Artificial intelligence and the impact on medical genetics
Abstract
Virtually all areas of biomedicine will be increasingly affected by applications of artificial intelligence (AI). We discuss how AI may affect fields of medical genetics, including both clinicians and laboratorians. In addition to reviewing the anticipated impact, we provide recommendations for ways in which these groups may want to evolve in light of the influence of AI. We also briefly discuss how educational and training programs can play a key role in preparing the future workforce given these anticipated changes.
1 INTRODUCTION
Artificial intelligence (AI) has already had a profound impact on medical genetics, though practitioner awareness of this impact may vary. Beyond many ongoing activities in the research arena and everyday clinical practices such as accessing data through search engines or using some voice-to-text systems, examples of current clinical uses of AI include discovery and translational insights of novel disease genes, clinical diagnostic genomic analysis of established disease genes with variant and gene prioritization based upon phenotypic matching, and dysmorphology assessment for clinical diagnosis (Hsieh et al., 2022; Jaganathan et al., 2019; Ledgister Hanchard et al., 2022; Poplin et al., 2018). It is also important to note that AI is not a monolith—many different methods are used in clinical genetics, sometimes in concert (Dias & Torkamani, 2019; Ledgister Hanchard et al., 2022).
The pace of AI development is accelerating, and the effects on clinical medicine will continue to expand and increase. Newer foundational AI models will be able to ingest, analyze, and generate diverse data types. As intuitive user interfaces are layered on top of these models, the geneticist of the future will operate in ways that are very different from today (Lee et al., 2023; Moor et al., 2023). In this piece, we briefly outline our predictions pertaining to the field of medical genetics. We will also offer recommendations for geneticists to help evolve to capitalize on new opportunities in what we feel is inevitable or at least highly probable change.
We divide the discussion into two areas based upon the persona: clinician geneticists and clinical laboratory-based geneticists. While there is overlap (and though many people work in both spheres), we anticipate that these areas will be affected differently. We intentionally do not subdivide these sections to separate individuals with different degrees or certifications (e.g., MD, PhD, NP, PA, CGC, RN, etc.), including because we feel that one effect of AI will be to flatten the field. That is, we refer to “clinician geneticist” as any clinician in the medical genetics field. “Clinical laboratory-based geneticist” refers to any clinically oriented individual in a clinical laboratory setting, such as a molecular geneticist, cytogeneticist, genome analyst, medical geneticist, or genetic counselor involved in some part of the genetic testing process. Though outside the scope of this commentary, we note that other staff working in these spaces will also eventually be affected by AI-driven automation. For example, robots that automate wet lab processes without leveraging AI are already used extensively in clinical laboratories, especially large, high-throughput facilities. Although the near-term changes engendered by AI will primarily affect analytic processes, it is likely that robots performing physical tasks will increasingly employ AI-based algorithms to optimize existing or automate new processes such as primer designs or capture sequences. Finally, though the larger biotech/pharmaceutical space will also be impacted by AI, partially driven by breakthroughs like AlphaFold (which will influence therapeutics as well as diagnostics, such as by improvements in medicinal chemistry), we do not delve into that area except to note here that the field of genetics has many direct and indirect connections with entities like pharmaceutical and biotechnology companies that will likely grow (Jumper et al., 2021).
We would like to emphasize that this piece is intentionally provocative. We recognize that many may disagree with some or all of our predictions, and we encourage discourse.
1.1 Clinician geneticists
Medical genetics has long been a diagnostically focused specialty, and the main goal has been to select specific tests to help understand the cause of a person's signs and symptoms. After establishing a diagnosis, or exhausting available testing, some geneticists would play a less central role in patient management.
We expect several converging issues—many of which relate to advances in AI—to affect the role of medical geneticists. First, clinical genetic/genomic testing is moving toward increasingly broad-based approaches, where it is less important to select the specific test beyond recognizing that exome or genome sequencing is indicated (in the future, these broad approaches may increasingly include additional modalities such as epigenomics) (Aradhya & Nussbaum, 2018; Manickam et al., 2021). Furthermore, AI-based decision support can help clinicians identify patients likely to have a genetic diagnosis earlier in the disease course (and should be able to do so more uniformly and equitably, though careful attention must be paid to this area to ensure that AI does not develop biases against groups such as underserved communities; Tekendo-Ngongang et al., 2020), and generate differential diagnoses, including decision support, to identify which patients might benefit from a specific test versus broad-based genomic sequencing (Hsieh et al., 2022). We anticipate that this type of AI guidance will expand and can be embedded in the electronic health record to scale to the large number of patients who can benefit from a genetic diagnosis and to serve patients in areas with insufficient access to geneticists. The most efficient and highest-performing genomic diagnostic methods are often undergirded by a suite of AI-based tools used to interpret the large numbers of genetic variants by analyzing both genomic and phenotypic data in concert (De La Vega et al., 2021; Dias & Torkamani, 2019; Hsieh et al., 2019).
