No association of alcohol dependence with HOMER 1 and 2 genetic variants†
How to Cite this Article: Preuss UW, Ridinger M, Rujescu D, Fehr C, Koller G, Wodarz N, Bondy B, Soyka M, Wong WM, Zill P. 2010. No Association of Alcohol Dependence With HOMER 1 and 2 Genetic Variants. Am J Med Genet Part B 153B:1102–1109.
Abstract
Several lines of evidence indicate that alterations of the central cortico-accumbens glutamate pathway are involved in the development and maintenance of alcohol- and substance-use disorders. The HOMER protein family is encoded by 3 genes HOMER (1–3) which are components of the excitatory postsynaptic density complex and function to modulate synaptic activity by the regulation of glutamate signaling. HOMER 1 and 2 have been reported to contribute to chronic alcohol-induced long-term neurochemical changes in the endogenous reward system. Data from animal models suggest a potential role of the Homer protein family in the development of alcohol and substance use. The aim of this study is to assess potential associations between HOMER 1 and 2 genetic variants in a larger sample of alcohol-dependent individuals and unrelated controls. Five genetic variants of HOMER 1 and 3 of HOMER 2 were genotyped in a multi-site sample of 1,923 German healthy controls and 2,039 alcohol-dependent subjects. Neither single SNP nor haplotype analysis could detect significant associations with alcohol dependence (AD) and related phenotypes. While most of the HOMER 1 and 2 SNPs are in low-to-moderate linkage disequilibrium, three major haplotypes of HOMER 1 and 4 haplotypes of HOMER 2 are present in the majority of alcohol-dependent and control subjects. In conclusion, our results suggest that single SNPs, respectively, haplotypes of the HOMER 1 and 2 genes are unlikely to play a major role in the pathophysiology of AD. © 2010 Wiley-Liss, Inc.
Several lines of evidence indicate that the integrity of the cortico-accumbens glutamate pathway is required for expressing many alcohol- and other drug-induced changes in behavior, including the sensitization of a drug's psychomotor-activating effects [Bowers et al., 2004; Szumlinski et al., 2006] the development of tolerance to a drug's psychomotor-inhibiting effects [Szumlinski et al., 2006; 2008], drug-conditioned place-preference in animal models [e.g., Zavala et al., 2003; Williams and Steketee, 2004], the maintenance of drug self-administration [e.g., Spanagel and Heilig, 2005; Sudakov et al., 2006], and the reinstatement of drug-seeking [Baker et al., 2003; Backstrom et al., 2004].
While one of the best characterized actions of ethanol is modulation of glutamatergic transmission, ethanol exposure, and withdrawal leads to an increase in extracellular levels of glutamate in the N. accumbens and modulates glutamate receptor function, including NMDA receptors [e.g., Szumlinski et al., 2008].
One class of proteins involved in glutamatergic signaling that may play an important role in regulating the activity of this neurochemical pathway in response to alcohol and other substances is the HOMER protein family. The Homer family consists of three structurally related scaffolding proteins encoded by three distinct genes, HOMER 1–3 [de Bartolomeis and Iasevoli, 2003; Szumlinski et al., 2008].
The products of the HOMER genes are components of the excitatory postsynaptic density complex and function to modulate synaptic activity by the regulation of both calcium and glutamate signaling [de Bartolomeis and Iasevoli, 2003; Kalivas, 2004].
Constitutively expressed Homer proteins interact postsynaptically, via an EVH1-binding domain, with the glutamatergic C-terminus of Group 1 metabotropic receptors (mGluRs), the inositol triphosphate, and ryanodine receptors, as well as the NMDA receptor scaffolding protein Shank [for reviews, see Xiao et al., 2000; de Bartolomeis and Iasevoli, 2003].
Furthermore, HOMER 2 KO mice exhibit an alcohol-avoiding phenotype when assessed in a two bottle-choice procedure (0 vs. 3, 6, or 12% alcohol, v/v) and an alcohol-induced place-conditioning paradigm (8 g/kg × 0–3 g/kg) and HOMER 2 deletion also prevents alcohol-induced neurochemical plasticity in a brain region implicated in the rewarding/reinforcing effects of alcohol [Szumlinski et al., 2005]. These results indicate that expression of HOMER 2 may significantly contribute to long-term neurochemical changes in chronic alcohol exposure and other drugs of abuse, including cocaine, amphetamines, and opiates [review by Szumlinski et al., 2008].
