A pediatric case of multiple trauma with impending cardiac arrest due to hemorrhagic shock successfully treated with resuscitative thoracotomy: A case report
Abstract
Background
The effectiveness of resuscitative thoracotomy (RT) in pediatric patients with multiple trauma is limited. We present a pediatric case of multiple trauma successfully treated with RT.
Case Presentation
A 9-year-old boy was injured after falling down stairs. On arrival, his blood pressure was unmeasurable, and the carotid artery pulse was barely palpable. Sonographic assessment indicated intra-abdominal hemorrhage. RT and aortic cross-clamping were performed, and he received a blood transfusion, after which his circulatory status recovered. Laparotomy indicated an inferior mesenteric vein injury that was sutured. Ten hours after arrival, an acute epidural hematoma was observed and treated with an emergency craniotomy. The patient's condition remained stable and he was discharged on the 101st day.
Conclusion
RT may save the life of patients with multiple trauma, even pediatric patients, if performed in a timely manner, based on the diagnosis of hemorrhagic shock, along with rapid transfusion and hemostatic intervention.
INTRODUCTION
Trauma is the most common cause of death among children under 18 years of age.1 Mortality occurs in a high proportion of pediatric trauma cases involving head trauma.2 Hemorrhagic shock is a rare but fatal condition in patients with pediatric trauma. Recognizing hemorrhagic shock is challenging for clinicians because hypotension is unlikely to occur in children until a significant amount of blood is lost.
Resuscitative thoracotomy (RT) can be performed in patients with refractory shock.3 However, the number of reports on RT in pediatric cases is limited, and there are no guidelines regarding the indications for RT in pediatric cases. The post-RT survival rate for pediatric trauma patients is less than 10%.3, 4 As death is highly associated with severe head trauma in pediatric trauma cases,5 some experts state that RT should be withheld, especially if the trauma is caused by blunt injury.6 We report a pediatric case of multiple trauma with impending cardiac arrest due to hemorrhagic shock. Even though the patient had a traumatic brain injury, RT saved the patient's life.
CASE PRESENTATION
A 9-year-old boy, being treated for attention deficit/hyperactivity disorder, was found lying unconscious with his bicycle at the bottom of approximately 170 stairs. When a physician-staffed helicopter emergency medical system arrived at the scene, the patient exhibited impaired consciousness (Glasgow Coma Scale, E4V1M2) with anisocoria and contusion on the left side of the head. The patient also showed a state of shock; heart rate was at 123 beats/min, blood pressure was unmeasurable, respiratory rate was 30 breaths/min, and the radial artery pulse was not palpable. Above the umbilicus, there was a contusion with a herniated intestinal tract. Focused assessment with sonography for trauma (FAST) showed fluid accumulation around the spleen, liver, and cystorectal fossa. The patient was diagnosed with multiple trauma, including severe traumatic brain injury, and being in a state of shock. As the time for transfer back was suspected to be short (approximately 10 min), the physician determined to transport the patient to the university hospital after tracheal intubation and initiation of rapid fluid infusion via two peripheral venous lines. During the flight back, the attending physician sent the case information via radio wave communication to the emergency room, asked the staff to prepare for the massive blood transfusion, and convened staff for the surgery.
Upon arrival at the emergency room, his vital signs were as follows: Glasgow Coma Scale score, E1VTM1 (without any sedatives, analgesics, or muscle relaxants) and oxygen saturation (SpO2), 82% (with oxygen supplementation at 10 L/min). The patient showed sustained shock status with a heart rate of 110 beats/min, unmeasurable blood pressure, and the common carotid artery pulse was barely palpable (Table 1). Physical examination revealed a contusion on the left side of his head, a 4–5-cm contusion wound in the upper abdomen, and omental prolapse from the ruptured abdominal wall. The anisocoria had disappeared. Arterial blood gas showed mixed acidosis with pH 6.91, partial pressure of carbon dioxide (pCO2) 62.2 mmHg, partial pressure of oxygen (pO2) 240.4 mmHg, bicarbonate (HCO3) 11.7 mmol/L, base excess −19.1 mmol/L, and lactate 12.2 mmol/L. The patient was diagnosed with an impending cardiac arrest due to hemorrhagic shock associated with intra-abdominal hemorrhage. Thus, we decided to perform RT along with rapid blood transfusion.