Second, as genetics continues to “go mainstream,” and continues to be limited by the small numbers of geneticists relative to individuals with known or suspected genetic conditions, we expect that more non-geneticists (including more nonphysicians) will order genetic testing for individuals suspected to have genetic conditions (Jenkins et al., 2021). That is, many non-geneticists will be able to leverage genetic diagnostics so that a genetic pre-test consultation may be felt to be less important or unnecessary and may act as a barrier to patient care. As the cost of genetic testing declines and evidence-based guidelines clarify indications for which genetic tests are appropriate and as third-party payers cover genetic testing, we anticipate that geneticists will not need to gatekeep access to genetic testing.
Third, as the costs of genome sequencing (and related expenses, such as computational requirements) drop, and as AI tools allow efficient and large-scale analysis of sequencing data, the field may continue to move toward a genome-first approach (Biesecker et al., 2021; Wilczewski et al., 2023). In this scenario, it will be less important for clinical geneticists to determine who should undergo genetic testing than to help determine guidelines and practices and to manage patients once the diagnosis is made.
Thus, there is both a threat and opportunity for geneticists to evolve from focusing on diagnosis to focusing on management after diagnosis (Vockley et al., 2023). This will be supported by growing opportunities for precision medical care based upon molecular diagnosis (Katz et al., 2020), including new medical management strategies, and gene-targeted therapies such as gene modulation, gene addition, and gene editing.
Although these new precision therapies offer great promise, they will not be available quickly or universally, and the impact of AI on geneticists will not wait until these treatments are available. Furthermore, many “single-organ” genetic conditions will be primarily diagnosed and managed by nongenetic subspecialists, particularly as more therapies become available. For example, nephrologists will oversee the care of people with genetic nephropathies, cardiologists will care for individuals with genetic cardiomyopathies, and neurologists will manage people will genetic seizure disorders.
Geneticists will likely have a larger role to play in the care of individuals with complex, multi-system diseases (see Table 1 for a summary of recommendations pertaining to multiple areas discussed in this paper). This should optimally occur in conjunction with other subspecialists, but geneticists, with their deep understanding of the medical, familial, and social impacts of pleiotropic conditions, can coordinate care, ensure that appropriate surveillance is followed, and advocate for patients to receive necessary education and social services (Schaefer et al., 2016; Solomon et al., 2013). An illustrative example is biochemical geneticists, who coordinate the care of patients with inborn errors of metabolism. Their practices are different from those of other types of geneticists, and their ongoing clinical management is a model for how practices for other clinical geneticists should evolve.
| Clinical geneticists | Clinical laboratory-based geneticists | Genetics training programs | |
|---|---|---|---|
| Effects of AI |
|
|
|
| Recommendations and opportunities |
|
|
|
1.2 Clinical laboratory-based geneticists
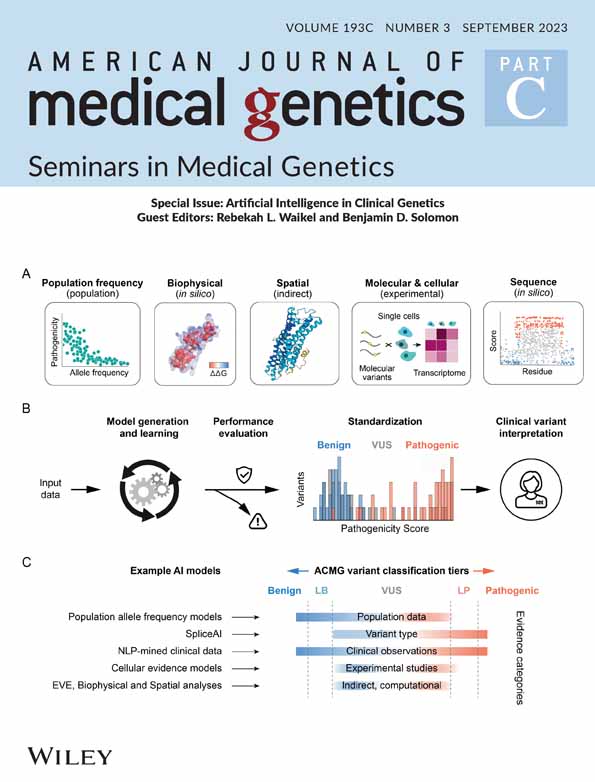
AI is likely to impact the genetic diagnostic laboratory more quickly and substantially than the genetics clinic. In the lab, AI-driven automation will yield faster and more accurate genomic diagnoses and report generation (De La Vega et al., 2021; Dias & Torkamani, 2019). Methods for variant and genome interpretation have been built and will be refined for many types of genomic tests, and may be especially valuable for genomic (and other ‘omic) data, as well as for cost-effective reanalysis of genomic data (Cristiano et al., 2019; O'Brien et al., 2022; Sundaram et al., 2018). In the not-too-distant future, the process of getting results from a genome will look much more similar to today's most frequently ordered genetic tests, such as noninvasive prenatal screening, where the majority of tests go through an automated workflow, with a minority of cases flagged for manual review (Bianchi & Chiu, 2018). In the laboratory setting, generative AI will also be able to perform other administrative tasks that would formerly fall at least partially under the purview of clinical laboratory-based geneticists. For example, large-language models (LLMs) will be used to provide information and explanations for insurance companies, populate testing websites, respond to pretest questions from clinicians and patients, and provide basic pretest genetic education (Lee et al., 2023). AI-based chatbots are already currently in use for customer service and pretest counseling in some genetic testing laboratories (Snir et al., 2021).
