Inherited eye diseases in Turkey: Current approaches and future directions
Abstract
The aim of this review is to reveal Turkey's current status of medical practice in inherited eye diseases and the necessary steps to improve healthcare services and research activities in this area. Since consanguinity rate is high, disease burden is estimated to be high in Turkey. Universal health insurance system, easily accessible medical specialists, increasing genetic test, and counseling opportunities are the key advantages of Turkey's healthcare system. However, specialized clinics for inherited eye diseases, low-vision rehabilitation services, training of ophthalmologists about the recent developments in ocular genetics, and multidisciplinary translational research are the main headlines needed to be focused for better health services and successful research in Turkey.
1 INTRODUCTION
Turkey is a transcontinental country occupying a unique geographic position that has acted both as a barrier and a bridge between Asia and Europe throughout its history. The country with a population of approximately 83 million (TUIK, 2019) has been a center for migration routes and so population admixture (Ozçelik, 2017). In a study of the Greater Middle East, it was reported that the Turkish peninsula population was consistent with higher levels of European admixture and its genomic landscape was important for enhanced discovery of disease-associated genes (Scott et al., 2016). Besides, nearly one in five marriages in Turkey was consanguineous (Kaplan et al., 2016; Tuncbilek & Koc, 1994) that also contributes to a higher rate of births with congenital abnormalities and recessive Mendelian diseases (Ozçelik et al., 2010). Although we currently do not know the actual burden of inherited eye diseases in Turkey, those factors mentioned above should cause a higher number and variability of inherited eye diseases compared with Europe and the United States. This review aims to reveal Turkey's current status of practice and research in inherited eye diseases.
2 INHERITED EYE DISEASES IN TURKEY
2.1 Clues for disease burden
In Turkey, there has been a limited number of data that gives an idea about the inherited eye disease burden in the country. In a previous national study investigating the causes of childhood blindness in Turkey through a survey among schools for visually disabled, it was noted that retinopathy (28.1%) and congenital cataract (16.3%) were the leading causes and the parental consanguinity rate was 52.7% among disabled children in those schools (Turan, Recep, Abdik, Karaatlı, & Hasıripi, 2002). In this study, the number of inherited conditions was not defined clearly but it was reported that two thirds of retinopathy cases had a diagnosis of inherited eye diseases. A local study in Turkey investigating the etiology of childhood blindness in 148 patients who had visual impairment or blindness, it was reported that 25% of patients had been diagnosed with a genetic disease as the cause of visual impairment (Cetin, Yaman, & Berk, 2004). This group published another study revealing the changing trends over the last decade in the etiology of childhood blindness and reported that the incidence of genetic diseases was significantly decreased from 25% in 2002 to 19% in 2014 (Ozturk, Er, Yaman, & Tulin Berk, 2016). Besides those studies in children, there have been two published reports of the causes of blindness in the adult population who were admitted to hospitals for health reports: The first study was from the east of Turkey and the second one was from the west of Turkey. The first study reported that cataract was the leading cause of blindness in aged 64 years and over (Kivanc, Akova-Budak, Olcaysu, & Cevik, 2016). The second study reported that retinal dystrophies and congenital eye anomalies were the leading causes for the 18–50 years of age group (Koç, Erden, & Sefi-Yurdakul, 2018). The difference between the results of these two studies could be attributed to the age groups included and the difference in socioeconomic characteristics between two geographical regions. Despite the studies mentioned above, there is no nationwide report about the incidence of inherited eye diseases in Turkey. However, we have the knowledge of high consanguinity rates in Turkey (Kaplan et al., 2016) and published data showed that consanguinity was more likely to result in children with eye diseases with genetic etiology, especially autosomal recessive diseases (Bener & Mohammad, 2017; Kemmanu et al., 2019; Kumaramanickavel, Joseph, Vidhya, Arokiasamy, & Shetty, 2002). Therefore, we could estimate that inherited eye diseases had a major contribution to the visually impaired and blind patient population in Turkey.
