Intranasal Calcitriol Accelerates Improvement of Sinonasal Inflammation and Olfactory Impairment in Mice After Cessation of Chronic Cigarette-Smoke Exposure
Logan Langerude
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorAlex McQuiston
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorCarl Atkinson
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorCorresponding Author
Jennifer K. Mulligan
Division of Division of Rhinology & Skull Base Surgery Department of Otolaryngology, University of Florida, Gainesville, Florida, USA
Correspondence: Jennifer K. Mulligan ([email protected])
Search for more papers by this authorLogan Langerude
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorAlex McQuiston
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorCarl Atkinson
Department of Surgery, Department of Pediatrics, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA
Search for more papers by this authorCorresponding Author
Jennifer K. Mulligan
Division of Division of Rhinology & Skull Base Surgery Department of Otolaryngology, University of Florida, Gainesville, Florida, USA
Correspondence: Jennifer K. Mulligan ([email protected])
Search for more papers by this authorFunding: Research reported in this publication was supported by the National Institutes of Health Awards R01AI134698 (J.K.M.), R01AI144364 (J.K.M. and C.A.), and R01HL140470 (C.A.).
ABSTRACT
Rationale
Smoking has been shown to be associated with circulating deficiencies in 25(OH)D3 and reduced sinonasal tissue levels of the active form of vitamin D, 1,25(OH)2D3. Given vitamin D's ability to reduce inflammation, we sought to examine if intranasal (IN) delivery of calcitriol [clinical analog of 1,25(OH)2D3] could reduce inflammation and improve disease severity in a murine model of chronic cigarette smoke-induced sinonasal inflammation (CS-SI).
Methods
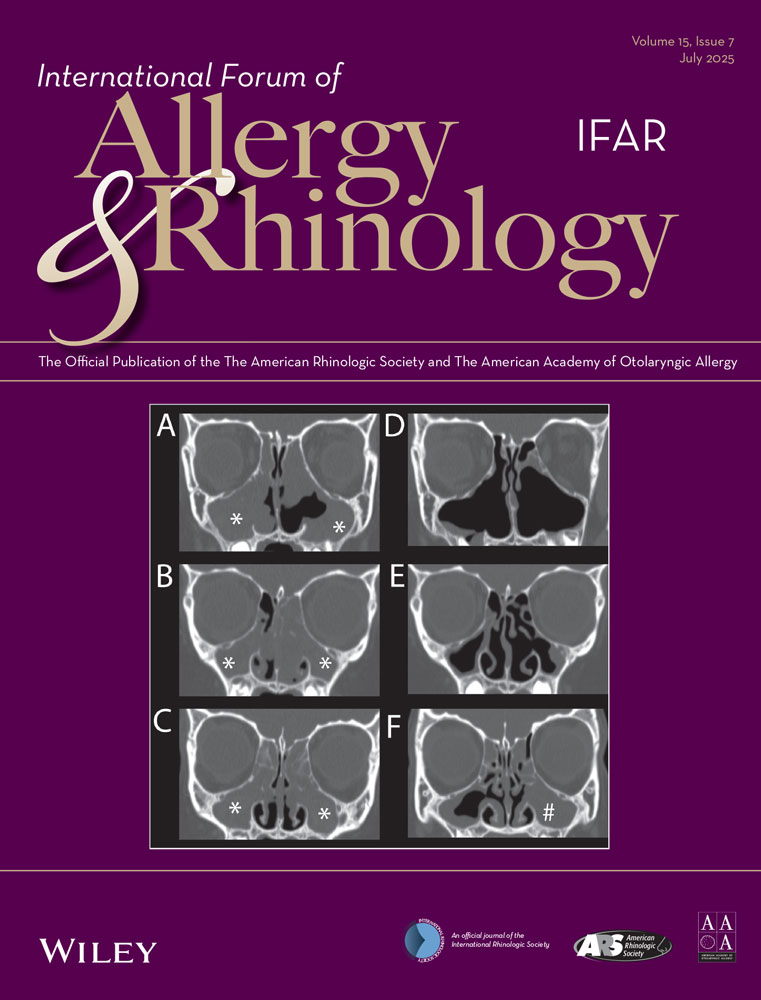
Mice were exposed to CS 5 h/day, 5 days/week for 9 months, and then began IN calcitriol three times per week for 4 weeks. Micro-CT was used to assess disease severity. Sinonasal tissues were collected for RNA-seq analysis. Olfactory function was assessed using a T-maze odorant avoidance sniff behavior test. Nasal lavage fluid (NALF) was used for cytology and cytokines analysis.
