, the 28-day mortality was significantly lower in the PMX group than in the control group with SOFA category of 7–9 (15.0% vs. 19.9%, p = 0.04) and 10–12 (18.6% and 27.4%, p = 0.0008), but not in the other SOFA categories.
Stress ulcer prophylaxis
There was one propensity score-matched study on stress ulcer prophylaxis. This study examined the benefits of stress ulcer prophylaxis using histamine-2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs) in patients with sepsis caused by lower gastrointestinal perforations between 2010 and 2015. Propensity score matching created 1088 pairs with no significant differences between the H2RA and PPI groups in gastrointestinal bleeding, Clostridioides difficile infection, or 28-day mortality (11.3% vs. 12.9%, p = 0.39).26
Dexmedetomidine
In this review, we investigated the effect of dexmedetomidine on 28-day mortality in patients with sepsis who required mechanical ventilation between 2010 and 2016. Compared with the group receiving midazolam or propofol, dexmedetomidine was associated with reduced 28-day mortality in the propensity score-matched analysis (odds ratio [OR] 0.85, 95% CI 0.80–0.91, p < 0.001).29
Location of management
In terms of location for managing patients with sepsis, two studies compared patients with sepsis in intensive care unit (ICU) and non-ICU settings.16, 28 The 30-day mortality rate was significantly lower in ICU patients. In-hospital mortality rate was also significantly lower in ICU patients (ICU: 25.8% vs. non-ICU: 29.2% [propensity score-matched analysis],16 OR 0.82, 95% CI 0.75–0.90, p < 0.001 [logistic regression analysis]28).
Medical cost of sepsis
Using a Japanese administrative database from more than 50 million hospitalized patients over an 8-year period from 2010 to 2017, a previous study examined annual trends in medical costs and cost-effectiveness for patients with sepsis.14 Along with an increasing annual number of patients with sepsis during the study period, the total annual medical spending for sepsis treatment increased from US $3.04 billion in 2010 to US $4.38 billion in 2017. Conversely, the effective cost per survivor, calculated from the gross medical cost and the number of survivors per year, as well as the cost per sepsis case, gradually declined. In the subgroup analysis by age, the proportion of total medical costs for the oldest old (≥75 years) was substantial (47.3% in 2010 and 50.5% in 2017), with a greater annual rate of growth in total medical costs than that of adults and the old (65–74 years).
DISCUSSION
Over recent years, there has been a growing body of research focused on sepsis using DPC data. Randomized controlled trials (RCTs) represent the gold standard in clinical research, providing the highest level of evidence for treatment efficacy. However, enrolling patients with sepsis in trials who require prompt diagnosis and treatment into studies within a limited timeframe poses challenges. Furthermore, these studies often include patients who meet specific predefined criteria, which may not necessarily reflect their effectiveness in real-world clinical settings. In recent times, studies leveraging DPC data, which constitute the largest available real-world data set, have emerged as a viable alternative to RCTs. Given the lack of laboratory information in DPC data and the absence of SOFA score until 2018, accurate identification of patients who align with the Sepsis-3 definition, presenting sepsis with organ dysfunction due to an infection, is a pivotal aspect in population-based studies using the administrative claims database.13 In this context, the statistics of patients with sepsis estimated by the Japanese epidemiological study using the administrative database are consistent with estimates derived from a recent Global Burden of Diseases study,2 thereby providing further validation of the adopted methodology.