Overall, innovations in genomic analytics that are more automated and AI-driven will improve speed, accuracy, and cost-efficiency in existing labs as well as new labs that come into the market and compete, particularly as sequencing costs come down. This will help with the correlation of genotypic and phenotypic data, including improved ability to classify variants, especially for variants with conflicting data and variants of uncertain significance, which disproportionately impact individuals of non-European ancestry (Nykamp et al., 2017; Spielmann & Kircher, 2022) pil. The jobs of genetic analysts will be particularly vulnerable as their tasks are replaced by computational automation driven by ever-larger genomic and phenotypic data sets. This vulnerability may be tempered by several factors. First, the field of genetic/genomic diagnostics is still growing, especially as the costs of sequencing drop. More people now undergo clinical testing for a wider variety of indications than in the past, and this trend will likely continue. Thus, even if much of manual analysis and other human-centric work is replaced by AI and other forms of automation, the increasing volume of testing will mean that many edge cases will remain that require human resolution. The laboratory geneticist of the future—like the pathologist and radiologist—will work increasingly hand-in-hand with assistive AI tools but will still be a key part of the workflow (Farzaneh et al., 2023; He et al., 2023; Kann et al., 2023; Topol, 2019). Second, and related to the previous point, the availability of AI-based tools will continue to decrease the activation energy needed to order genetic testing. While regulatory burdens will (and should) remain in place to ensure the safety and accuracy of interpretation, AI may make it easier for new labs to enter the market or existing labs to expand their offerings. One possible outcome is that laboratories may be more viable in lower-resource settings around the world than was previously possible, enabling more equitable inclusion of a diverse group of patients. Clinical laboratory-based geneticists will continue to be critical to help establish labs and on-board new tests (see more on this point below). Finally, regulatory requirements will likely include the need for validation of new analytical methods with oversight from credentialed geneticists.
Despite some of these tempering effects, the long-term impact of AI on the laboratorian will be profound. There will still be positions for laboratorians, but they will likely be fewer and different in the future, both in terms of day-to-day activities and which entities employ laboratory geneticists.
In genetic testing laboratories, geneticists will spend less time analyzing individual genetic testing results. However, in the same laboratories, there will be opportunities for those with expert domain knowledge to work with bioinformaticians and computational staff to establish, curate, and annotate datasets to train AI tools, fine-tune methods, assess quality, train the workforce on new approaches, and develop and test generative models like LLMs. For example, in large laboratories, it may be useful to tailor publicly available AI models using a lab's internal, proprietary datasets. In the longer term, an individual laboratory's proprietary data will likely be replaced by robust datasets that are becoming increasingly publicly available, as off-the-shelf commercial pipelines obviate the need for home-grown bioinformatic solutions, and as unsupervised or automated training methods are employed (De La Vega et al., 2021). As we are seeing in fields like radiology and pathology, there may also be key roles for laboratorians in testing and implementing AI-based solutions (Hosny et al., 2018). Work in these fields has also shown that implementation efforts will be critical to ensure that AI processes are accurate and can fit into the clinical workflow (Kiani et al., 2020).