All three Homer isoforms are expressed within several regions of the hippocampus and N. accumbens Ary and Szumlinski 2007; Szumlinski et al., 2008, but also in the dorsal and ventral aspects of the striatum [Xiao et al., 1998; Shin et al., 2003], the amygdala [Ary et al., 2007], the cerebellum [Shiraishi et al., 2004], but only HOMER 1 and 2 receptor isoforms have been localized within the thalamus [Xiao et al., 1998].
A previous study investigated the relationship between several genetic variants of HOMER 1 and HOMER 2 located on chromosomes 5q14.2 and 15q24.3, respectively, with cocaine dependence [Dahl et al., 2005], and reported a significant association of the HOMER 1 SNP rs6871510 genotypes with cocaine dependence, while no association was detected between HOMER 2 variants.
To our knowledge, no previous study was conducted on any association of HOMER 1 and 2 SNPs and haplotypes with alcohol dependence (AD).
The aim of this case–control association study is to investigate the role of HOMER 1 and 2 gene variants in AD. Five SNPs in HOMER 1 and 3 SNPs in HOMER 2 genes in a larger, German multi-site sample of clinically well-characterized alcohol-dependent individuals and healthy control subjects were genotyped.
In addition, linkage disequilibrium (LD) measurement among the HOMER 1 and 2 polymorphisms and haplotype analyses (5 SNP haplotype for HOMER 1 and 3 SNP for HOMER 2) were conducted.
The first group of control individuals were recruited from the general population at different locations (e.g., libraries, road construction sites, department stores) and represent a range of social classes from unskilled workers to university graduates (n = 442).
A comprehensive medical and psychiatric assessment including the semi-structured assessment on genetics in alcoholism [SSAGA; Bucholz et al., 1994; Hesselbrock et al., 1999], as well as various personality questionnaires and a brief structured clinical interview with a psychiatrist was carried out in all control individuals together with routine laboratory screening to assess general dimensional personality characteristics and to exclude possible psychiatric axis I/II disorders, such as schizophrenia, depression, personality disorders, and substance-use disorders including AD. Furthermore, all individuals with any first-degree relative with a history of any axis I disorders (including AD) were excluded. This control sample has been described in more detail previously [Zill et al., 2004a,b].
A second group of controls (n = 1396) were unrelated volunteers of German descent, which were randomly selected from the general population of Munich, Germany, and contacted by mail. To include only subjects without a personal or family history of neuropsychiatric disorders, a screening was performed before enrolment in the study. First, subjects who responded (approximately 50%) were initially screened by phone. Detailed medical and psychiatric histories were assessed for both themselves and their first-degree relatives by using systematic forms. Second, they were invited to a comprehensive interview [SCID-I and SCID-II, German Versions, Fydrich et al., 1997; Wittchen et al., 1997].
Psychiatric diagnoses among their first-degree relatives were assessed using the Family History Assessment Module [Rice et al., 1995]. Subjects with relevant somatic diseases or a lifetime history of any axis I or II psychiatric disorders or suicidal behavior were excluded. Subjects who had first-degree relatives with a lifetime history of a mental disorder or suicidal behavior were also excluded.
The third group of controls from the University of Mainz were contacted by board notices at the Universities (n = 85). The absence of a psychiatric disorder was confirmed by a detailed psychiatric investigation in addition to a standardized diagnostic interview [CIDI/DIA-X, Composite International Diagnostic Interview, Wittchen and Pfister, 2004].
All alcohol-dependent subjects were recruited as inpatients from three addiction treatment wards (“qualified detoxification”) of the psychiatric hospitals Ludwig-Maximilians-University of Munich (n = 450), Gutenberg University of Mainz (n = 250), and University of Regensburg (n = 1,339). All alcohol-dependent subjects (n = 2,039) were treatment-seeking and admitted through an outpatient motivational group (Munich), an addiction outpatient unit (Regensburg) or for emergency detoxification (Mainz). While the mode of admission is different across hospitals, all three centers offer a “qualified detoxification” program which not only includes somatic detoxification but also individual and group psychotherapy, counseling for social and financial problems, and somatic medical care. All subjects met DSM-IV criteria for AD and were assessed using the German Versions of CIDI/DIA-X [Composite International Diagnostic Interview, Wittchen et al., 1998] in Mainz and Regensburg, or SSAGA [Bucholz et al., 1994; Hesselbrock et al., 1999] in Munich. Diagnosis of antisocial personality disorder (ASPD) was obtained in all samples using SCID II questionnaire and interview [German version: Wittchen et al., 1997].