2.2 Healthcare system, eye care services, and medical genetics in Turkey
Turkey has universal health insurance (UHI) system since 2012. With this system, there are no copayments for patients using the primary healthcare services and a small copayment at a fixed rate declared by the state for the patients visiting hospitals without a referral. Individuals with lower income than the defined amounts are also covered by the state (Atun et al., 2013). There is a centralized governance model including both public and private healthcare services. Despite a strong primary health care system served by family physicians and general practitioners, patients could choose to visit directly a medical specialist in public and private hospitals without any restrictions and with a minimal extra cost (Yardim & Uner, 2018). The lack of the obligatory referral system is one of the major differences between the healthcare systems of Turkey and most of the European countries (Sekercan et al., 2018). When we examined some of the general health statistics: The number of physicians in 2018 was 153,128 and the number of persons per physician was 536 (TUIK, 2018). The total expenditure on health per capita of Turkey in 2016 was 1,036 dollars that was 5.4% of GDP in recent years that is lower than the European Union (9.93) and the United States (17.07) (The World Bank, 2016). The life expectancy in Turkey was 75.75 years on average in 2016 that is similar to most European countries and the United States (Our World in Data, 2016).
In the case of private and public eye care services in Turkey, the UHI system has been valid for most of the services except some refractive and aesthetic procedures (SGK, 2013). The patient has the right to choose and visit directly the ophthalmologist without any referral. The medical and surgical healthcare services including prescriptions for refractive errors and rehabilitation could only be given by ophthalmology specialists who were trained for 4 years after medical school. There is no official ophthalmology subspecialty training in Turkey but the Turkish Ophthalmological Association (TOA) has sub-societies for retina, glaucoma, refractive surgery and cataract, neuro-ophthalmology, cornea and ocular surface, oculoplastic surgery, electrodiagnostic, low vision rehabilitation, and pediatric ophthalmology (TOA, 2020). There has been no subsociety or group focused on ocular genetics in Turkey. Therefore, patients with inherited eye diseases are evaluated by general ophthalmologists and/or specialists in the cornea, glaucoma, retina, and pediatric ophthalmology units of hospitals.
The Medical Genetics specialists provide healthcare services for the inherited conditions in Turkey. Medical Genetics specialization is given to medical doctors after 4 years of training in Medical Genetics Departments of university hospitals. After completing this training, they become competent for genetic counseling, the services in the medical genetics' clinics, cytogenetics, and molecular genetics' laboratories. Medical Genetics experts provide services to the patients in Genetic Diseases Consultancy Centers, which are licensed by the Ministry of Health. In Turkey, there are over 200 licensed Genetic Diseases Counseling Centers in university hospitals, public hospitals, private genetic diagnostic centers and currently, about 200 specialists are working in them (Turkish Medical Genetics Association, 2020). Regarding these centers; dysmorphic patient examination and genetic counseling are being held in clinics; prenatal, postnatal, and cancer services are provided in the cytogenetic laboratories; genetic testing of single-gene disorders, rare diseases, hereditary cancers, whole exome analysis, liquid biopsy, noninvasive prenatal genetic diagnosis, preimplantation genetic screening, and diagnosis are provided in molecular genetics laboratories. The most common genetic tests invoiced to the Social Security System of Turkey from these centers consist of the next-generation sequencing analyses, FMF, and thrombophilia tests (Official Gazette of the Republic of Turkey, 2018). Fortunately, all these tests when ordered by a medical genetic specialist are covered by the state (Atun et al., 2013).
2.3 Approach to the inherited eye diseases in clinics
Patients with an inherited eye disease need comprehensive evaluation for clinic and genetic diagnosis, follow-up, treatment and/or rehabilitation, genetic counseling, social, and financial counseling. In Turkey, there is no specialized ocular genetics center providing this comprehensive service for inherited eye diseases. Therefore, patients could apply to ophthalmology clinics of public and private hospitals or private medical offices of ophthalmologists. However, the detailed examination including imaging, electrophysiological testing is applied in university hospitals or training and research hospitals or large private hospitals in big cities. In most of these centers, there are specialized units for pediatric ophthalmology, retina, cornea and anterior segment, glaucoma, and oculoplastic surgery. According to the disease, patients are directed to these units, and the process of evaluation continues there. If the patient has a systemic condition besides the eye problem, the ophthalmologists counsel them to the related departments in the same hospital. After the clinical diagnosis of an inherited eye disease there exist three options: (a) Follow-up and management without any genetic diagnosis, (b) referral to the medical genetics department of the same hospital for genetic testing and counseling, and (c) directing patients to private genetic diagnostic centers for genetic testing at their own expense. Until recently, the preferred option was the first one. However, as the genetic testing opportunities became cheaper, more widely distributed and the patients became more informed, the second and the third option have been preferred more often by ophthalmologists. Currently, the clinical and genetic testing opportunities are advanced in Turkey. However, there have still been challenges related to health services for inherited eye diseases. Firstly, the services are often provided in scattered locations in the same hospital and sometimes not even in the same hospital, which is a great handicap for patients and their families. Secondly, there are no established algorithms, standardized approaches, or training for inherited eye diseases supported by the ophthalmological association in Turkey. Thirdly, the clinics are too crowded which results in shorter visit periods and less detailed examination of patients and their families. Lastly, there are few low vision rehabilitation centers in Turkey compared with the visually disabled population (Altınbay & İdil, 2019).
