Preoperative interventional radiology in penetrating posterior abdominal trauma with bowel injury: A case report
Abstract
Background
Penetrating posterior abdominal injuries pose a significant risk of retroperitoneal and intra-abdominal damage. Although interventional radiology (IR) is commonly used for hemorrhage control in trauma cases, the role of IR in penetrating bowel injuries is unclear because these injuries often require urgent surgical repair, limiting the use of IR as a primary intervention.
Case Presentation
A 76-year-old man sustained a penetrating posterior abdominal injury from a pruning shear, damaging the descending colon and lumbar arteries. Preoperative contrast-enhanced computed tomography (CT) revealed active extravasation into the colonic lumen and a retroperitoneal hematoma. A two-stage approach was implemented, starting with transcatheter arterial embolization of the lumbar artery, followed by surgical repair of the descending colon. Preoperative IR effectively controlled bleeding, enabling safe and efficient surgery.
Conclusion
Preoperative IR can help manage penetrating posterior abdominal injuries, including bowel damage, when active extravasation complicates surgery.
INTRODUCTION
Penetrating posterior abdominal injuries can cause severe retroperitoneal and intra-abdominal damage, often necessitating surgical intervention. Although interventional radiology (IR) is widely used for blunt trauma and solid organ injuries, the use of IR is limited in cases involving penetrating injuries or bowel injuries, where surgical intervention is usually prioritized. This report describes the use of preoperative IR to manage severe bleeding, enabling safe surgical intervention for penetrating injuries involving the lumbar artery.
CASE PRESENTATION
A 76-year-old man with a history of hypertension and femoral neck fracture was transported to the emergency room after a traumatic injury. On the day of presentation, he fell backward from a height of 2 m while pruning on a ladder, landing on the ground. During the fall, pruning shears penetrated more than 5 cm into the left flank. A nearby family member called for emergency assistance. Upon arrival of the emergency medical service, the foreign body had been removed by bystanders. Compression was applied to control the bleeding. However, active external bleeding from the flank persisted.
The patient was transported to the emergency room approximately 1 hour after the injury. On presentation, his vital signs were as follows: blood pressure, 160/87 mmHg; heart rate, 74 beats/min; respiratory rate, 31 breaths/min; and oxygen saturation, 100% with supplemental oxygen (10 L/min). The Glasgow Coma Scale score was E4V5M6, and he had severe pain in the flank region with peripheral coldness, peritoneal irritation sign, and agitation. A transfusion of four units of packed red blood cells and four units of fresh frozen plasma was initiated. Airway intubation was performed because of shock and agitation. Contrast-enhanced computed tomography (CT) revealed a retroperitoneal hematoma extending from the left iliopsoas muscle near the third lumbar vertebra to the descending colon, with evidence of extravasation into the descending colon (Figure 1). Based on these findings, a diagnosis of injury to the descending colon due to penetrating trauma was made. No other significant injuries were observed.
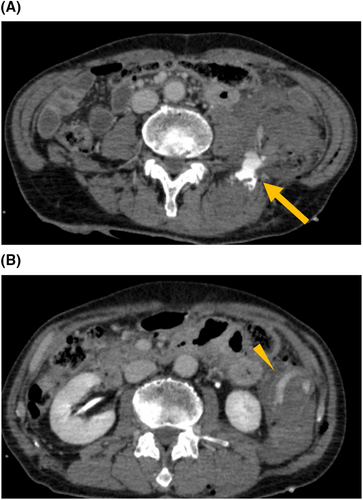
Blood gas analysis revealed a hemoglobin level of 12.5 g/dL, indicating mild anemia. However, within 1.5 h of arrival, blood pressure dropped to 80/54 mmHg, and hemoglobin level decreased to 10.4 g/dL, indicating worsening anemia. Emergency surgery was considered; however, persistent bleeding from the deep retroperitoneal space could complicate surgical management. Therefore, a two-stage approach was planned, starting with percutaneous arterial embolization to control the bleeding, followed by exploratory laparotomy for hemostasis and resection of the descending colon.
DETAILS OF INTERVENTIONAL RADIOLOGY PROCEDURE
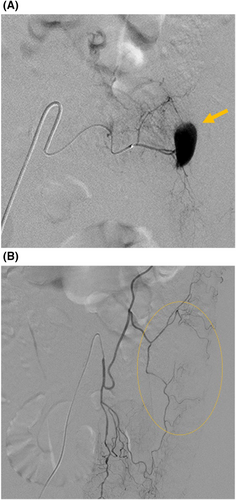
A 4-Fr short sheath was placed in the right femoral artery. Based on CT findings, the left fourth lumbar artery suspected of being injured was selected using a 4-Fr Shepherd hook catheter, and angiography was performed. Disruption of the distal segment of the artery was observed. A 2.6-Fr high-flow catheter was advanced into the lumbar artery, and repeat angiography revealed extravasation from the distal branch of the lumbar artery (Figure 2). Embolization was performed using gelatin sponge particles, and posttreatment angiography confirmed successful embolization. After hemostasis, blood pressure rapidly increased to 124/71 mmHg. Angiography of the inferior mesenteric artery showed no obvious injury or extravasation. Nonetheless, a hypovascular region in the mid-descending colon suggested bowel compression by the surrounding hematoma. The duration of IR was 24 min, and the total IR room stay was 50 min.