Clinical laboratory-based geneticists may also find that as the need for manual testing analysis in laboratories diminishes, and as commercial pipelines become even more standardized, there may be increasing demand for content experts at the companies that develop AI-based genetic testing algorithms. In addition to companies that focus on building genomic analysis algorithms, opportunities will arise in other settings where clinical laboratory-based geneticists work. Currently, many are employed in traditional genetic testing labs (of various types and sizes). There will be other opportunities to implement and grow genomic medicine, and clinical laboratory-based geneticists can fill critical niches. Experts will be needed to assist with integration of genomic data into EMRs, manage population-based genomic screening programs, and—critically—be involved in efforts to assure that AI-driven methods work equitably across diverse populations (Porras et al., 2021; Solomon et al., 2023; All of Us Research Program Investigators, 2019). Lastly, in the previous section, we discussed the advent of precision genomic therapies, which hold tremendous promise. Clinical laboratory-based geneticists may find opportunities in biotechnology/pharmaceutical companies that develop and test these treatments, as well as related regulatory agencies that oversee medical interventions for patients with genetic conditions.
1.3 Implications for education and training programs
To paraphrase Wayne Gretzky's statement that we need to skate to where the puck is going not where it is now, it is imperative that genetic training programs prepare trainees for the future, not the past (or even the present). This is easier said than done, especially as many aspects of future work in genetics are unpredictable. However, several themes related to AI are helpful to consider. First, it will be important for all types of geneticists to be trained in data science and understand the basis of AI-based tools. We are not advocating for all geneticists to become computer scientists—in fact, AI may threaten the job of computer programmers more than most professions. Still, geneticists should be able to understand nuances of how AI tools work, and the pros and cons of various methods, and should strive to be fluent in their uses. Second, related to the previous point, the content of education should shift from an emphasis on memorizing specifics about genes and genetic conditions to a more holistic approach that includes the overall care of individuals with complex, multisystem conditions. This will allow more time for working through subjects like computationally driven information retrieval, data management, and applications of patient-centric care. Third, one danger of AI involves algorithmic biases and other ethical dilemmas. Just as genetic training programs have wrestled with bioethical questions involving issues such as germline editing, prenatal testing, and secondary findings in genomic sequencing, training programs are uniquely poised to ensure that practitioners are well-informed about controversial areas in AI and genetics, understand the limits of AI (including how to recognize inaccurate or misleading results) and can work to ensure that the use of AI promotes equity. Finally, training programs should work to prepare geneticists for careers in more diverse settings than traditional clinics and genetics laboratories, including in roles involving the implementation of genomic medicine, diagnostics, clinical management, and areas of public policy and advocacy. Interestingly, AI is already having a dramatic effect in education, and training programs will have to face many issues to manage the repercussions. For example, trainees (and others) can quickly access coherent but potentially inaccurate information via AI-based tools (Duong & Solomon, 2023).
1.4 Conclusions
The speed at which recent AI methods are being developed and adopted is astonishing. The ultimate pace and scope of the effects of these developments are still unclear. Nevertheless, we expect that AI will cause the field of genetics to change rapidly. Although regulatory costs of testing and treatments may affect the pace of change, we also expect that this future will come soon. We urge our colleagues to think about what they want our field to become in the light of AI's effects, and to prepare for our future state.
While aspects of this piece may feel dystopian to some, we want to finish by emphasizing some very positive developments that AI could bring. AI may be able to assist with some of the most unpleasant tasks such as clinical documentation, billing, and gating by payors (Topol, 2019). In an ideal world, AI could free people to more directly help and interact with people affected by genetic conditions and could be a powerful tool to promote equity and inclusion. AI holds great promise, but there are also many risks. Geneticists can play important roles to ensure that AI has a net positive effect in our field.
ACKNOWLEDGMENTS
The authors would like to thank Anna Hurst, Shahida Moosa, and Kyle Retterer for their insightful reviews and comments. This work was supported in part by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. Benjamin D. Solomon is the co-Editor-in-Chief of the American Journal of Medical Genetics, parts A and C, and receives textbook publishing royalties from Wiley. Benjamin D. Solomon and Wendy K. Chung were formerly employees of commercial testing laboratories (BioReference and GeneDx). Wendy K. Chung is on the Board of Directors of Prime Medicine and RallyBio.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.