2.4 Genetic testing and genetic counseling for inherited eye diseases
Until the last 2 years, the referral of patients for genetic testing in ophthalmology was mostly restricted to the research or the thesis studies of the residents in ophthalmology or medical genetic departments (Kepez Yildiz et al., 2016; Kramer et al., 2019). Since 2019, the referral of patients from the ophthalmology clinics to the Medical Genetics Department or private genetic diagnostic centers for clinical genetic testing or genetic counseling has started to increase as mentioned in the previous section.
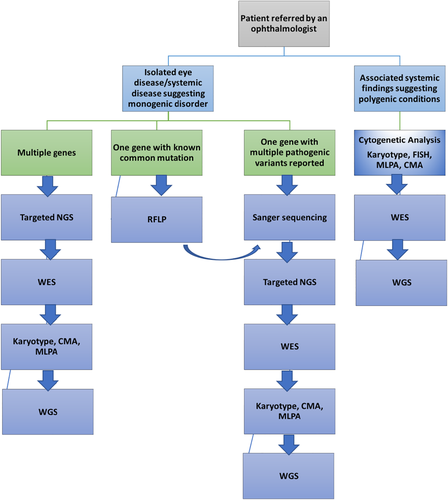
According to the standardized procedures in Medical Genetics Departments, detailed anamnesis is obtained, and the pedigree analysis is performed after the referral of the patient from ophthalmology clinics. The genetic tests can be administered to the patients depending on the disease whether it is sporadic or familial; isolated or part of a syndrome; single gene disorder or due to a chromosomal abnormality. Regarding chromosomal abnormalities that result in eye findings such as velocardiofacial syndrome (VCFS), karyotyping, fluorescent in situ hybridization (FISH), multiplex ligation-dependent probe amplification (MLPA), and chromosomal Microarray (CMA) can be performed to detect submicroscopic changes. If the disease occurs due to a single gene mutation, such as macular corneal dystrophy caused by mutations in CHST6 gene, Sanger sequencing is sufficient to find the pathogenic variant. Additionally, restriction fragment length polymorphisms (RFLP) could also be used if the disease is characterized by a single mutation in a single gene such as autosomal dominant Basal Laminar Drusen disease characterized by the most common Y402H mutation in the CFH gene. However, these genetic testing methods could be used rarely due to genetic heterogeneity in most of the inherited eye diseases. Regarding the genetic heterogeneity in ophthalmic diseases, next-generation sequencing (NGS) technology provides the most favorite methods to find the responsible gene for multigenic diseases. NGS includes high-throughput sequencing techniques which allow the analysis of many genes in parallel (Gillespie, Hall, & Black, 2014). Multigene testing or panel testing should be the first choice in eye diseases characterized by multiple mutations in multiple genes (Tsang & Sharma, 2018). If nothing can be found with targeted sequencing, whole-exome sequencing (WES) which provides more data should be chosen. WES allows sequencing of the whole coding region of DNA that is thought to contain the majority of disease-causing mutations (Choi et al., 2009). The next option could be the whole-genome sequencing (WGS) that sequences the entire genome, both coding and noncoding DNA. It provides a huge amount of variant information that needs further evaluation, therefore WGS is often used for research purposes (Tsang & Sharma, 2018). With NGS, a new mutation in the known gene or a “novel” gene that can cause disease can be identified. The variants detected in NGS tests are evaluated by medical geneticists according to the recommendations of the American College of Medical Genetics and Genomics (ACGM) via searching the literature, certain datasets, and via using computational analysis (Richards, Aziz, Bale, et al., 2015). The pathogenic, likely pathogenic variants and variants of unknown significance related to the clinical diagnosis are included in the reports. Also, confirmation of the results with Sanger sequencing is necessary in the patient and if possible, in the available family members before preparation of the genetic test reports.