Results
Quantification of disease severity by micro-CT showed IN calcitriol reduced opacification by 18%, as compared to smoke cessation alone, in which only a 5% reduction was noted. H&E analysis of NAFL demonstrated heightened neutrophil infiltration and neutrophil-associated chemokines in CS-SI mice, which was reduced with IN calcitriol treatment. RNA-seq pathway analysis demonstrated that smoking was associated with odorant binding changes and that calcitriol treatment reduced neutrophil migration and inflammation. Lastly, IN calcitriol reversed olfactory loss caused in CS-SI.
Conclusions
IN delivery of calcitriol accelerates inflammatory resolution in the nose and olfactory mucosa after prolonged CS exposure. Furthermore, treatment was associated with improved olfactory function in mice CS-SI, as such local delivery of calcitriol may serve as a novel treatment for modulating sinonasal inflammation.
Conflicts of Interest
J.K.M. is senior advisor for 3D Matrix Medical Technologies. None of the other listed authors have any potential conflicts to disclose related to the research presented herein.
Supporting Information
| Filename | Description |
|---|---|
| alr23504-sup-0001-figuresS1-S2.docx196.3 KB | Supporting information |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1B. W. Hollis and C. L. Wagner, “Clinical Review: The Role of the Parent Compound Vitamin D With Respect to Metabolism and Function: Why Clinical Dose Intervals Can Affect Clinical Outcomes,” The Journal of Clinical Endocrinology and Metabolism 98, no. 12 (2013): 4619–4628, https://doi.org/10.1210/jc.2013-2653.
- 2M. Hewison, “Vitamin D and the Intracrinology of Innate Immunity,” Molecular and Cellular Endocrinology 321, no. 2 (2010): 103–111, https://doi.org/10.1016/j.mce.2010.02.013.
- 3J. M. Brehm, J. C. Celedon, M. E. Soto-Quiros, et al., “Serum Vitamin D Levels and Markers of Severity of Childhood Asthma in Costa Rica,” American Journal of Respiratory and Critical Care Medicine 179, no. 9 (2009): 765–771, https://doi.org/10.1164/rccm.200808-1361OC.
- 4A. A. Ginde, J. M. Mansbach, and C. A. Camargo, “Association Between Serum 25-hydroxyvitamin D Level and Upper respiratory Tract Infection in the Third National Health and Nutrition Examination Survey,” Archives of Internal Medicine 169, no. 4 (2009): 384–390, https://doi.org/10.1001/archinternmed.2008.560.
- 5J. K. Mulligan, B. S. Bleier, B. O'Connell, R. M. Mulligan, C. Wagner, and R. J. Schlosser, “Vitamin D3 Correlates Inversely With Systemic Dendritic Cell Numbers and Bone Erosion in Chronic Rhinosinusitis With Nasal Polyps and Allergic Fungal Rhinosinusitis,” Clinical and Experimental Immunology 164, no. 3 (2011): 312–320, https://doi.org/10.1111/j.1365-2249.2011.04325.x.
- 6R. J. Schlosser, Z. M. Soler, G. W. Schmedes, K. Storck, and J. K. Mulligan, “Impact of Vitamin D Deficiency Upon Clinical Presentation in Nasal Polyposis,” International Forum of Allergy & Rhinology 4, no. 3 (2014): 196–199, https://doi.org/10.1002/alr.21274.
