‘Hydro-point’ – The forgotten and unspoken entity in hydropneumothorax
Abstract
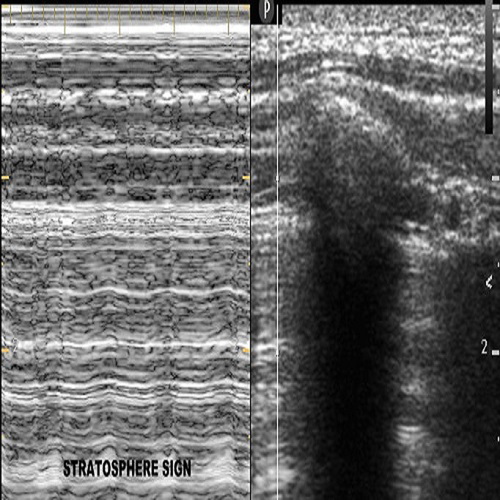
Effusive pneumothorax is an abnormal collection of air and fluid within the pleural space: blood, pus, or serous fluid. Thus, effusive pneumothorax can be categorized as hemopneumothorax, pyopneumothorax, or hydropneumothorax, depending on the type of fluid accumulation. Hydropneumothorax is a clinical condition defined by the presence of air and serous fluid within the pleura space. Hydropneumothorax is one of the common respiratory emergencies encountered in the emergency department in India. Etiologies can be classified into infectious and non-infectious causes, among which tuberculosis being the most common one. Point of care ultrasound (POCUS) can help diagnose hydropneumothorax at the bedside rather than shift the patient for an X-ray. Here, we describe a case of hydropneumothorax, which was diagnosed using POCUS by characteristic sonographic signs, namely “Hydro-point” and “barcode-hydro point-sinusoidal sign.” Sonographic hydro-point is the transition zone of the air-fluid interface, which is seen in hydropneumothorax. Targhetta et al., in 1992, introduced the term “Hydro-point” in lung ultrasound for diagnosing hydropneumothorax but has been under-reported/unspoken much in the literature. With the use of POCUS, we diagnosed and stabilized the patient in the Emergency Department.