In Figure 1, the algorithm, used in the Medical Genetics Department of Gazi University Hospital collaborating with one of the biggest reference ophthalmology clinics in Turkey, was shown. To summarize this algorithm, the first step is to obtain detailed anamnesis and to make a pedigree analysis. If the clinical diagnosis suggests a monogenic disorder, the testing strategy depends on the genetic heterogeneity of the clinical diagnosis. If the clinical diagnosis suggests a polygenic disorder with dysmorphic findings, retardation and/or other systemic findings, the first step is to rule out chromosomal abnormalities, submicroscopic deletions, or duplications through karyotype, FISH, MLPA, and CMA. As further steps in both conditions, NGS tests are being used. If the targeted NGS panel or WES could not give a result, WGS is the last testing option. When the causative mutation is found, this mutation is confirmed by Sanger sequencing in the patient and the segregation is tested if possible, in the family as a last step. Genetic counseling is performed before and after the genetic tests by the medical geneticist in the clinics. Also, the consent form has to be taken from individuals or family members for ethical reasons. Since 2019, there have been 57 probands who were referred from the Ophthalmology Department of Gazi University Hospital. The clinical diagnoses in those patients were retinitis pigmentosa (28.1%), Stargardt disease (12.3%), cone-rod dystrophies (10.5%), corneal dystrophy (10.5%), congenital cataract (17.5%), and congenital glaucoma (7%), others including syndromes, microphthalmia, familial strabismus, Malattie Levantinese, etc. Systemic findings were found in 13% of the patients. The genetic diagnosis was provided in 82.4% of patients. In 10 patients, no pathogenic or likely pathogenic variants were detected in WES and directed for WGS as part of a research project.
2.5 Management of inherited eye diseases
In Turkey, when a patient receives a clinical and/or genetic diagnosis of an inherited eye disease, the management steps include: (a) Follow-up without any intervention; (b) appropriate routine medical and surgical therapies; (c) referral to the clinical trials conducted in Turkey; and (d) low vision rehabilitation.
Follow-up without any intervention could be an option for advanced retinal dystrophies, hereditary optic neuropathies. However, this option has been offered less due to emerging novel therapies, rehabilitation methods, and information networks used by patients and their families.
Routine medical and surgical therapies could be offered in many hospitals nationwide including spectacle prescription, topical medications, cataract surgery, refractive surgery, vitrectomy, strabismus surgery, intravitreal injections, etc., whenever indicated for the patient with inherited eye disease.
In the case of clinical trials conducted in Turkey, there have been studies including stem cell therapy, retinal prosthesis, and platelet-rich plasma (PRP) and/or electrical stimulation. Dr. Ayse Oner and her colleagues have conducted clinical studies of stem cell therapy in retinitis pigmentosa (RP) and Stargardts' macular dystrophy (SMD) at Erciyes University, Kayseri. Their study group published the results of the subretinal adipose-tissue derived mesenchymal stem cell implantation in advanced stage retinitis pigmentosa (Oner et al., 2019a; Oner, Gonen, Sevim, Sinim, & Unlu, 2019b; Oner, Gönen, Sinim, Çetin, & Özkul, 2016). With the subretinal delivery method, complications requiring second surgeries occurred during follow-ups such as epiretinal membrane formation at the implantation site and peripheral tractional detachment. Therefore, the subretinal delivery technique was abandoned and was replaced with the suprachoroidal delivery method which did not cause any complication other than a subconjunctival hemorrhage. The suprachoroidal delivery method being near the choroid also had the advantage of allowing the produced growth factors (GF) to enter the choroidal flow and reaching the endothelial cell receptors and eventually reaching to and interacting with retinal pigment epithelium cells (RPEs), Muller cells, and photoreceptors and managing to constant GF secretion in the choroidal flow (Oner, Gonen, Sevim, Sinim, & Unlu, 2018). The continuous improvement in this study through a 1-year follow-up could relate to this phenomenon. The choroidal thickening in the set of study patients could be the reflectance of an increase in choroidal perfusion