Though different assessment instruments were employed because each ward had a specific measure in evaluating AD, all participating hospitals used the same DSM-IV diagnostic criteria. Alcohol-dependent subjects were further interviewed regarding any current or lifetime history of withdrawal symptoms, delirium tremens, or alcohol withdrawal-related seizures. Inpatients were further subgrouped according to Cloninger's type 1 (age of onset >25 years, no ASPD) or type 2 (age of onset <25 years, diagnosed with ASPD).
Furthermore, while no differences in gender (χ2 value: 0.87; P: 0.64) or age (F-value: 1.18; P: 0.31) was detected, a number of AD characteristics differed significantly across recruitment sites, including recent average daily alcohol intake (F-value: 4.61; P: 0.01) and number of DSM IV criteria endorsed (F-value: 39.27, P: <0.001), all of which were higher in subjects from the Regensburg hospital.
While each recruiting hospital enrolled alcohol-dependent subjects consecutively, subjects were excluded if they had any current axis I disorders, for example, schizophrenia, schizoaffective, bipolar disorder, dementia, and current suicidal behavior, since these patients were not admitted to open addiction treatment wards in all three hospitals. Alcohol-dependent subjects with current and lifetime major depression but without current suicidal behavior were included. Subjects incapable of informed consent were not enrolled into the study.
All assessments, with the exception of alcohol withdrawal at admission, were conducted approximately 2 weeks after detoxification from alcohol prior to patient's discharge. At this time, all subjects were still inpatients and free of any psychotropic medication. Characteristics of AD including DSM IV criteria, amount of daily alcohol intake, duration of AD, age at first drinking, or rates of specific DSM IV alcoholism criteria were assessed using the CIDI/DIA-X or the SSAGA.
All interviewers participated in an initial training using the CIDI, SSAGA, and SCID-II.
Informed written consent was obtained from patients and healthy controls after complete and extensive description of the study. The study was approved by the Ethics Committee of the Ludwig-Maximilians-University of Munich in agreement with the principles laid down in the Helsinki Declaration [1997]. All patients and healthy controls signed a written informed consent.
Genomic DNA was isolated from whole blood according to standard procedures.
As illustrated in Figure 1a, the HOMER 1 SNPs rs4132033, rs6871510, rs10039490, rs7708478, and rs6891537 were genotyped applying the TaqMan® technology (Assay-on-Demand) on an ABI7000 system (Applied Biosystems, Foster City, CA) with the following assay-IDs: rs4132033 (C_502666_10), rs6871510 (C_11646654_10), rs10039490 (C_29967781_10), rs7708478 (C_82423_20), rs6891537 (C_11650075_10). The standard PCR reaction was carried out using TaqMan® Universal PCR Master Mix reagent kit in a 10 µl volume according to the manufacture's instructions.
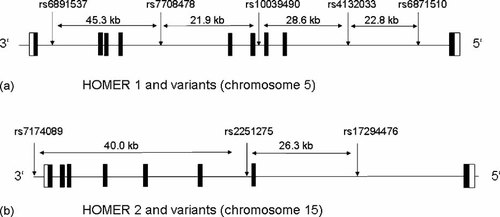
a: HOMER 1 and variants (chromosome 5). b: HOMER 2 and variants (chromosome 15).
As shown in Figure 1b, the SNPs rs2251275, rs7174089, and rs17294476 in the HOMER 2 gene were genotyped using the same approach with the following assay IDs: rs2251275 (C_1156475_10), rs7174089 (C_1156505_10), rs17294476 (C_1156462_10).
All laboratory procedures were carried out blind to case–control status. The “rs” number of the SNPs and the position of the amino acid exchange were taken from the SNP database (http://www.ncbi.nlm.nih.gov/SNP/).