- 7J. K. Mulligan, W. N. Pasquini, W. W. Carroll, et al., “Dietary Vitamin D3 Deficiency Exacerbates Sinonasal Inflammation and Alters Local 25(OH)D3 Metabolism,” PLoS ONE 12, no. 10 (2017): e0186374, https://doi.org/10.1371/journal.pone.0186374.
- 8D. R. Murdoch, S. Slow, S. T. Chambers, et al., “Effect of Vitamin D3 Supplementation on Upper respiratory Tract Infections in Healthy Adults: The VIDARIS Randomized Controlled Trial,” JAMA: The Journal of the American Medical Association 308, no. 13 (2012): 1333–1339, https://doi.org/10.1001/jama.2012.12505.
- 9S. M. Tse, H. W. Kelly, A. A. Litonjua, M. L. Van Natta, S. T. Weiss, and K. G. Tantisira, “Corticosteroid Use and Bone Mineral Accretion in Children With Asthma: Effect Modification by Vitamin D,” The Journal of Allergy and Clinical Immunology 130, no. 1 (2012): 53–60, https://doi.org/10.1016/j.jaci.2012.04.005. e4.
- 10M. Urashima, T. Segawa, M. Okazaki, M. Kurihara, Y. Wada, and H. Ida, “Randomized Trial of Vitamin D Supplementation to Prevent Seasonal Influenza A in Schoolchildren,” The American Journal of Clinical Nutrition 91, no. 5 (2010): 1255–1260, https://doi.org/10.3945/ajcn.2009.29094.
- 11E. Lewis, C. Fernandez, A. Nella, R. Hopp, J. C. Gallagher, and T. B. Casale, “Relationship of 25-Hydroxyvitamin D and Asthma Control in Children,” Annals of Allergy, Asthma & Immunology: Official Publication of the American College of Allergy, Asthma, & Immunology 108, no. 4 (2012): 281–282, https://doi.org/10.1016/j.anai.2012.01.003.
- 12S. M. Bjerk, B. D. Edgington, T. S. Rector, and K. M. Kunisaki, “Supplemental Vitamin D and Physical Performance in COPD: A Pilot Randomized Trial,” International Journal of Chronic Obstructive Pulmonary Disease 8 (2013): 97–104, https://doi.org/10.2147/COPD.S40885.
- 13A. M. Tolppanen, A. Sayers, R. Granell, W. D. Fraser, J. Henderson, and D. A. Lawlor, “Prospective Association of 25-Hydroxyvitamin d3 and d2 With Childhood Lung Function, Asthma, Wheezing, and Flexural Dermatitis,” Epidemiology (Cambridge, MA) 24, no. 2 (2013): 310–319, https://doi.org/10.1097/EDE.obo13e318280dd5e.
- 14M. Castro, T. S. King, S. J. Kunselman, et al., “National Heart L, Blood Institute's A. Effect of Vitamin D3 on Asthma Treatment Failures in Adults With Symptomatic Asthma and Lower Vitamin D Levels: The VIDA Randomized Clinical Trial,” Jama 311, no. 20 (2014): 2083–2091, https://doi.org/10.1001/jama.2014.5052.
- 15J. Jiao, T. S. King, M. McKenzie, et al., “Vitamin D3 Therapy in Patients With Asthma Complicated by Sinonasal Disease: Secondary Analysis of the Vitamin D Add-on Therapy Enhances Corticosteroid Responsiveness in Asthma Trial,” The Journal of Allergy and Clinical Immunology 138, no. 2 (2016): 589–592, https://doi.org/10.1016/j.jaci.2015.12.1329. e2.
- 16D. A. Jolliffe, C. Stefanidis, Z. Wang, et al., “Vitamin D Metabolism Is Dysregulated in Asthma and Chronic Obstructive Pulmonary Disease,” American Journal of Respiratory and Critical Care Medicine 202 (2020), https://doi.org/10.1164/rccm.201909-1867OC.
- 17K. Robien, S. J. Oppeneer, J. A. Kelly, and H.-R. JM, “Drug-Vitamin D Interactions: A Systematic Review of the Literature,” Nutrition in Clinical Practice 28, no. 2 (2013): 194–208, https://doi.org/10.1177/0884533612467824.