In the past 8 years, the in-hospital mortality rate in patients with sepsis in Japan decreased, while the annual incidence of sepsis and death in inpatients with sepsis increased. This trend in Japan is similar to that observed worldwide. Here, we describe the epidemiology of sepsis from the 1990s to the present day. Several studies have reported a decrease in the annual mortality rate due to sepsis. A meta-analysis of 36 multicenter trials on severe sepsis showed a decrease in mortality from 46.9% between 1991 and 1995 to 29% between 2006 and 2009.32 A nationwide study in the United States showed that mortality of severe sepsis decreased from 39% to 27% between 2000 and 2007.9 Similar trends were observed in Asian countries, with the mortality rate decreasing from 30.9% in 2007 to 22.6% in 2016 in South Korea33 and from 27.8% in 2002 to 22.8% in 2012 in Taiwan.34 By contrast, the number of patients with sepsis and sepsis-related deaths are on the increase. The proportion of patients with sepsis across inpatients increased from 1.2% to 2.7% during 2005–2014 in the United States,35 from 1.21% to 1.54% during 2007–2013 in Germany,36 and from 1.3% to 2.1% during 2008–2012 in Spain.37 In addition, the number of deaths in the United States were increasing from 4.0 deaths/1000 inpatients in 2000 to 6.5 deaths/1000 inpatients in 2007; the annual absolute number of deaths increased 1.8 times (213,124 deaths in 2007)9 and from 4.9 deaths/1000 inpatients in 2003 to 6.3 deaths/1000 inpatients in 2007; the annual absolute number of deaths increased 1.3 times (207,427 deaths in 2007).38
The definition of sepsis was modified in Sepsis-3 as “Life-threatening organ dysfunction caused by a dysregulated host response to infection.” This shift has driven more studies to focus on acute organ dysfunction rather than on systemic inflammation. Using electronic medical record data from 409 US medical facilities, Rhee et al.6 found that, among a total of 173,690 patients with sepsis from 2009 to 2014, the number of patients with septic shock, acute kidney injury, hepatic dysfunction, and thrombocytopenia was 27,502 (15.8%), 75,553 (43.5%), 26,083 (15.0%), 21,830 (12.6%), respectively. In the same population, 49,400 (28.4%) and 45,088 (26.0%) received vasopressors and mechanical ventilation, respectively. In this review, the most common acute organ dysfunction were respiratory and renal, in that order, and the proportion of those requiring mechanical ventilation was about 18%. In Japan, respiratory infections (41.0%) and elderly patients (aged 65 years or older, 78.6%) are common.13 In Japan's super-aging society, the proportion of patients with respiratory failure and those requiring mechanical ventilation is expected to increase.
Only few studies have reported on the use of antibiotics in patients with sepsis, and most of them were related to the timing of antibiotic administration.39, 40 Previous studies have reported no difference in mortality or treatment failure rates between longer and shorter antibiotic durations.41, 42 However, these studies have been based on small sample sizes or on infectious diseases rather than sepsis. In the lack of high-quality evidence on sepsis, it remains controversial as to whether shorter antibiotic durations are superior to longer durations; however, the latest sepsis guidelines weakly recommend shorter antibiotic durations, but with “very low quality of evidence.”43 In this review, the short-course group had significantly more antibiotic-free days (21 vs. 17 days, p < 0.001) and shorter hospital stays (24 vs. 31 days, p < 0.001).
The Surviving Sepsis Campaign Guidelines (SSCG) 2021 did not include a section on therapy for DIC.43 The latest Japanese guidelines in 202044 weakly recommend the supplementation of rhTM for patients with sepsis-associated DIC based on a meta-analysis of three RCTs.45-47 In this review, no significant association was observed between rhTM administration and 28-day mortality in patients with DIC due to pneumonia or lower gastrointestinal perforation in 2015. These results are consistent with those of two randomized trials in patients with sepsis-associated DIC.45, 47 Furthermore, anticoagulation therapy including rhTM showed reduced mortality in critically ill patients with DIC.48 In the future, it is expected that the effects of rhTM by severity of illness are expected to be clarified in a larger cohort using a national database.
The efficacy of administering steroids for septic shock has been investigated extensively through numerous RCTs and systematic reviews. However, the findings were not always consistent due to variations in patient characteristics, diverse types and doses of administered steroids, and the heterogenous outcomes evaluated. The two studies included in this review were conducted in 2015, a period when steroid administration to patients with sepsis was limited to septic shock refractory to fluid resuscitation and vasopressors. Mortality rates have been suggested to vary by infectious organisms and site of infection,49 and these studies verified and clarified that the usage of low-dose corticosteroids was associated with reduced mortality in patients with septic shock due to lower gastrointestinal perforation tract or community-acquired pneumonia. Two large RCTs were published in 2018, one of which demonstrated no mortality benefit (ADRENAL trial),50 while the other indicated a benefit in cases of greater severity (APROCCHSS trial).51 Although the administration of steroids for sepsis remains a topic of controversy, it is plausible that specific patient cohorts may exhibit improved outcomes with such treatment. Therefore, it remains imperative to continue exploring this matter, using comprehensive cohorts derived from nationwide databases.
RCTs investigating the efficacy of PMX-DHP with survival as the primary endpoint have yielded conflicting results.52-55 The latest guidelines discourage the implementation of PMX-DHP. Nevertheless, a post hoc study of the EUPHRATES trial, the largest RCT of PMX-DHP published in 2018, revealed a significant benefit of PMX-DHP among patients with a multiple organ dysfunction score (MODS) of 10 or higher and an endotoxin activity assay (EAA) level ranging from 0.6 to 0.9.56 The study17 conducted by Fujimori et al. in 2021 corroborated previous findings, indicating that PMX-DHP could be effective in patients with an intermediate level of organ dysfunction. Currently, a new RCT is underway in the United States, aiming to verify the results of a post hoc analysis on the EUPHRATES trial within a cohort featuring an EAA level between 0.6 and 0.9 and an MODS of 10 or higher. The results of this study are forthcoming (NCT03901807).