Furthermore, all HOMER 1 and 2 SNPs were cross-checked with HAPMAP (http://www.hapmap.org) and PERLEGEN (http://genome.perlegen.com/) for genomic coverage. For both genes, tagging and non-tagging SNPs were chosen to include as much information across genes as possible. For the HOMER 1 gene, rs4132033, rs10039490, and rs7708478 SNPs and for the HOMER 2 gene, rs7174089 and rs17294476 SNPs are labeled as tagSNPs in HAPMAP or PERLEGEN databases.
All laboratory procedures were carried out with blinding to case–control status.
All continuous data were tested for normal distribution by Kolmogorov–Smirnov nonparametric tests. Hardy–Weinberg equilibrium (HWD) was analyzed for each genetic variant. As recently recommended by Wigginton et al. 2005, the HWD was verified using the exact test [Guo and Thompson, 1992].
To analyze the relationship between AD, controls and HOMER 1 and 2 genetic variants, chi-squared test, with Fisher's exact test, if necessary was employed. An alpha-error (P-value) of <0.05 (two-tailed) was considered as statistically significant. Data are presented as mean ± SD. Estimation of haplotype frequencies across groups and case–control haplotype analyses were conducted using “SNPALYZE” Software (Ver. 6.0.1., Dynacom Inc, 2007). LD between SNPs and estimation of haplotype frequencies across groups and case–control SNP and haplotype analyses were conducted using again “SNPALYZE” Software (Ver. 6.0.1., Dynacom Inc, 2007).
Statistical correction for multiple comparisons was conducted for the two genes (Bonferroni correction).
Using the “G*3-Power” Software [Faul et al., 2007], a priori sample size estimates revealed that with reported genotype frequencies of HOMER 1 rs5871510 SNP genotype frequencies [Dahl et al., 2005] (Cohen's ω: 0.1616, α-error of 0.05, power of 90% and df = 2), the required sample size was n = 485 (critical χ2 = 5.991) per group. For each of the nine SNPs analyzed, these requirements were exceeded.
Characteristics of alcohol-dependent individuals and control subjects are presented in Table I. Alcohol-dependent individuals differed significantly across centers regarding their daily alcohol intake before admission (highest in Regensburg, lowest in Mainz), histories of delirium tremens, alcohol withdrawal-induced seizures (lowest in Regensburg, highest in Mainz), and number of AD criteria endorsed (lowest in Munich, highest in Regensburg), while no differences were detected in rates of ASPD or type II alcoholism.
| Characteristics, mean ± SD or % | Munich | Mainz | Regensburg | Total sample (n = 2,039) | F- or χ2, signif. |
|---|---|---|---|---|---|
| Sex (M/F) | 348/102 | 194/56 | 1,026/313 | 1,568/471 | 0.28 |
| Age (years) | 43.21 ± 10.1 | 44.31 ± 9.9 | 43.20 ± 9.7 | 43.32 ± 9.8 | 1.28 |
| Age at onset (years) | 30.45 ± 9.5 | 31.28 ± 10.9 | 31.10 ± 10.6 | 30.45 ± 9.5 | 0.91 |
| Duration of dependence (years) | 13.11 ± 8.9 | 11.97 ± 13.9 | 11.86 ± 9.1 | 13.11 ± 8.9 | 3.05* |
| Average alcohol consumed (g/day) | 285.93 ± 175.2 | 207.30 ± 147.0 | 298.51 ± 148.7 | 281.64 ± 174.6 | 5.95** |
| Delirium in history % | 17.7 | 18.9 | 11.6 | 13.9 | 20.40*** |
| Epileptic seizures in history % | 18.5 | 34.3 | 15.9 | 17.8 | 29.30*** |
| # DSM IV criteria | 5.40 ± 1.5 | 5.60 ± 1.4 | 6.01 ± 1.3 | 5.84 ± 1.4 | 35.52*** |
| Tolerance % | 75.4 | 66.7 | 92.9 | 86.6 | 143.07*** |
| Withdrawal % | 73.1 | 86.5 | 81.7 | 80.0 | 24.17*** |
| Longer and more often % | 80.0 | 90.1 | 98.8 | 93.8 | 205.35*** |
| Tried to stop, continued % | 90.9 | 83.0 | 95.7 | 93.4 | 43.27*** |
| Great deal of time getting alcohol % | 60.3 | 76.0 | 62.6 | 63.4 | 14.32** |
| Given up important activities % | 69.7 | 60.2 | 81.9 | 77.3 | 58.00*** |
| Continued despite knowledge % | 80.0 | 97.7 | 90.9 | 89.1 | 51.66*** |
| Antisocial personality disorder (ASPD) % | 18.8 | 13.7 | 15.0 | 16.0 | 3.85 |
| Cloninger's type II % (early onset, ASPD+) | 13.1 | 10.7 | 11.3 | 12.0 | 0.59 |
| Controls | |||||
| Age (years) | 47.86 + 16.11 | ||||
| Sex M/F | 980/943 |
- * p < 0.05;
- ** p < 0.01;
- *** p < 0.001.