- 18D. Zehnder, R. Bland, M. C. Williams, et al., “Extrarenal Expression of 25-Hydroxyvitamin D(3)-1 Alpha-hydroxylase,” Journal of Clinical Endocrinology and Metabolism 86, no. 2 (2001): 888–894, https://doi.org/10.1210/jcem.86.2.7220.
- 19M. Hewison, D. Zehnder, R. Bland, and P. Stewart, “1alpha-Hydroxylase and the Action of Vitamin D,” Journal of Molecular Endocrinology 25, no. 2 (2000): 141–148, https://doi.org/10.1677/jme.0.0250141.
- 20S. Hansdottir, M. M. Monick, S. L. Hinde, N. Lovan, D. C. Look, and G. W. Hunninghake, “Respiratory Epithelial Cells Convert Inactive Vitamin D to Its Active Form: Potential Effects on Host Defense,” Journal of Immunology (Baltimore, Md.: 1950) 181, no. 10 (2008): 7090–7099.
- 21J. K. Mulligan, D. R. White, E. W. Wang, et al. “ Vitamin D3 Deficiency Increases Sinus Mucosa Dendritic Cells in Pediatric Chronic Rhinosinusitis with Nasal Polyps”, Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery 147, no. 4 (2012): 773–781. https://doi.org/10.1177/0194599812448852.
10.1177/0194599812448852 Google Scholar
- 22J. A. Tamblyn, R. Susarla, C. Jenkinson, et al., “Dysregulation of Maternal and Placental Vitamin D Metabolism in Preeclampsia,” Placenta 50 (2017): 70–77, https://doi.org/10.1016/j.placenta.2016.12.019.
- 23J. S. Adams, B. Rafison, S. Witzel, et al., “Regulation of the Extrarenal CYP27B1-Hydroxylase,” Journal of Steroid Biochemistry and Molecular Biology 144 (2014): 22–27, https://doi.org/10.1016/j.jsbmb.2013.12.009. Pt A.
- 24S. Christakos, M. Hewison, D. G. Gardner, et al., “Vitamin D: Beyond Bone,” Annals of the New York Academy of Sciences 1287 (2013): 45–58, https://doi.org/10.1111/nyas.12129.
- 25R. J. Schlosser, W. W. Carroll, Z. M. Soler, W. N. Pasquini, and J. K. Mulligan, “Reduced Sinonasal Levels of 1-Alpha-Hydroxylase Are Associated With Worse Quality of Life in Chronic Rhinosinusitis With Nasal Polyps,” International Forum of Allergy & Rhinology 6, no. 1 (2016): 58–65, https://doi.org/10.1002/alr.21576.
- 26J. K. Mulligan, W. Nagel, B. P. O'Connell, J. Wentzel, C. Atkinson, and R. J. Schlosser, “Cigarette Smoke Exposure Is Associated With Vitamin D3 Deficiencies in Patients With Chronic Rhinosinusitis,” The Journal of Allergy and Clinical Immunology 134, no. 2 (2014): 342–349, https://doi.org/10.1016/j.jaci.2014.01.039.
- 27J. K. Mulligan, D. Nord, M. V. Villanueva, et al., “Role of C3a as a Novel Regulator of 25(OH)D3 to 1-Alpha,25-Dihydroxyvitamin D3 Metabolism in Upper Airway Epithelial Cells,” Journal of Immunology (Baltimore, Md.: 1950) 209, no. 2 (2022): 262–269, https://doi.org/10.4049/jimmunol.2000726.
- 28D. Risso, D. Drayna, and G. Morini, “Alteration, Reduction and Taste Loss: Main Causes and Potential Implications on Dietary Habits,” Nutrients 12, no. 11 (2020), https://doi.org/10.3390/nu12113284.