OPERATIVE FINDINGS
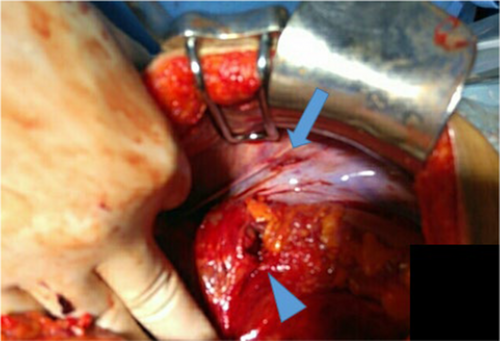
A midline incision was made from the upper to the lower abdomen, revealing approximately 500 mL of hemoperitoneum. Five-point packing was done. Examination revealed a little less than 50% laceration of the circumference of the descending colon (American Association for the Surgery of Trauma grade II), 10 cm distal to the splenic flexure, with fecal contamination in the left abdomen (Figure 3). There was a small retroperitoneal hematoma in the left Zone II and a 3-cm peritoneal laceration in the left flank, consistent with the pruning shears' trajectory. No injuries to the small intestine, other organs, or retroperitoneum beyond Zone II were found. After mobilizing the left colon and splenic flexure, the injured segment (5 cm proximally and distally) was resected using a linear stapler. Functional end-to-end anastomosis was performed with staple line reinforcement. Given the fecal contamination and retroperitoneal hematoma, which posed a risk of secondary anastomotic leakage from a retroperitoneal abscess, a diverting loop ileostomy was created 30 cm proximal to the ileocecal valve and fixed to the right lower quadrant. The abdominal cavity was irrigated with 10 L of warm saline. In the intensive care unit, the posterior wound was irrigated with 500 mL of saline and sutured. The patient was transferred to the general ward on postoperative day 4 without complications.
DISCUSSION
This case highlights two key points. First, preoperative contrast-enhanced CT can improve decision-making in the management of penetrating posterior abdominal trauma. Second, in cases of penetrating trauma or bowel injuries, which are typically managed surgically, initiating treatment with IR may be more beneficial in certain situations.
Penetrating injuries to the posterior abdomen carry an elevated risk of retroperitoneal and intra-abdominal organ damage, potentially leading to severe complications.1 The colon is the most commonly injured organ, and colon injuries may cause peritonitis, necrotizing fasciitis, and sepsis, necessitating surgical intervention. Injuries to the kidney, ureter, spleen, diaphragm, small intestine, and pancreas require surgery in cases of hemodynamic instability, pneumoperitoneum, or ureteral injury.2 CT scans provide valuable information on these complex injuries. In this case, organ injuries were identified, and the rare condition of lumbar artery injury with extravasation into the colon lumen was visualized, improving treatment decision-making.
The role of IR in penetrating trauma and bowel injury is unclear,3 likely because these injuries often require surgical repair, limiting the use of IR as a primary intervention. In contrast, damage control IR has gained acceptance for blunt trauma as a complement to surgery for hemorrhage control, particularly in liver, splenic, and pelvic injuries.4 Retroperitoneal hemorrhage is difficult to control surgically because of the anatomical complexity and the challenge of achieving hemostasis. Lumbar artery injuries can cause persistent bleeding that is difficult to access via laparotomy, and retroperitoneal decompression may worsen hemorrhage by impairing the tamponade effect. In contrast, transarterial embolization is a standard treatment for lumbar artery bleeding in stable or resuscitated patients.5
In this case, anticipating the challenges in surgical hemostasis for vascular injuries in the retroperitoneal space—where achieving proximal and distal control and ensuring adequate visualization is difficult—a two-stage approach was employed, starting with preoperative IR for lumbar artery embolization, followed by surgery. This strategy improved visualization, enabling safe and efficient surgical repair. This case suggests that in penetrating posterior abdominal trauma with major vascular injuries, including those in the lumbar artery, where surgical hemostasis is difficult, IR can offer more effective care, even when additional surgical interventions are needed.
The successful outcome also highlights the importance of a multidisciplinary approach. Close cooperation between trauma surgeons, emergency physicians, and interventional radiologists, as well as easy access to CT, is crucial in cases where severe abdominal trauma involves multiple critical organs or vascular injury.
CONCLUSION
Preoperative IR may be an effective strategy for hemorrhage control in complex penetrating posterior abdominal injuries, including bowel injuries. IR can facilitate surgery and improve outcomes in selected cases.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: Informed consent for publication was obtained from the patient.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
Supporting data for this study can be obtained from the corresponding author upon reasonable request. However, the data are not openly available due to privacy and ethical considerations.