Twelve hundred sixteen of the inpatients could be identified as type 1 (59.6% of all alcohol-dependent individuals analyzed) and 245 subjects as Cloninger's type 2 subjects (12.0% of all alcohol-dependent individuals).
The genotype frequencies for all SNPs examined in both HOMER 1 and 2 genes did not significantly deviate from those predicted by the HWD, as presented in Table II.
| SNPs HOMER 1 and 2 | Genotype | Alcohol-dependent subjects % | Controls % | Allele | Alcohol-dependent subjects % | Controls % | HWE, cases (exact test) | HWE, controls (exact test) | Chi-squared value | P (exact test) | Odd ratio ES | 95% CI | Effect size (Cohen's ω for chi-squared) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [1,0]HOMER 1 rs4132033 | G/G | 30.8 | 30.9 | C | 45.0 | 43.9 | F = −0.02 | F = −0.02 | 0.92 | 0.34 | 1.04 | 0.96–1.14 | 0.008 |
| G/C | 48.5 | 50.3 | G | 55.0 | 56.1 | P = 0.38 | P = 0.44 | ||||||
| C/C | 20.7 | 18.8 | |||||||||||
| HOMER 1 rs6871510 | C/C | 55.3 | 54.9 | C | 74.1 | 74.0 | F = 0.004 | F = 0.02 | 0.002 | 0.96 | 1.00 | 0.91–1.11 | 0.008 |
| C/T | 37.6 | 38.3 | T | 25.9 | 26.0 | P = 0.86 | P = 0.36 | ||||||
| T/T | 7.1 | 6.8 | |||||||||||
| HOMER 1 rs10039490 | G/G | 59.9 | 59.3 | G | 77.3 | 77.1 | F = −0.007 | F = 0.01 | 0.062 | 0.81 | 1.01 | 0.91–1.13 | 0.009 |
| G/A | 34.7 | 35.6 | A | 22.7 | 22.9 | P = 0.73 | P = 0.65 | ||||||
| A/A | 5.4 | 5.1 | |||||||||||
| HOMER 1 rs7708478 | C/C | 46.3 | 46.4 | C | 67.8 | 67.7 | F = 0.03 | F = 0.02 | 0.006 | 0.94 | 1.00 | 0.91–1.10 | 0.007 |
| C/T | 43.0 | 42.5 | T | 32.2 | 32.3 | P = 0.19 | P = 0.51 | ||||||
| T/T | 10.7 | 11.1 | |||||||||||
| HOMER 1 rs6891537 | T/T | 78.3 | 77.8 | T | 88.5 | 88.0 | F = 0.005 | F = 0.04 | 0.44 | 0.53 | 1.05 | 0.91–1.20 | 0.018 |
| T/C | 20.3 | 20.4 | C | 11.5 | 12.0 | P = 0.83 | P = 0.11 | ||||||
| C/C | 1.4 | 1.8 | |||||||||||
| HOMER 2 rs2251275 | T/T | 32.4 | 33.0 | T | 57.3 | 57.4 | F = −0.02 | F = 0.003 | 0.004 | 0.98 | 0.99 | 0.91–1.09 | 0.011 |
| T/G | 49.8 | 48.8 | G | 42.7 | 42.6 | P = 0.40 | P = 0.91 | ||||||
| G/G | 17.8 | 18.3 | |||||||||||
| HOMER 2 rs7174089 | T/T | 25.0 | 27.2 | T | 50.1 | 52.1 | F = 0.004 | F = −0.005 | 3.17 | 0.08 | 0.92 | 0.85–1.01 | 0.028 |
| T/C | 50.2 | 49.7 | C | 49.9 | 47.9 | P = 0.85 | P = 0.83 | ||||||
| C/C | 24.8 | 23.1 | |||||||||||
| HOMER 2 rs17204476 | G/G | 68.4 | 68.8 | G | 82.6 | 83.0 | F = 0.009 | F = −0.009 | 0.21 | 0.78 | [2,0]0.97 | 0.87–1.10 | 0.012 |
| G/A | 28.4 | 28.4 | A | 17.4 | 17.0 | P = 0.69 | P = 0.68 | ||||||
| A/A | 3.2 | 2.8 |
- ω for chi-squared (0.10: small; 0.30: medium; 0.50: large), Cohen 1992.