Case Report
A 30-year-old chronic smoker presented to our emergency department with a history of breathlessness, cough with expectoration, and right-sided chest pain for the past four days. On initial assessment, the patient’s saturation was low (50% in room air), and right-sided air entry was absent. Hence, the patient was started on high flow oxygen and saturation improved to 90%. Other assessments and vital signs were normal.
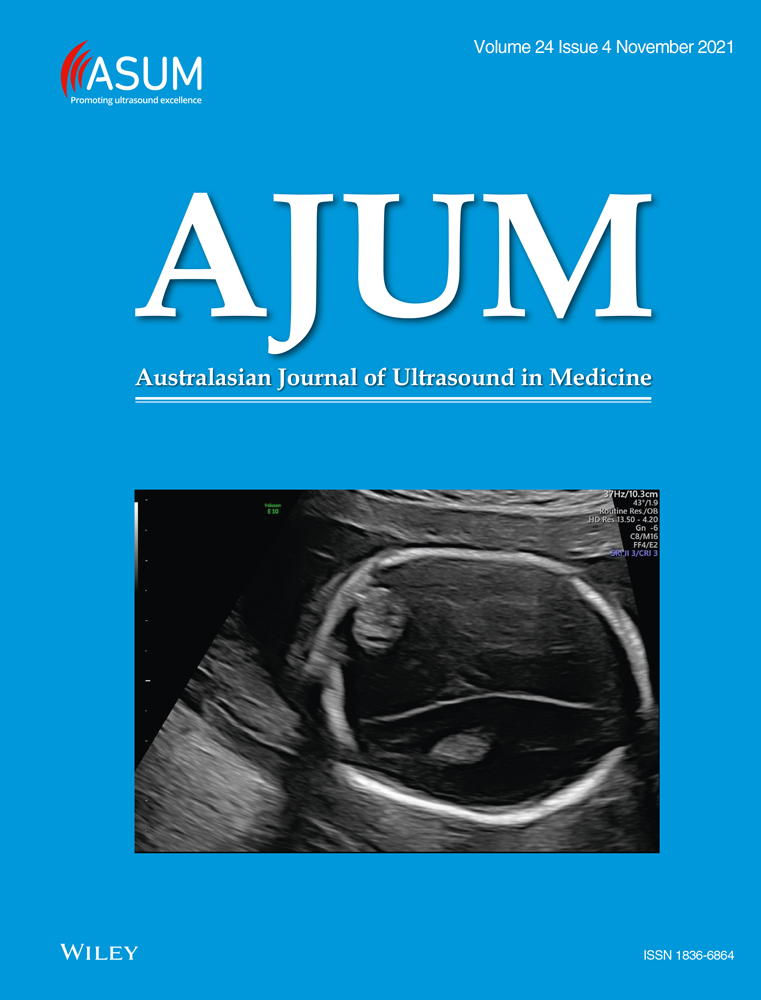
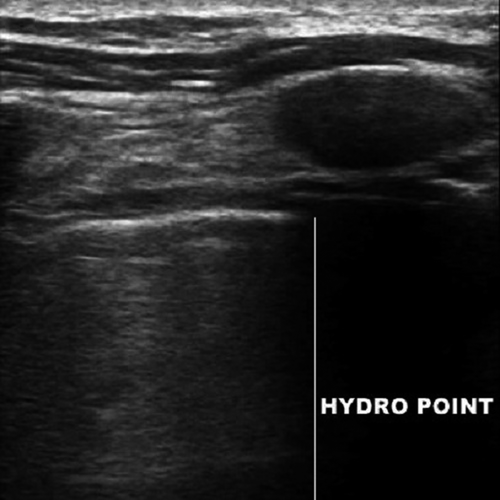
Point-of-care ultrasound findings – Point-of-care ultrasound (POCUS) in lung showed hydro-point, dynamic air–fluid interface (DAFI) sign (Video S1) and a characteristic triple sign, namely barcode sign/stratosphere sign (Figure 1), hydro-point (Figure 2) and sinusoidal pattern (Figure 3) in right lung. These features are seen in effusive pneumothorax, namely hydropneumothorax, hemopneumothorax and pyopneumothorax.1-3
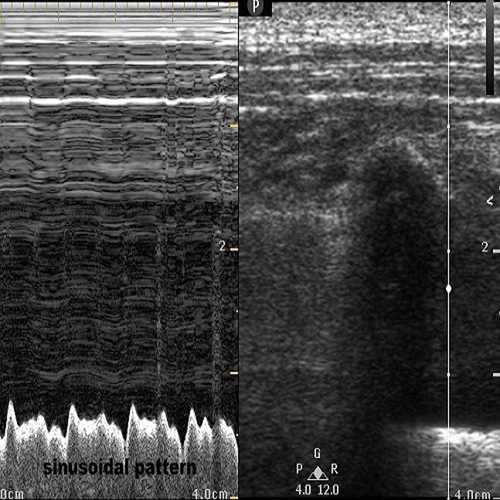
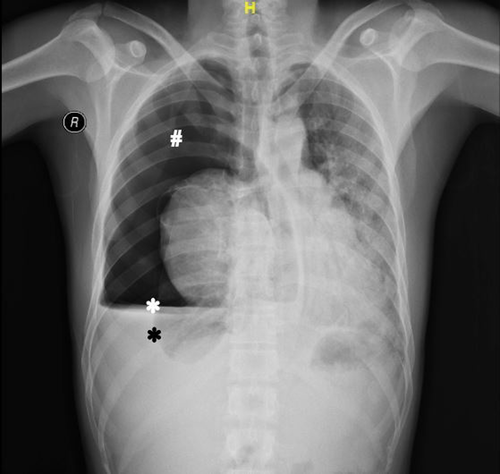
Chest X-ray findings – Chest X-ray showed air–fluid level, which confirmed effusive pneumothorax (Figure 4) as predicted by POCUS.