compatible with previous study results (Oner et al., 2018; Oner, Gonen, Sevim, Sinim, Cetin, & Ozkul, 2019a; Oner, Gonen, Sevim, Sinim, & Unlu, 2019b). Their group also used umbilical cord-derived MSCs (UC-MSCs) as a stem cell source. UC-MSCs have advantages like higher proliferation potential, a larger portion of mesenchymal progenitor cells, more stable doubling time, faster self-renewal ability, lower immunogenicity, and more primitive than other adult tissue derived MSCs. They may release GFs, mediators, and have immunomodulatory effects. These released factors can slow the apoptotic process, promoting angiogenesis, preventing inflammation, and creating a microenvironment for cell survival (Hsieh et al., 2013). The collection of these cells is noninvasive, and patients could be protected against infection. It is an easy and more suitable process compared with MSCs from other sources such as bone marrow and adipose tissue. In a recent study of this group which included the largest number of patients in the literature 124 eyes of 82 RP patients received 5 million UC-MSCs to the suprachoroidal area with a surgical procedure and followed-up for 6-months. The median age was 38.5 years (range between 34 and 46 years). There were statistically significant improvements in best-corrected visual acuity (BCVA) and visual field (VF) results during the 6-month follow-up (p < .05 and p < .05 respectively). The evaluation of BCVA results individually showed that 57 eyes (46%) experienced an improvement in vision, 52 eyes (42%) remained stable, and 15 eyes (12%) worsened during the follow-up period. There were no serious ocular adverse events during the 6-month follow-up period (in press). In another study of this group including 16 eyes of 12 SMD patients received suprachoroidal UC -MSC implantation and followed-up for 6 months. Twelve eyes (75%) showed improvements in visual acuity, VF, and multifocal electroretinography (mfERG) tests, 1 eye (6.25%) remained stable and 3 eyes (18.75%) worsened during the study period. None of them experienced any systemic or ocular complications (in press).
Another group conducting clinical trials in retinal dystrophies is Dr. Ozmert's team from Ankara University. This group conducted clinical trials involving subtenon injection of PRP and/or electrical stimulation in patients with retinitis pigmentosa. Subtenon region of the eye acts as a natural cell culture medium for GFs and stem cells by peribulbar administration. Autologous platelet-rich plasma (aPRP) is a good source of GFs. Platelets have more than 30 GFs and cytokines in alpha-granules. GFs perform their activity by binding to the tyrosine kinase receptors, which are commonly found around the limbus, extraocular muscle insertions, and optic nerve. In the earlier clinical study conducted by Özmert et al., only aPRP was injected into subtenon space as a source of GFs. Effects of aPRP on the visual functions in eyes with RP was investigated in 71 eyes of 48 RP patients, and compared with the autologous platelet-poor plasma as a control to exclude the mechanical effects of the subtenon injections (Arslan, Özmert, Demirel, Örnek, & Şermet, 2018). Injections were made three times with 3-week intervals between each injection. The results of this study were encouraging as they showed that the subtenon injection of aPRP had a favorable effect on the visual field, mfERG, and microperimetry results. There were no serious adverse events or any ophthalmic or systemic side effects during the 1 year follow-up. Molecules smaller than 75 kDa can passively move from the sclera to the suprachoroidal space. Electrical or electromagnetic stimulation (Magnovizion Bioretina Biotechnology, Ankara, Turkey) is required for molecules larger than 75 kDa to pass through the sclera into the subretinal space. Also, electromagnetic stimulation (EMS) increases binding affinity and the synthesis of GF receptors on neural tissues. It also provides electromagnetic iontophoresis by changing the electrical charges of scleral pores and tyrosine kinase receptors. One-year results of 60 patients with RP were analyzed retrospectively by Ozmert et al. Patients constituted three groups: combined management group (40 eyes) who received combined retinal EMS and subtenon aPRP injections, the subtenon PRP-only group (40 eyes), and the natural course (control) group (20 patients with RP). Subtenon aPRP might more effectively slow down photoreceptor loss when repeated as booster injections with 4–6 months interval and