| Time (min) | Events | Transfusion (units) | Blood pressure (mmHg), pulsation | Heart rate (beats/min) |
|---|---|---|---|---|
| 0 | Arrival to the emergency room | Unmeasurable | 110 | |
| 1 |
Start blood transfusion Perform resuscitative thoracotomy |
PRBC: 4 | Carotid artery pulsation is impalpable | 126 |
| 2 | Aortic cross-clamping | Cryoprecipitate: 3 packs | 120 | |
| 7 | Cardiac contractions clearly improved | FFP: 4 | Unmeasurable | 126 |
| 9 | Release the aortic cross-clamping | 134 | ||
| 19 | Perform whole body CT scanning | FFP: 4 | ||
| 30 |
Return back to the emergency room Aortic cross-clamping |
Carotid artery pulsation is impalpable again | 128 | |
| 33 |
Start the laparotomy (with manual compression to the abdominal aorta) Release the aortic cross-clamping |
PRBC: 4 FFP: 4 |
140 | |
| 45 | PRBC: 4 | 121/41 | 133 | |
| 83 | Finish the laparotomy | PC: 10 | 114/87 | 127 |
- Abbreviations: CT, computed tomography; FFP, fresh frozen plasma; PC, platelet concentrate; PRBC, packed red blood cell.
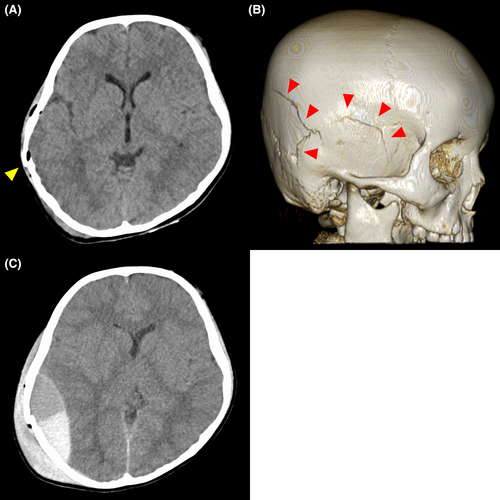
The left chest was opened with an anterolateral incision and the thoracic aorta was cross-clamped with a Satinsky clamp by an emergency physician. The heart had collapsed and ventricular contractions were reduced. After cross-clamping and rapid blood transfusion, the heart expanded, cardiac contractions improved, and the common carotid artery pulse became palpable. The patient required an emergency hemostatic laparotomy for the intra-abdominal hemorrhage and an investigation with computed tomography (CT) because of the severely altered consciousness and anisocoria at the scene, indicating severe traumatic brain injury. As the patient's circulatory status had improved sufficiently, the aortic cross-clamp was removed to prevent intra-abdominal organ ischemia and perform the CT scanning. Head CT revealed right temporal and occipital bone fractures, pneumocephalus, and acute epidural hematoma (Figure 1A,B); the latter did not show any space-occupying effects. Abdominal CT revealed extensive fluid retention in the abdominal cavity (Figure 2A,B), indicating the cause of the hemorrhagic shock.
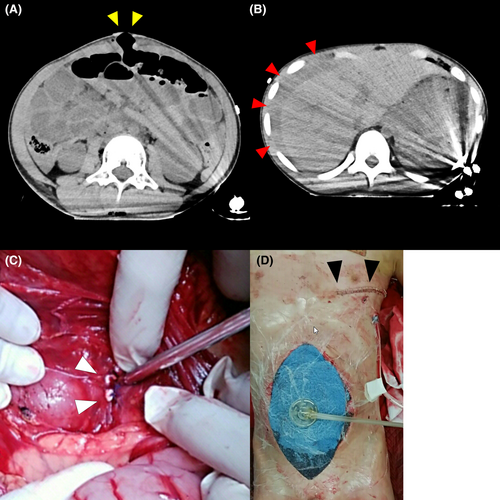
The patient's blood pressure decreased again following CT scanning, resulting in repeat aortic cross-clamping and emergency room laparotomy. The abdomen was opened for the laparotomy and the abdominal aorta was manually compressed under the diaphragm to control bleeding. The inferior mesenteric vein was lacerated, although no other intra-abdominal organ injuries were observed; the vein was sutured (Figure 2C) and open abdomen management was performed using ABTHERA (Figure 2D). CT performed postoperatively indicated no increase in the intracranial hematoma.