- 29I. Croy, S. Nordin, and T. Hummel, “Olfactory Disorders and Quality of Life—An Updated Review,” Chemical Senses 39, no. 3 (2014): 185–194, https://doi.org/10.1093/chemse/bjt072.
- 30J. James, A. M. Tsvik, S. Y. Chung, J. Usseglio, D. A. Gudis, and J. B. Overdevest, “Association Between Social Determinants of Health and Olfactory Function: A Scoping Review,” International Forum of Allergy & Rhinology 11, no. 10 (2021): 1472–1493, https://doi.org/10.1002/alr.22822.
- 31R. Ueha, S. Ueha, K. Kondo, et al., “Damage to Olfactory Progenitor Cells Is Involved in Cigarette Smoke-Induced Olfactory Dysfunction in Mice,” The American Journal of Pathology 186, no. 3 (2016): 579–586, https://doi.org/10.1016/j.ajpath.2015.11.009.
- 32R. Ueha, S. Ueha, K. Kondo, S. Kikuta, and T. Yamasoba, “Cigarette Smoke-Induced Cell Death Causes Persistent Olfactory Dysfunction in Aged Mice,” Frontiers in Aging Neuroscience 10 (2018): 183, https://doi.org/10.3389/fnagi.2018.00183.
- 33R. Ueha, S. Ueha, T. Sakamoto, et al., “Cigarette Smoke Delays Regeneration of the Olfactory Epithelium in Mice,” Neurotoxicity Research 30, no. 2 (2016): 213–224, https://doi.org/10.1007/s12640-016-9617-5.
- 34A. Woodell, B. W. Jones, T. Williamson, et al., “A Targeted Inhibitor of the Alternative Complement Pathway Accelerates Recovery from Smoke-Induced Ocular Injury,” Investigative Ophthalmology & Visual Science 57, no. 4 (2016): 1728–1737, https://doi.org/10.1167/iovs.15-18471.
- 35K. J. Patel, Q. Cheng, S. Stephenson, et al., “Emphysema-Associated Autoreactive Antibodies Exacerbate Post-Lung Transplant Ischemia-Reperfusion Injury,” American Journal of Respiratory Cell and Molecular Biology 60, no. 6 (2019): 678–686, https://doi.org/10.1165/rcmb.2018-0224OC.
- 36B. S. Bleier, R. M. Mulligan, and R. J. Schlosser, “Primary Human Sinonasal Epithelial Cell Culture Model for Topical Drug Delivery in Patients With Chronic Rhinosinusitis With Nasal Polyposis,” The Journal of Pharmacy and Pharmacology 64, no. 3 (2012): 449–456, https://doi.org/10.1111/j.2042-7158.2011.01409.x.
- 37J. K. Mulligan, W. Nagel, B. P. O'Connell, J. Wentzel, C. Atkinson, and R. J. Schlosser, “Cigarette Smoke Exposure Is Associated With Vitamin D3 Deficiencies in Patients With Chronic Rhinosinusitis,” The Journal of Allergy and Clinical Immunology 134, no. 2 (2014): 342–349.
- 38J. K. Mulligan, R. M. Mulligan, C. Atkinson, and R. J. Schlosser, “Human Sinonasal Epithelial Cells Direct Dendritic Function and T-cell T Helper 1/T Helper 2 Skewing Following Aspergillus Exposure,” International Forum of Allergy & Rhinology 1, no. 4 (2011): 268–274, https://doi.org/10.1002/alr.20055.
- 39J. K. Mulligan, B. P. O'Connell, W. Pasquini, et al. “ Impact of Tobacco Smoke on Upper Airway Dendritic Cell Accumulation and Regulation by Sinonasal Epithelial Cells”, International Forum of Allergy & Rhinology 7 (2017): 777–785. https://doi.org/10.1002/alr.21955.
10.1002/alr.21955 Google Scholar
- 40R. Mahadeva, C. Atkinson, Z. Li, et al., “Polymers of Z Alpha1-Antitrypsin Co-Localize With Neutrophils in Emphysematous Alveoli and Are Chemotactic in Vivo,” The American Journal of Pathology 166, no. 2 (2005): 377–386.