combined with retinal EMS (Arslan & Özmert, 2020). Therefore, PRP is a good and noninvasive source of GFs, but its efficiency lasts for 4–6 months and requires booster injections to maintain the effect. Additionally, Ozmert's group conducted stem cell clinical trial in RP patients. Umbilical cord Wharton's jelly-derived mesenchymal stem cells (WJ-MSCs) have significant paracrine and immunomodulatory properties, were shown to secrete trophic factors that stimulate RPE or that are similar to those produced by RPE (Millán-Rivero, Nicolás, Bernal, et al., 2018; Wysocka, Kot, Sułkowski, Badyra, & Majka, 2019). In animal models, they were found to be effective in halting the progression of retinal degeneration (Zhang et al., 2017). Also, they can proliferate almost 300 times without karyotype changes (Canto-Soler, Flores-Bellver, & Vergara, 2016). This means that the paracrine-trophic effects of WJ-MSCs may last for 3–7 years in the tissue. This is why, another prospective, open-label, phase-3 clinical study conducted by Dr. Ozmert and his colleagues at Ankara University (Ozmert & Arslan, 2020). Umbilical cord WJ-MSCs were transplanted into the subtenon space using two distinct methods in 32 RP patients (34 eyes). WJ-MSCs were found to be effective in stopping the progression of retinal degeneration and rescuing photoreceptors in the dormant phase. Regardless of the type of genetic mutation, its administration appeared to be an effective and safe option. There were no serious adverse events or ophthalmic/systemic side effects for 6-months follow-up. As an extraocular approach, subtenon implantation of the stem cells with trophic paracrine effect seems to be a reasonable way to avoid the devastating side effect of intravitreal/subretinal injection. The first-year results of this clinical trial also revealed similar sustainable benefits with no adverse events (in press). Besides the therapeutic approaches mentioned above, various artificial vision research has been performed in the world (Chuang, Margo, & Greenberg, 2014). Özmert's group conducted the Argus II retinal prosthesis clinical studies in Turkey. For this purpose, fitting and rehabilitation laboratories, simulated living facilities for the rehabilitation studies, simulation laboratory for the training of international surgeons were established at the “Artificial Vision & Bionic Eye Department” of Ankara University. The endoscopic assistance in Argus II epiretinal prosthesis implantation in two advanced RP cases was reported for the first time in literature by Ozmert's group. The endoscopic assistance was used to prevent or lessen serious surgical complications such as retinal tear/detachment, choroidal detachment, and serious hypotony (Ozmert & Demirel, 2016). Clinical trials on the Argus II epiretinal prosthesis performed to date have shown the long-term safety and potential benefits in patients with advanced visual impairment due to outer retinal degeneration associated with conditions such as RP, choroideremia (Rizzo et al., 2018; Rizzo et al., 2020a; Rizzo et al., 2020b).
The number of clinical trials in inherited eye diseases should increase through more funding, governmental support, and multidisciplinary approach in Turkey. Additionally, networking should be widened between Turkish ophthalmologists to increase patient referral to these trials.
For inherited retinal diseases the last and the most important management step is the rehabilitation due to limited treatment options in several of them. Low vision rehabilitation enables patients to use their residual vision as effectively and efficiently as possible. In Turkey, The Vision Research and Low Vision Rehabilitation Center of Ankara University is the first and the only center providing comprehensive low vision rehabilitation to patients. This center provides low vision rehabilitation via field expansion prisms, microperimetry, telescopic glasses, telescopic intraocular lenses, telescopic contact lenses, and electro-optic systems. There are also Argus rehabilitation rooms for patients who underwent Argus II retinal prosthesis surgery, a library for patients, different living spaces for practice (Altınbay & İdil, 2019). Apart from this center, some of the rehabilitation services could be offered by ophthalmologists trained in this center and working in other hospitals (IBAYDER, 2020). However, in Turkey, the number is still low, and these services should disseminate throughout the country in order to meet the needs of patients with low vision.