As a part of continued resuscitation, a right-sided intercostal tube drainage (ICD) was inserted, which had a gush of air and straw-coloured fluid confirming it as hydropneumothorax, followed by a CXR to check for tube position. The patient's saturation improved to 96% and was symptomatically better after ICD. Baseline workup showed raised white blood cell counts. Sputum acid-fast bacilli staining (AFB) was positive for mycobacterium tuberculosis. The patient's pleural fluid culture–sputum culture turned out to be positive for pseudomonas aeruginosa and klebsiella pneumoniae co-infection. Hence, we started the patient on category 1 antitubercular treatment (ATT) and antibiotics, namely amikacin and ciprofloxacin, based on the antibiotic sensitivity profile. The final diagnosis was tubercular hydropneumothorax with secondary bacterial infections. Bedside point-of-care ultrasound helped us rapidly assess and diagnose the underlying clinical condition, which helped us resuscitate this patient well in our emergency department.
Discussion
Bedside lung ultrasonographic assessment may sometimes simultaneously show pneumothorax signs in the non-dependent zone and pleural effusion signs in the dependent zone, which might hint towards hydropneumothorax. In such a patient to confirm hydropneumothorax at the bedside, the lung can be screened slowly in the caudocranial direction in sitting position from the effusion zone, and one can see hyperechoic–anechoic dynamic image subpleurally at the air–fluid interface level. This hyperechoic–anechoic interface and the hyperechoic–anechoic dynamic image are called hydro-point and DAFI sign. Thus, if such a pattern of barcode sign or absent lung sliding in the non-dependent zone, hydro-point at interface zone and pleural effusion/sinusoidal pattern in the dependent zone are seen, hydropneumothorax can be diagnosed at the bedside.
The DAFI sign, or hydro-point, is seen when the linear probe is kept at the air–fluid interface of effusive pneumothorax. Ultrasound in peripherally located larger lung abscess may also show hydro-point, which requires further ultrasonographic research studies. Severity assessment of effusive pneumothorax can be done by hydro-point location. If the hydro-point is located in anterior hemithorax in the supine position, effusion is more than pneumothorax, and if located in posterior hemithorax, pneumothorax is more than effusion. Few ultrasonographic caveats that one should keep in mind are a positional variation (supine or sitting) that can alter the triple sign from the anteroposterior to the craniocaudal direction, and the DAFI should not be mistaken for lung sliding.
The most common cause of hydropneumothorax in India is tuberculosis.4 Other causes can be necrotising bacterial pneumonia, obstructive lung disease, bronchopleural fistula, esophagopleural fistula, prior lung surgery, lung malignancy, iatrogenic causes, chest trauma, cystic lung disease, pulmonary infarction, post-partial pneumonectomy and rarely connective tissue disorders.5 The characteristic triple sign in effusive pneumothorax, namely ‘barcode–hydro-point–sinusoidal sign’, has not been sufficiently reported or discussed in the literature. The literature search also revealed only three case reports are there regarding hydro-point.1-3 Thus, we felt reporting this case would be a worthwhile addition to the literature.
Authorship statement
The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Funding
This article did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of interest
None declared.
Author Contributions
Sasikumar Mahalingam: Conceptualisation (lead); Resources (lead); Visualisation (lead); Writing-original draft (equal); Writing-review & editing (lead). Gunaseelan Ranjendran: Conceptualisation (equal); Writing-review & editing (equal). Balamurugan Nathan: Conceptualisation (equal); Writing-review & editing (equal). Ezhil Kugan: Writing-review & editing (equal). Anuusha Sadasivam: Writing-review & editing (equal).