The LD matrix (D′) between 5 HOMER 1 and 3 HOMER 2 SNPs are presented in Tables IIIa and IIIb. The LD was not very strong for all combinations of the HOMER 1 and 2 SNPs analyzed with D′ values ranging between 0.042 and 0.940 for HOMER 1 and 0.194 and 0.790 for HOMER 2 SNPs (Tables IIIc and IIId).
| HOMER 1 rs4132033 | HOMER 1 rs6871510 | HOMER 1 rs10039490 | HOMER 1 rs7708478 | |
|---|---|---|---|---|
| HOMER 1 rs6871510 | 0.894 | |||
| HOMER 1 rs10039490 | 0.697 | 0.596 | ||
| HOMER 1 rs7708478 | 0.678 | 0.568 | 0.960 | |
| HOMER 1 rs6891537 | 0.541 | −0.002 | −1 | 0.756 |
| HOMER 1 rs4132033 | HOMER 1 rs6871510 | HOMER 1 rs10039490 | HOMER 1 rs7708478 | |
|---|---|---|---|---|
| HOMER 1 rs6871510 | 0.880 | |||
| HOMER 1 rs10039490 | 0.648 | 0.544 | ||
| HOMER 1 rs7708478 | 0.662 | 0.577 | 0.940 | |
| HOMER 1 rs6891537 | 0.545 | 0.042 | −0.820 | 0.691 |
| HOMER 2 rs2251275 | HOMER 2 rs7174089 | |
|---|---|---|
| HOMER 2 rs7174089 | 0.149 | |
| HOMER 2 rs17204476 | 0.573 | −0.720 |
| HOMER 2 rs2251275 | HOMER 2 rs7174089 | |
|---|---|---|
| HOMER 2 rs7174089 | 0.152 | |
| HOMER 2 rs17204476 | 0.597 | −0.691 |
As also shown in Table II, all SNPs of HOMER 1 and 2 did not significantly differ between alcohol-dependent individuals and controls, except HOMER 2 rs7174089, which had a slightly higher frequency of the T-allele in control subjects. However, after correcting the α-error for multiple testing, the result did not remain significant anymore.
Haplotype analysis between groups, as presented in Tables IVa and IVb, did not reveal any significant differences in HOMER 1 haplotypes between groups. One haplotype (comprising rs2251275, rs7174089, rs17294476) of the HOMER 2 gene (G–T–G) was more often detected in the control group (alcohol-dependent individuals: 5.03%, control subjects: 6.38%). However, the result did no remain significant after statistical correction for multiple testing. Testing associations between Homer SNPs and haplotypes with alcohol withdrawal, delirium tremens, alcohol withdrawal-related seizures, or Cloninger's type 1 or 2 individuals did not yield significant results, after correcting for multiple testing.