- 41G. T. Motz, B. L. Eppert, G. Sun, et al., “Persistence of Lung CD8 T Cell Oligoclonal Expansions Upon Smoking Cessation in a Mouse Model of Cigarette Smoke-Induced Emphysema,” Journal of Immunology (Baltimore, Md.: 1950) 181, no. 11 (2008): 8036–8043, https://doi.org/10.4049/jimmunol.181.11.8036.
- 42M. C. Duan, H. J. Tang, X. N. Zhong, and Y. Huang, “Persistence of Th17/Tc17 Cell Expression Upon Smoking Cessation in Mice With Cigarette Smoke-induced Emphysema,” Clinical & Developmental Immunology 2013 (2013): 350727, https://doi.org/10.1155/2013/350727.
- 43G. De Cunto, B. Bartalesi, E. Cavarra, E. Balzano, G. Lungarella, and M. Lucattelli, “Ongoing Lung Inflammation and Disease Progression in Mice After Smoking Cessation: Beneficial Effects of Formyl-Peptide Receptor Blockade,” The American Journal of Pathology 188, no. 10 (2018): 2195–2206, https://doi.org/10.1016/j.ajpath.2018.06.010.
- 44C. Ren, Y. K. Mou, X. Y. Song, et al., “P2×7 Receptor of Microglia in Olfactory Bulb Mediates the Pathogenesis of Olfactory Dysfunction in a Mouse Model of Allergic Rhinitis,” FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology 37, no. 6 (2023): e22955, https://doi.org/10.1096/fj.202300160RR.
- 45M. Li, P. Hener, Z. Zhang, S. Kato, D. Metzger, and P. Chambon, “Topical Vitamin D3 and Low-Calcemic Analogs Induce Thymic Stromal Lymphopoietin in Mouse Keratinocytes and Trigger an Atopic Dermatitis,” PNAS 103, no. 31 (2006): 11736–11741, https://doi.org/10.1073/pnas.0604575103.
- 46J. K. Mulligan, K. Patel, T. Williamson, et al., “C3a receptor Antagonism as a Novel Therapeutic Target for Chronic Rhinosinusitis,” Mucosal Immunology 11, no. 5 (2018): 1375–1385, https://doi.org/10.1038/s41385-018-0048-x.
- 47S. D. Shapiro, N. M. Goldstein, A. M. Houghton, D. K. Kobayashi, D. Kelley, and A. Belaaouaj, “Neutrophil Elastase Contributes to Cigarette Smoke-Induced Emphysema in Mice,” The American Journal of Pathology 163, no. 6 (2003): 2329–2335, https://doi.org/10.1016/s0002-9440(10)63589-4.
- 48J. H. Turner, L. May, R. R. Reed, and A. P. Lane, “Reversible Loss of Neuronal Marker Protein Expression in a Transgenic Mouse Model for Sinusitis-Associated Olfactory Dysfunction,” American Journal of Rhinology & Allergy 24, no. 3 (2010): 192–196, https://doi.org/10.2500/ajra.2010.24.3460.
- 49W. H. Huang, Y. W. Hung, W. Hung, M. Y. Lan, and C. F. Yeh, “Murine Model of Eosinophilic Chronic Rhinosinusitis With Nasal Polyposis Inducing Neuroinflammation and Olfactory Dysfunction,” The Journal of Allergy and Clinical Immunology 154, no. 2 (2024): 325–339, https://doi.org/10.1016/j.jaci.2024.02.021.e3.
- 50A. Strzelak, A. Ratajczak, A. Adamiec, and W. Feleszko, “Tobacco Smoke Induces and Alters Immune Responses in the Lung Triggering Inflammation, Allergy, Asthma and Other Lung Diseases: A Mechanistic Review,” International Journal of Environmental Research and Public Health 15, no. 5 (2018): 1033, https://doi.org/10.3390/ijerph15051033.