2.6 Research in inherited eye diseases
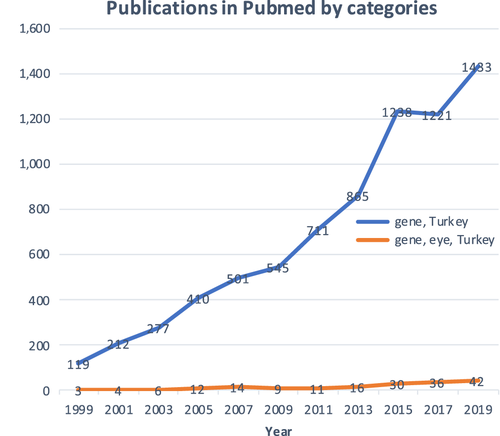
A search in PubMed using the keywords “gene, Turkey” showed that gene-related publications in Turkey have been growing in the last two decades (Figure 2). The keywords could not definitely display all publications however, the results could enable us to understand trends and make comparisons between groups. The number of publications about eye and gene in Turkey is relatively small as compared with the developed countries but it has also been growing throughout the years. When we compared the number of publications by changing the country name among the keywords including ocular genetics; retinitis pigmentosa and gene; eye and gene, the number of publications at least three times higher in Italy and 20 times higher in the United States. When we used the keyword retinitis pigmentosa only instead of retinitis pigmentosa and gene, the gap between Turkey and other countries becomes smaller (Table 1). Among the publications in recent years, there are clinical studies in patients about stem cell therapy, retinal prosthesis application, PRP treatments. Besides, there has been no previous or ongoing study about gene therapy or genome editing therapy in inherited eye diseases. As mentioned previously, there have been few studies about the epidemiology of inherited eye diseases, their social, and economic burden in the country. The number of animal studies investigating mechanisms of inherited eye disorders was also limited (Yaylacioglu Tuncay & Dincer, 2019). There have been relatively fewer studies investigating the genotype–phenotype correlations in inherited eye diseases from Turkey (Bardak et al., 2016; Ergun, Akay, Ergun, & Perçin, 2017; Karti et al., 2017; Semerci et al., 2014; Yaylacioglu Tuncay et al., 2016), and the most of these publications were accomplished by international collaborations (Bagiyeva et al., 2007; Elcioglu et al., 2007; Holt et al., 2017; Ozgul et al., 2004; Yamada et al., 2004) or by including Turkish patients living abroad (Angius et al., 2018; Iftikhar et al., 2019; Pach, Kohl, Gekeler, & Zobor, 2013). The dataset should grow about the genotypes of patients living in Turkey. Firstly, this is important to reveal founder alleles in diseases which are expected to be common in several types of inherited eye diseases due to consanguinity rates in the country. Secondly, this will be important to develop genetic testing methods or algorithms more cost-effective and applicable. Thirdly, novel variants or novel genotype–phenotype correlations in such a rich patient population could help researchers in revealing disease mechanisms and developing therapeutics. In this sense, the Turkish Genome Project has started recently with the aim of comprehensive genomic analysis of patients with cancer, complex and rare diseases (TUSEB, 2019). Inherited eye diseases are included in this project which will speed up the developing population-specific genomic dataset. The research potential of Turkey in hereditary eye diseases is high considering the variability and large patient population. Increasing the research capacity in the field needs higher financial support, more and efficient national and international networking, and collaboration between ophthalmologists and basic science researchers.
| Keywords | Ocular genetics | Retinitis pigmentosa | Retinitis pigmentosa, gene | Eye, gene |
|---|---|---|---|---|
| Turkey | 223 | 137 | 37 | 329 |
| Italy | 708 | 448 | 170 | 1,338 |
| The United States | 4,585 | 2,323 | 1,246 | 15,346 |
3 CONCLUSION
In this article, we summarized the current clinical and genetic approach to inherited eye diseases in Turkey. To increase the quality of healthcare services, to implement the increasing genetic knowledge into clinical practice, to provide the recent treatment and rehabilitation options for our patients, to increase high impact research activities in this field, Turkey should define a roadmap and apply this step by step. The roadmap will develop through collaboration between physicians from different disciplines, researchers, social workers, opticians, and patients, through observing the organizations in developed countries and through the support of the government. The first step in the roadmap might be a national registry system for inherited eye diseases. This is very important to know the disease burden exactly and manage the other steps accordingly. The second step might be establishing dedicated centers, namely ocular genetic centers, in large hospitals to provide comprehensive healthcare services uniting ophthalmologists, medical geneticists, opticians, and social workers in one location for patients. The third step may be the training of ophthalmologists with a fellowship program of ocular genetics or at least providing training options informing physicians about advancements and current approaches in inherited eye diseases. Fourth step may be the development of standardized algorithms for inherited eye diseases by the TOA to help general ophthalmologists for appropriate and standardized patient management and referral. The last step might be encouraging researchers, ophthalmologists, and funding agencies to increase the number of high-quality researches that would make important contributions to science and patients from Turkey.