Anisocoria recurred on the night of admission and a CT revealed an increase in the acute epidural hematoma, which caused a midline shift (Figure 1C). Emergency craniotomy to remove the hematoma and external decompression were performed. On day 3, the planned reoperation was performed, and the injured site of the inferior mesenteric vein was settled and the abdomen was successfully closed.
Rehabilitation was initiated on day 5. A tracheostomy was performed on day 24, and mechanical ventilation was discontinued on day 28. Magnetic resonance imaging of the head was performed on day 32, and it showed findings of diffuse axonal injury on the corpus callosum and left basal ganglia, bilateral thalamus, bilateral cerebral white matter, and bilateral cerebellar hemispheres. He continued rehabilitation and was discharged home on the 101st day walking alone, although he still had symptoms such as coordination disorder of the left upper and lower extremities, decreased working memory, left homonymous hemianopsia, and left contralateral spatial neglect.
Finally, we diagnosed the patient's severity as follows: the Injury Severity Score, 26; the Revised Trauma Score, 4.2112; the probability of survival calculated with the Trauma and Injury Severity Score (TRISS), 0.69; and that calculated with the Pediatric Age-Adjusted TRISS,7 less than 0.01.
DISCUSSION
Our case indicates some points that lead to the success of the RT. First, our patient showed signs of severe shock upon arrival at the emergency room, and RT was performed when the carotid artery was barely palpable. Contrary to its use in the adult population, some reports reveal a dismal, almost universally fatal outcome for emergency department thoracotomy following blunt trauma in children.6 However, the presence of a pulse and signs of life are highly associated with saving life after RT, and a report shows a survival rate of 11% in those with signs of life.4 Therefore, the presence of these signs is necessary for making the decision to perform RT. In this case, RT by a retrieval physician before transportation is also considered. However, the retrieval physician did not perform RT on-site due to the short transport time (about 10 min). As the patient did not respond to the prehospital care and still showed signs of life, the timing of RT, in this case, would be suitable.
As the second point, the cause of the impending cardiac arrest was quickly and accurately diagnosed as hemorrhagic shock due to intra-abdominal hemorrhage, using FAST. A positive FAST result highly suggests intra-abdominal hemorrhage in pediatric patients with trauma.8 Diagnosing the cause of impending cardiac arrest may be difficult in pediatric trauma cases because of the bias that traumatic brain injury is the most common cause of death.5 RT should be performed without missing opportunities through the prompt and correct diagnosis of hemorrhagic shock.
Furthermore, rapid transfusion and hemostatic laparotomy along with RT would be critical for the success of RT. Among RT procedures, aortic cross-clamping has the effect of distributing the significantly reduced blood volume, particularly to the brain and heart, which makes time until subsequent hemostatic treatment. Our hospitals are available for severe trauma 24 h a day, and in this case, the ability to control the bleeding through prompt surgery may have saved the patient's life.
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is another option for cases with hemorrhagic shock. REBOA is less invasive than RT and the position and degree of the aortic occlusion can be adjusted; however, unlike RT, REBOA is unable to simultaneously repair cardiac injury, perform pulmonary resection, release the obstruction, and is associated with complications such as peripheral thromboembolism and lower extremity ischemia.9 Although a case of successful REBOA implementation in a pediatric patient with massive bleeding has been reported,10 REBOA has not commonly been used in pediatric cases.
In this case, the patient has a severe traumatic brain injury, but it was not a cause of impending cardiac arrest at the time of RT. RT would be futile if the cause of impending cardiac arrest is clearly diagnosed as severe head trauma. However, as in this case, when the cause of impending cardiac arrest was not clearly diagnosed as severe traumatic brain injury but with findings of hemorrhagic shock, rapid RT would be a critical procedure to save the patient's life. We believe that the RT should be considered case-by-case based on the patient's findings in a timely fashion.
CONCLUSION
RT may save a life of a patient with multiple trauma, even in a pediatric patient. RT should be performed timely for patients with signs of life, with a prompt and accurate diagnosis of hemorrhagic shock, along with adequate transfusion and rapid hemostatic intervention.
ACKNOWLEDGMENTS
We thank the entire staff at the University of Miyazaki Hospital for their help in treating this case.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: Not applicable.
Informed consent: Informed consent for publication was obtained from his parents.
Registry and the registration no. of the study/trial: Not applicable.
Animal studies: Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this case report are openly available.