| Haplotypes | Overall % | Alcohol-dependent subjects % | Controls % | Chi-squared | P-value | Permutation P | ES |
|---|---|---|---|---|---|---|---|
| G–C–G–C–T | 46.33 | 46.36 | 4.63 | 0.006 | 0.94 | 0.93 | |
| C–T–A–T–T | 14.82 | 15.17 | 14.48 | 0.79 | 0.37 | 0.40 | |
| C–C–G–C–T | 11.46 | 11.68 | 11.21 | 0.43 | 0.51 | 0.54 | |
| C–T–G–C–T | 5.37 | 5.51 | 5.19 | 0.45 | 0.50 | 0.55 | |
| G–C–A–T–T | 3.98 | 3.83 | 4.17 | 0.64 | 0.42 | 0.45 | |
| C–T–G–T–C | 3.16 | 2.96 | 3.38 | 1.24 | 0.26 | 0.36 |
| Select locus | Chi squared | P-value | Permutation P | Upper | Done |
|---|---|---|---|---|---|
| Overall statistics | |||||
| Haplotype: rs6871510, rs4132033, rs10039490, rs7708478, rs6891537 | 40.71 | 0.025 | 0.6 | 663 | 1,000 |
| Haplotypes | Overall % | Alcohol-dependent subjects % | Controls % | Chi-squared | P-value | Permutation P | ES |
|---|---|---|---|---|---|---|---|
| T–T–G | 30.67 | 30.32 | 31.08 | 0.58 | 0.44 | 0.46 | |
| G–C–G | 23.87 | 24.57 | 23.16 | 2.32 | 0.12 | 0.16 | |
| T–C–G | 22.58 | 22.71 | 22.39 | 0.12 | 0.72 | 0.74 | |
| G–T–A | 12.61 | 12.84 | 12.37 | 0.45 | 0.50 | 0.54 | |
| G–T–G | 5.71 | 5.03 | 6.38 | 7.28 | 0.007 | 0.03* | 0.03 |
| Select locus | Chi-squared | P-value | Permutation P | Upper | Done |
|---|---|---|---|---|---|
| Overall statistics | |||||
| Haplotype: rs17204476, rs2251275, rsS7174089 | 25.25 | 0.0007 | 0.03 | 30 | 1,000 |
- ω for chi-squared (0.10: small; 0.30: medium; 0.50: large), Cohen 1992.
- * Did not remain significant after Bonferroni correction.
The aim of this study was to perform an association study of HOMER 1 and 2 genetic variants in AD, performing single SNP, haplotype, and LD analysis in a sufficiently large sample of approximately 2,000 alcohol-dependent individuals and control subjects.
Single SNP analysis revealed no significant association of HOMER 1 and 2 genetic variants with AD. Since the investigated SNPs are common in the general population, the genetic background of AD may be better represented when haplotypes are considered. Initial results of HOMER 2 3SNP haplotype analysis indicated a significant association of a rare haplotype with AD, which did not remain significant after correcting for multiple testing.
In addition, AD-related phenotypes, like current or lifetime history of withdrawal, delirium tremens, or alcohol withdrawal-related seizures were not related to both HOMER 1 and 2 SNPs and haplotypes which does not support a major role of HOMER variants in the aetiology of AD-related phenotypes, including early onset and antisocial alcoholism.
The 5 SNPs of HOMER 1 are, at most, in low-to-moderate LD in both alcohol-dependent individuals and controls which may have impaired the haplotype analyses. However, in both groups, 3 major and 5 SNP haplotypes account for 72.9% of all haplotypes in the total sample (alcohol-dependent subjects: 73.5%; controls: 72.3%), despite the low LD between several SNPs. In HOMER 2, all SNPs are also in low-to-moderate LD. The four major HOMER 2 and 3 SNP haplotypes account for 89.7% of all possible marker combinations (alcohol-dependent individuals: 90.4%; controls: 89.0%). For this study, several tagSNPs (from HAPMAP and Perlegen) were used for genotyping to increase optimal information on variants across genes.
To estimate LD between pairs of SNPs, Lewontin's D′ was employed [Lewontin, 1988] and has been suggested to be reasonably robust towards differences in allele frequencies in contrast to D [Thompson et al., 1988]. The LD matrix of HOMER 1 and 2 SNPs is fairly identical in both alcohol-dependent individuals and controls.
Compared to a previous association study in cocaine-dependent individuals which reported an association of a HOMER 1 SNP [Dahl et al., 2005], the current study did not detect an association with this and other HOMER 1 and 2 gene variants with AD. Indicated by several lines of evidence [reviewed by Szumlinski et al., 2008], there is a potential role of the HOMER protein family in the development and course of alcohol and substance dependence. However, this influence may not be exerted by HOMER 1 and 2 genetic variants.