- 51C. Bourgon, A. S. Albin, O. Ando-Grard, et al., “Neutrophils Play a Major Role in the Destruction of the Olfactory Epithelium During SARS-CoV-2 Infection in Hamsters,” Cellular and Molecular Life Sciences: CMLS 79, no. 12 (2022): 616, https://doi.org/10.1007/s00018-022-04643-1.
- 52X. Wang, Y. Sima, Y. Zhao, et al., “Endotypes of Chronic Rhinosinusitis Based on Inflammatory and Remodeling Factors,” The Journal of Allergy and Clinical Immunology 151, no. 2 (2023): 458–468, https://doi.org/10.1016/j.jaci.2022.10.010.
- 53A. Brunet, J. Milara, S. Frías, J. Cortijo, and M. Armengot, “Molecular and Clinical Predictors of Quality of Life in Chronic Rhinosinusitis With Nasal Polyps,” Journal of Clinical Medicine 12, no. 4 (2023): 1391, https://doi.org/10.3390/jcm12041391.
- 54G. M. Oakley, R. J. Harvey, and V. J. Lund, “The Role of Macrolides in Chronic Rhinosinusitis (CRSsNP and CRSwNP),” Current Allergy and Asthma Reports 17, no. 5 (2017): 30, https://doi.org/10.1007/s11882-017-0696-z.
- 55T. L. Smith, R. J. Schlosser, Z. M. Soler, et al., “Olfactory Cleft Mucus Inflammatory Proteins in CRS: A Case-Control Study,” International Forum of Allergy & Rhinology 11, no. 9 (2021): 1321–1335, https://doi.org/10.1002/alr.22770.
- 56D. W. Kim, K. M. Eun, E. Y. Roh, S. Shin, and D. K. Kim, “Chronic Rhinosinusitis Without Nasal Polyps in Asian Patients Shows Mixed Inflammatory Patterns and Neutrophil-Related Disease Severity,” Mediators of Inflammation 2019 (2019): 7138643, https://doi.org/10.1155/2019/7138643.
- 57J. A. Poposki, A. I. Klingler, W. W. Stevens, et al., “Elevation of Activated Neutrophils in Chronic Rhinosinusitis With Nasal Polyps,” Journal of Allergy and Clinical Immunology 149, no. 5 (2022): 1666–1674, https://doi.org/10.1016/j.jaci.2021.11.023.
- 58G. Bigman, “Age-Related Smell and Taste Impairments and Vitamin D Associations in the U.S. Adults National Health and Nutrition Examination Survey,” Nutrients 12, no. 4 (2020), 984, https://doi.org/10.3390/nu12040984.
- 59Y. H. Shin, E. K. Ha, J. H. Kim, et al., “Serum Vitamin D Level is Associated with Smell Dysfunction Independently of Aeroallergen Sensitization, Nasal Obstruction, and the Presence of Allergic Rhinitis in Children,” Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology 32, no. 1 (2021): 116–123. https://doi.org/10.1111/pai.13341.
- 60J. E. Kim, E. Oh, J. Park, J. Youn, J. S. Kim, and W. Jang, "Serum 25-Hydroxyvitamin D3 Level May be Associated With Olfactory Dysfunction in De Novo Parkinson's Disease," Journal of Clinical Neuroscience 57 (2018): 131–135. https://doi.org/10.1016/j.jocn.2018.08.003.
- 61Z. Gao, Z. Danzhen, J. Zhu, Y. Li, Z. Xu, and L. Chu, "Vitamin D Levels and Olfactory Dysfunction in Multiple Sclerosis Patients," International Journal of Neuroscience (2024): 1-8. https://doi.org/10.1080/00207454.2024.2304081.
- 62W. W. Carroll, R. J. Schlosser, B. P. O'Connell, Z. M. Soler, and J. K. Mulligan, "Vitamin D Deficiency Is Associated With Increased Human Sinonasal Fibroblast Proliferation in Chronic Rhinosinusitis With Nasal Polyps," International Forum of Allergy & Rhinology 6, no. 6 (2016): 605–610. https://doi.org/10.1002/alr.21704.