Stress ulcer prophylaxis plays an essential role in reducing gastrointestinal bleeding in patients with sepsis.43, 44 By contrast, a meta-analysis suggested an increased risk of recurrent Clostridioides difficile infection with PPIs.57 However, no significant difference was observed in terms of efficacy and adverse events between H2 blockers and PPIs.58-60 The results in this review were consistent with those of previous reports.
In recent RCTs, the administration of dexmedetomidine did not result in a reduction of mortality in mechanically ventilated patients with sepsis.61, 62 Nevertheless, within the context of this review, a decrease in the 28-day mortality rate was observed in patients receiving dexmedetomidine.29 This finding may potentially signify an anti-inflammatory effect of dexmedetomidine.63, 64 Although this study was not an RCT, it represents propensity score-matched studies using real-world data, thereby possibly providing valuable insights into the efficacy of dexmedetomidine in actual clinical practice.
Previous guidelines have not provided clear recommendations regarding the location of management in patients with sepsis. While the SSCG 2021 recommends early ICU admission for patients requiring ICU management,43 the Japanese guidelines state that patients who do not respond to fluid resuscitation should be managed at the optimal location where ICU services are available.44 Although a comparative observational study reported that the in-hospital mortality rate was lower in critically ill patients requiring mechanical ventilation in the ICU,65, 66 in two studies of this review, a superior survival rate attributable to ICU management was also demonstrated in patients with sepsis.
The escalating cost of sepsis treatment has attracted international attention,67 yet there are few reports on the medical costs of patients with sepsis in Japan. A descriptive study of medical costs for patients with sepsis in this review showed a decrease in effective cost per survivor over the 8-year period from 2010 to 2017, while total annual medical spending for sepsis treatment increased. The study also found a larger proportion of total medical costs among the elderly aged 75 years, with a greater annual rate of growth in total medical costs compared with those aged less than 75 years. Considering the findings of this study and the increasing population of older adults in Japan,68 it is crucial to develop feasible strategies to ensure the optimal distribution of medical resources and enhance the quality of medical care.
Despite the concurrent increase in the number of patients and fatalities, the mortality rate of patients with sepsis in Japan has shown signs of improvement. While these trends are consistent with reported data from Europe and the United States, the proportion of patients and number of deaths due to sepsis tend to be higher. This trend is largely attributable to Japan's super-aging society, which is likely to escalate. To ensure the successful implementation of preventive, therapeutic, and long-term management strategies for sepsis, it is essential to gain a better understanding of the relationship between various organ dysfunctions and mortality, optimal selection of initial antimicrobial agents, efficacy of early rehabilitation, and long-term outcomes in patients with sepsis using an administrative database. DPC data lack laboratory results, including blood lactate levels and culture test results, which may reduce the accuracy of identifying patients with sepsis. It is possible that the identification of patients with sepsis using DPC data may underestimate the number of patients, as the sensitivity of the diagnostic accuracy based on DPC data for various diseases, not including sepsis, is not high.69 Therefore, studies are warranted to scrutinize the validity of using administrative databases for the identification of patients with sepsis.
CONCLUSIONS
Sepsis has a significant impact on public health, and is attracting attention as an ongoing global issue. The in-hospital mortality rate of patients with sepsis has improved; however, the incidence and number of deaths due to sepsis among inpatients have been increasing in Japan. Several countermeasures are required in the health care system to reduce the incidence of sepsis and improve the clinical outcomes of patients with sepsis. Further investigations using an administrative database may clarify the actual sepsis situation and lead to the identification of optimal strategies to save more patients with sepsis.
AUTHOR CONTRIBUTIONS
All authors provided intellectual input to the research and manuscript. T. I. contributed to the study conception and design, acquisition and interpretation of data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. T. O., N. T., D. S., and A. H. contributed to the acquisition, interpretation, and critical revision of the manuscript for important intellectual content. T. N. contributed to study conception and design, data acquisition, data interpretation, manuscript drafting, and critical revision of the manuscript for important intellectual content.
FUNDING INFORMATION
The authors received no specific funding for this work. T. N. is the CEO of Smart119 Inc. and owns stock. Smart119 Inc. had no role in the study design, data analysis, or manuscript preparation. The authors declare no conflicts of interest.
ETHICS STATEMENT
(i) Approval of the research protocol: N/A, (ii) Informed consent: N/A, (iii) Registry and the registration no. of the study/trial: N/A, (iv) Animal studies: N/A.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.